Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Treatment of Hirschsprung disease (HD) consists principally of resection of the aganglionic bowel with preservation of the anal sphincter complex. Several operative techniques have emerged over the past 50 years. The proposed advantage of the Duhamel side-to-side anastomosis is the avoidance of dissection of the anterior and lateral part of the distal rectum, preserving the nerve fibers to the adjacent bladder. In the open approach, the Duhamel procedure is a fairly straightforward operation and is known for its good results. Laparoscopically, the procedure is more difficult because it requires intracorporeal suturing of the rectal stump. To date, results with the laparoscopic approach seem promising. This chapter describes our laparoscopic Duhamel technique and documents our results.
Indications for the laparoscopic Duhamel procedure do not differ from those for the open operation. The diagnosis of HD is determined by rectal suction biopsies. In unclear cases, full-thickness rectal biopsies may be needed, although the biopsy site can interfere with the future location of the side-to-side anastomosis. Alternatively, anorectal manometry can give additional information that is helpful in making the diagnosis of HD. Generally, when a child is referred with suspected HD, rectal washouts (10 to 20 mL/kg each time) are initiated until clear effluent is returned and the abdominal distention has resolved. Parents are then taught to perform the daily rectal washouts at home until the child is admitted for the Duhamel procedure. We prefer to admit our infants and children the day before the operation for further rectal washout.
The infant or child is placed supine on the operating table. Infants are placed transversely at the lower end of a short operating table to allow the surgeon to stand comfortably above the patient’s head. Armrests covered with gel pads on one or both sides of the table allow older children to be positioned similarly. Endotracheal anesthesia is supported by epidural regional anesthesia. Before the procedure, the cleanliness of the rectosigmoid colon is checked by a final rectal washout on the operating table. The patient is prepped from the costal margin down to the lower legs. The legs are covered with separate drapes so they can be moved during the perineal phase of the procedure. The children receive intravenous antibiotics preoperatively and for 24 hours postoperatively. A urinary catheter is inserted after the patient has been draped.
The first 5.5-mm port is placed in the subumbilical fold by a cutdown technique and secured to the fascia with a 2-0 Vicryl (Ethicon Inc., Somerville, NJ) suture. (By tying this suture at the end of the procedure, this subumbilical facial defect is closed.) The 5-mm telescope is then inserted through this cannula. A 3.5- or 5.5-mm port is then introduced in the right lower abdomen under direct vision. A second cannula is then positioned in the right upper quadrant, also for instrumentation. A third port is inserted in the left lower abdomen (LLQ) for introduction of a grasping forceps to elevate and manipulate the bowel. The surgeon and surgical assistant/camera holder stand above the head of the patient.
The operation is started by taking biopsies of the colon for frozen section analysis for ganglion cells ( Fig. 15-1 ). The first biopsy is taken at the visual transition zone, and a second one more proximal in normal-appearing colon. Care is taken to avoid mucosal entry. Vicryl sutures are used to close the biopsy sites. It is advantageous to leave the most proximal suture a little long to mark the site for the subsequent coloanal anastomosis.
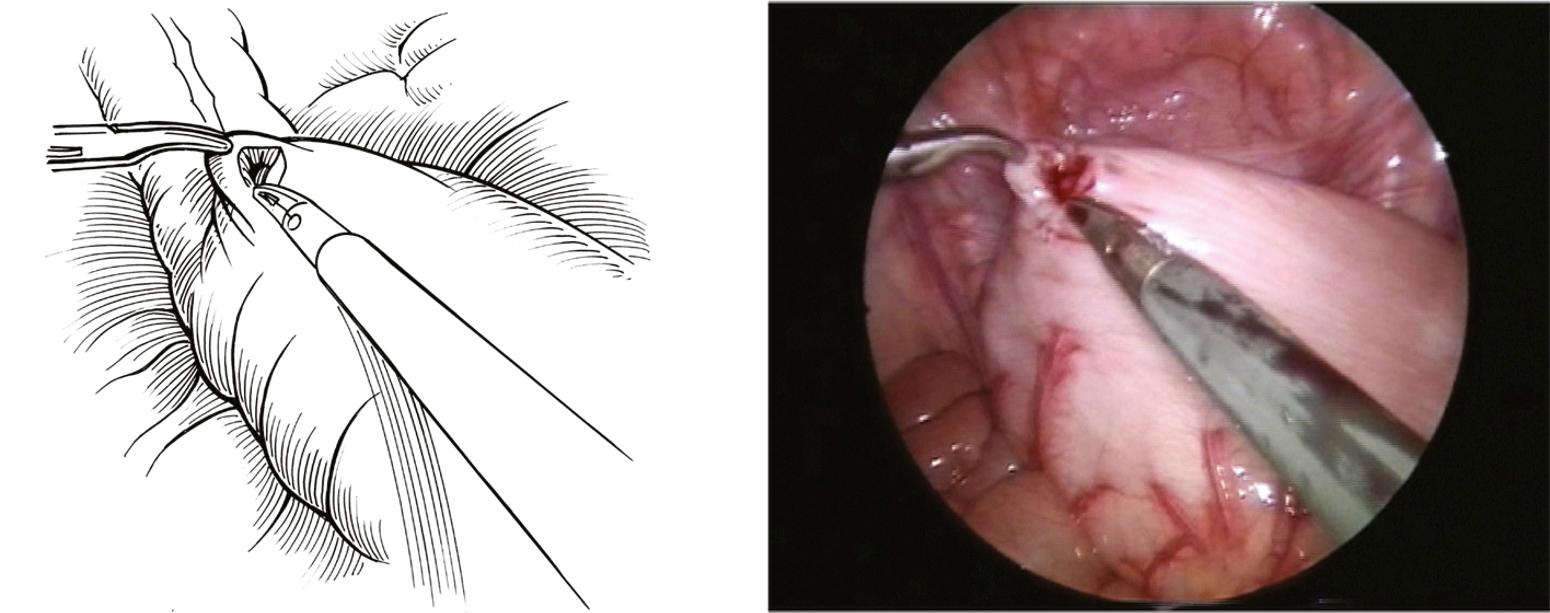
Using monopolar cautery, dissection of the aganglionic colon is started on the medial side close to the bowel wall at the level of the rectum by incising the peritoneal attachment and cauterizing the small vessels. When a sufficient mesenteric window has been created, dissection is moved to the patient’s left side, first cauterizing the vessels close to the bowel wall and then opening the peritoneum on the lateral side of the distal colon. In older children, an ultrasonic scalpel can be used to dissect further down the pelvis. At all times, notice should be taken of the location of both ureters and, in boys, the ducti deferentes, which may lie close to this dissection. At the peritoneal reflection in the pelvis, the peritoneum is opened anteriorly to allow more traction on the distal rectum. To preserve nerve fibers running to the bladder, the peritoneum is not extensively dissected inferiorly. Dissection is continued dorsally and laterally to the median hemorrhoidal vessels. The retrorectal space is then opened to facilitate the pull-through of the mobilized bowel ( Fig. 15-2 ). When the retrorectal space has been sufficiently enlarged, the grasping forceps can be palpated from the perineum at the level of the dentate line.
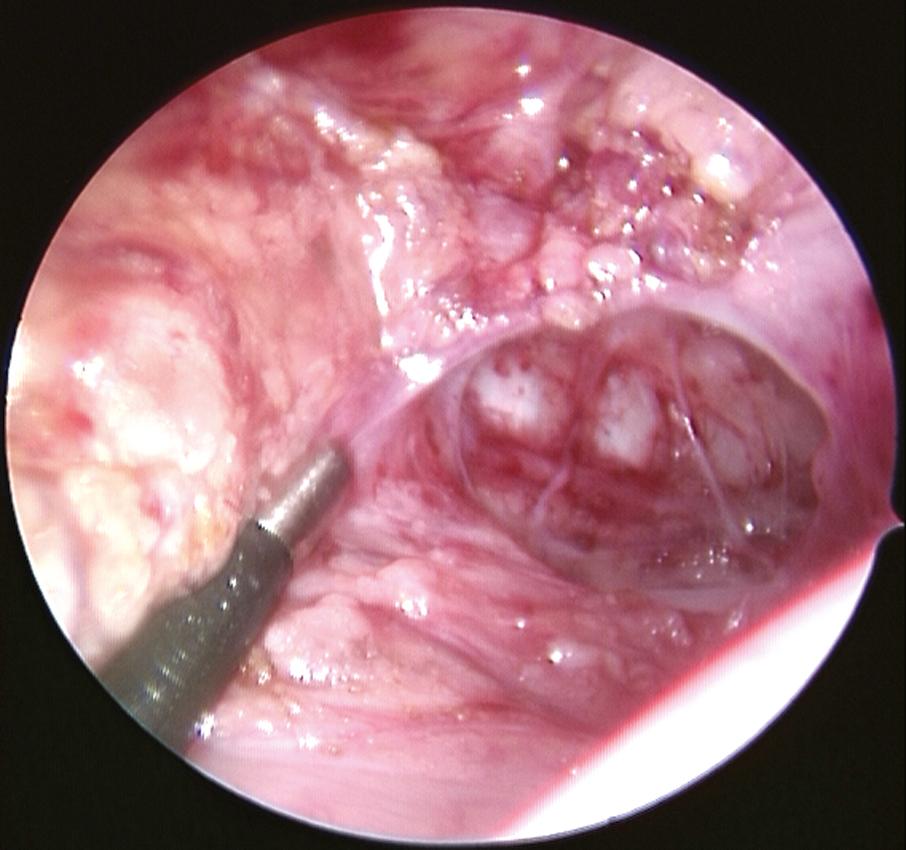
Dissection is then turned upward in the direction of the most proximal biopsy that is positive for ganglion cells, again staying close to the bowel wall. When the mobilization needs to extend higher to the splenic flexure and beyond, the middle colic vessels should be ligated and divided near the aorta. If the aganglionosis extends to the hepatic flexure, the surgeon should consider using the ileocolic artery for the vascular supply to the pull-through colon.
After the colon has been mobilized, a 2-0 Vicryl ligature is placed around the rectum, approximately 3 cm proximal to the peritoneal reflection. A suction device is introduced transanally and the rectum further cleansed. The rectum is elevated with a grasping forceps that has been inserted through the LLQ port. While elevating the rectum, the rectum is sharply transected approximately 2 cm above the peritoneal reflection ( Fig. 15-3 ). In dividing the rectum, first the anterior wall is incised, after which the grasping forceps is used to grasp the anterior wall of the rectum to avoid retraction of the stump. Once the anterior wall of the rectal portion is grasped, the posterior aspect of the rectal wall is incised. A grasping forceps is then introduced through the right midabdominal cannula and positioned in the retrorectal space just proximal to the dentate line.
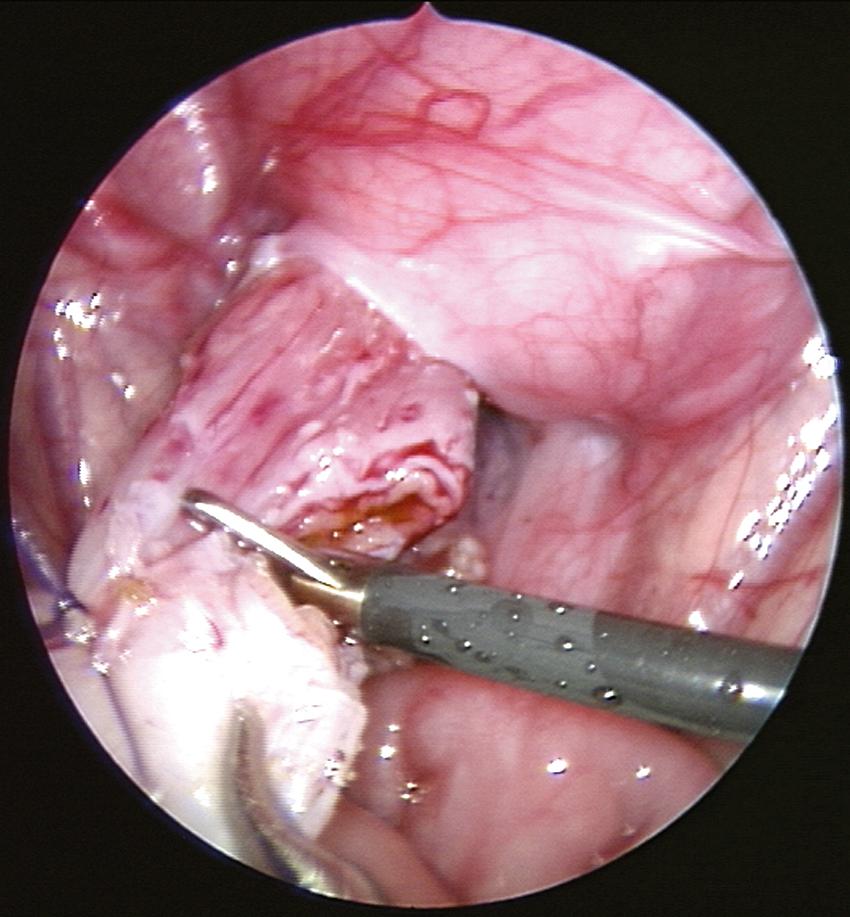
The legs of the patients are lifted and two small retracting hooks are carefully introduced into the anus. By pushing down on the grasping forceps that is positioned in the retrorectal space, the correct location for the incision in the posterior wall of the rectum just above the dentate line can be determined. An incision in the posterior aspect of the rectum is made 0.5 cm above the dentate line using a knife or diathermia tip right over the grasping forceps. The grasping forceps can then be exteriorized through this incision in the posterior anus. Two 4-0 Vicryl sutures are placed full thickness through the anterior proximal side of the incision for the future coloanal anastomosis. This incision in the native rectum is then extended laterally to each corner, parallel to the dentate line, where two additional corner sutures are positioned. Finally, a suture is placed on the anterior edge of this incision in the posterior native rectum in the midline. The protruding grasping forceps is then secured with an atraumatic clamp and both are returned to the abdominal cavity. After readjusting the camera, the clamp can be seen on the inside, and the transected pull-through rectum or colon can be secured into the atraumatic clamp.
With the grasping forceps that was inserted through the LLQ port, the anterior wall of the rectal stump can be secured and lifted up to avoid the stump being drawn deep into the pelvis. Under direct vision and with the guidance of the grasping forceps through the right midabdominal port, the atraumatic clamp containing the mobilized colon can be exteriorized to the point where the most proximal biopsy was taken ( Fig. 15-4 ). Care is taken so that the pulled-through colon is not twisted and lies with its antimesenteric surface facing anteriorly. The adequacy of the blood supply to the pull-through colon is then assessed, especially in the more extended resections. Also, the small bowel should be withdrawn from underneath the pulled-through bowel.

Once the ganglionic bowel has been pulled through the incision in the posterior native rectum, the anterior surface of the pull-through colon just proximal to the biopsy site is transected and anastomosed using the two sutures previously placed on the ventral side of the posterior incision in the native rectum. The sutures are left long for traction when the endoscopic stapler device is used later. The incision in the pulled-through bowel is then extended laterally. The lateral corners of the ganglionic pull-through are anastomosed to the corners of the native rectum, and these sutures are also left long for traction. The pull-through colon is then transected completely and the posterior suture line is created. (This coloanal anastomosis is the same as in the open Duhamel technique.) Alternatively, an eversion technique can be used with external resection of the aganglionic bowel, followed by the coloanal anastomosis.
By pulling on the previously mentioned two ventrally placed sutures, which now have anastomosed the pull-through colon and native rectum, the lumens of the rectum and the pulled-through colon can be visualized. A 45-mm EndoGIA (Ethicon Endosurgery, Cincinnati, OH) stapler is then introduced, with one arm in each opening between these two sutures ( Fig. 15-5 ). From inside the abdomen, the correct position of the EndoGIA can be confirmed ( Fig. 15-6 ). By pushing the handle once, the correct position of the stapler for firing can be checked a final time. If the surgeon is not satisfied with the position of the stapler, the device can be opened and repositioned. Once the surgeon is satisfied with the stapler position, the stapler is fired, thus creating the side-to-side anastomosis. After checking that the device was fired completely, the handle on the side of the stapler is retracted and the device is withdrawn carefully. Sometimes, a second loading is necessary to complete and/or lengthen this anastomosis.

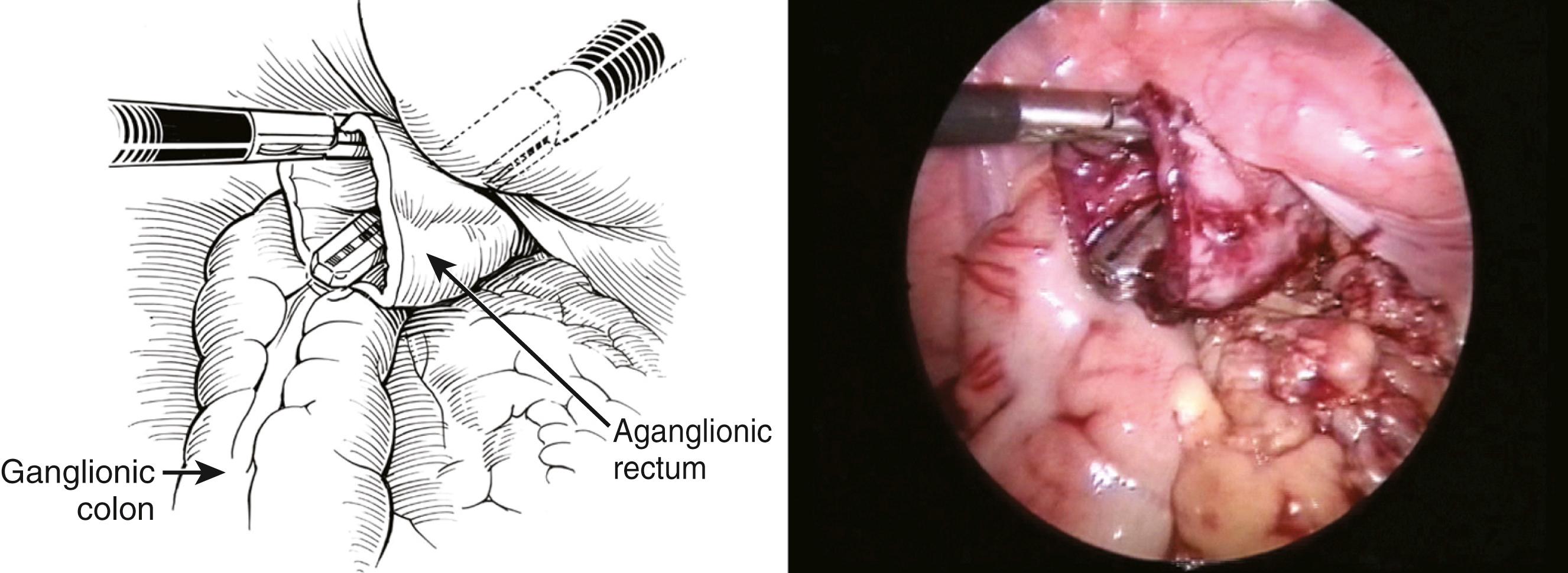
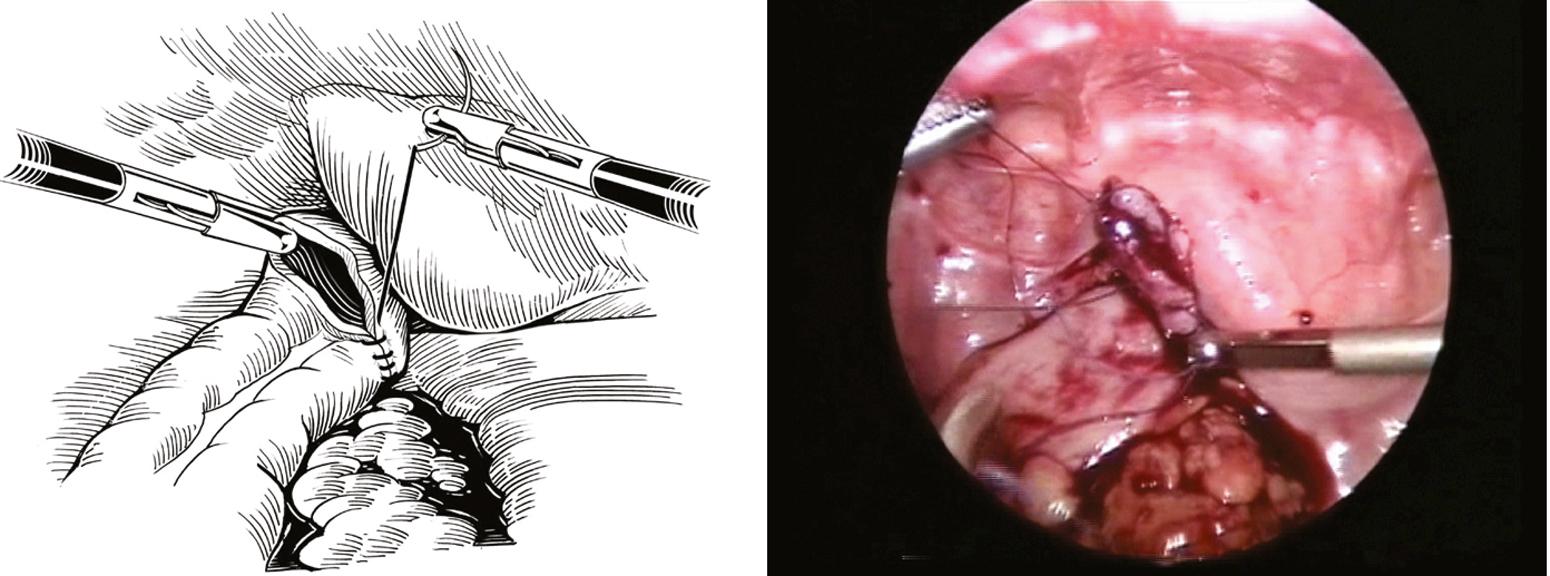
The final part of the operation is intra-abdominal closure of the rectal stump using intracorporeal suturing ( Fig. 15-7 ). If the side-to-side colorectal anastomosis has been extended sufficiently far enough cephalad, the rectal stump can be closed without leaving a blind cuff. A 4-0 Vicryl running suture is used, starting from the superior part of the rectal stump and coming down to the side-to-side anastomosis. If necessary, a second suture can be used running upward, and the two sutures can be tied, completing the closure.
If deemed necessary, a transrectal, transanastomotic siliconized drain can be introduced under direct vision and left for colonic decompression for a few days postoperatively. Under direct vision, the ports are removed and the fascial defects are all closed using 4-0 Vicryl. The skin is approximated with sterile strips.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here