Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Appendicitis is the most common pediatric surgical emergency, with nearly 82,000 appendectomies performed in children each year. There has been widespread adoption of laparoscopy by pediatric surgeons, though there is significant variation in techniques, ranging from a single-incision approach to the traditional three-port technique.
A child typically presents with nonspecific abdominal pain that localizes to the right lower quadrant (RLQ) of the abdomen over a 24- to 48-hour period. Pain is often accompanied by some or all of the following symptoms: fever, anorexia, a desire to remain still, nausea, vomiting, diarrhea, and dysuria. However, disease presentation may be nonspecific in younger children and toddlers, with the refusal to ambulate being the primary symptom.
The patient’s history, physical exam, and laboratory findings are used by several scoring systems to determine the likelihood of appendicitis. Although the Alvarado score (based on migration of pain, anorexia, nausea, RLQ tenderness, rebound pain, fever, leukocytosis, and left shift) has been validated in adult patients, it tends to overpredict appendicitis in intermediate- and high-risk children. The Pediatric Appendicitis Score (based on RLQ tenderness with coughing, percussion, or hopping; anorexia; fever; nausea or vomiting; right iliac fossa tenderness; leukocytosis; neutrophilia; and migration of pain) is more reliable in this patient population, with a positive predictive value of 0.96 and a negative predictive value of 0.99 in one study.
Although scoring systems can be helpful, particularly in resource-limited areas, imaging is typically obtained to confirm the diagnosis. Ultrasound (US) and computed tomography (CT) are the most common imaging modalities. The obvious benefit of the former is the avoidance of radiation associated with CT, but the imaging results are more operator dependent with US. However, the creation of regimented US scoring systems has increased the diagnostic accuracy of US to 97%, resulting in the need for fewer CT scans.
With the development of emergency room magnetic resonance imaging (MRI) protocols for patients with suspected appendicitis, there is an increasing use of this imaging modality, particularly for pediatric patients in whom radiation should be avoided whenever possible. The sensitivity and specificity of MRI for appendicitis (97.6% and 97.0%, respectively) are comparable to that of CT.
Patients with uncomplicated appendicitis can typically be resuscitated and treated with antibiotics prior to appendectomy. If admitted overnight, the operation can be safely delayed until the next morning without an increased risk of complicated (i.e., gangrenous or perforated) appendicitis or surgical site infections (SSIs). In cases of complicated appendicitis, management options include treatment with antibiotics, percutaneous abscess drainage, and appendectomy at the time of presentation or after a 6- to 8-week interval. A prospective randomized trial comparing initial laparoscopic appendectomy with initial nonoperative management and interval appendectomy showed a trend toward slightly longer operating times in the former but no difference in terms of total length of hospitalization, recurrent abscess rates, or overall hospital charges.
Studies to define the optimal management of complicated appendicitis have been somewhat hampered by varying definitions of what “complicated” actually means. A retrospective review of more than 5000 patients found that the “presence of a visible hole, diffuse fibrinopurulent exudate, intra-abdominal abscess, and extraluminal fecalith” were all associated with worse outcomes and should serve as criteria for defining complicated appendicitis.
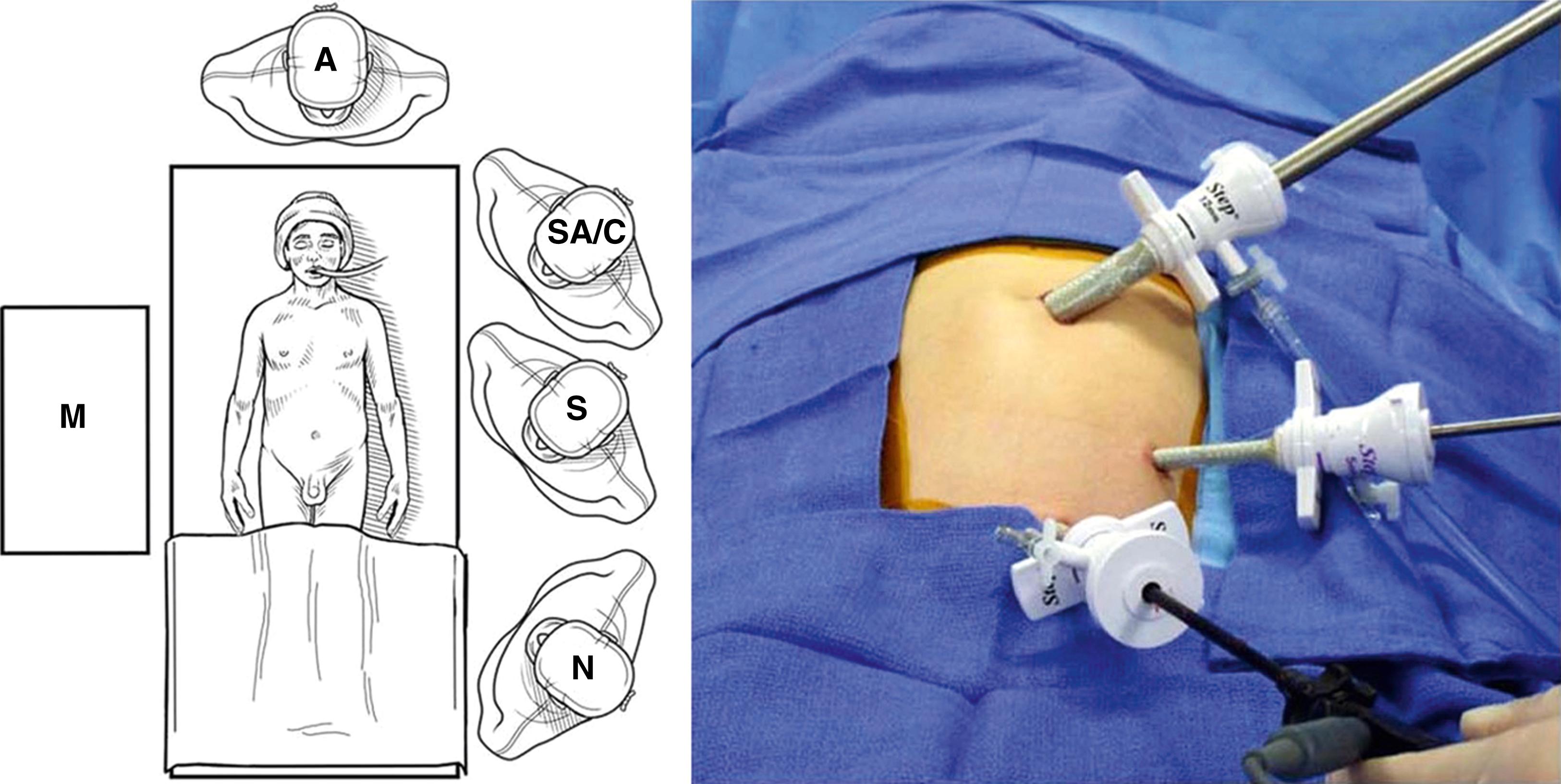
The patient is placed supine for induction of general anesthesia and endotracheal intubation. If the patient has not voided prior to entering the operating room, a Credé maneuver should be performed or urinary catheter inserted to decompress the bladder. Both arms are tucked at the sides. If unable to tuck both arms, the left arm is preferentially tucked to allow for both the surgeon and surgical assistant to stand on the left. The abdomen is prepped and draped. Appropriate antibiotics are administered prior to incision. The antibiotics used vary depending on the patient’s allergies and the preferences of the surgeon’s institution. (At our institution, patients without allergies receive both ceftriaxone and metronidazole, dosed once every 24 hours.) An incision is made in the umbilicus and a Veress needle is used to insufflate the peritoneal cavity to 15 mm Hg. At this point, the surgeon can decide to perform a three-port or a single-incision laparoscopic appendectomy.
A 10- to 12-mm Step cannula (Medtronic, Minneapolis, MN) is inserted through the umbilical incision, followed by a 5-mm 30-degree laparoscope. Two additional 5-mm ports are then introduced under visualization: one in the left lower quadrant (LLQ) and one in the suprapubic region ( Fig. 10-1 ). The table position can be adjusted to aid in visualization of the appendix (e.g., right side up and Trendelenburg). If present, fluid can be suctioned from the pelvis, paracolic gutter, and perihepatic space. Although there is general agreement that any murky fluid should be aspirated, there appears to be no benefit to widespread irrigation in cases of perforated appendicitis.
Adhesions between the appendix and omentum or small bowel are taken down bluntly with sweeping motions, rather than with direct grasping maneuvers. If the appendix is to be grasped, gentle use of Babcock graspers on a healthy, intact portion of the appendix or on the mesoappendix will reduce the risk of rupture and spillage. After mobilizing the appendix, the base should be exposed and a window created in the adjacent mesoappendix ( Fig. 10-2A ). At this point, the appendix and mesoappendix can be controlled with hook cautery and ligating loop suture, or with a stapler.
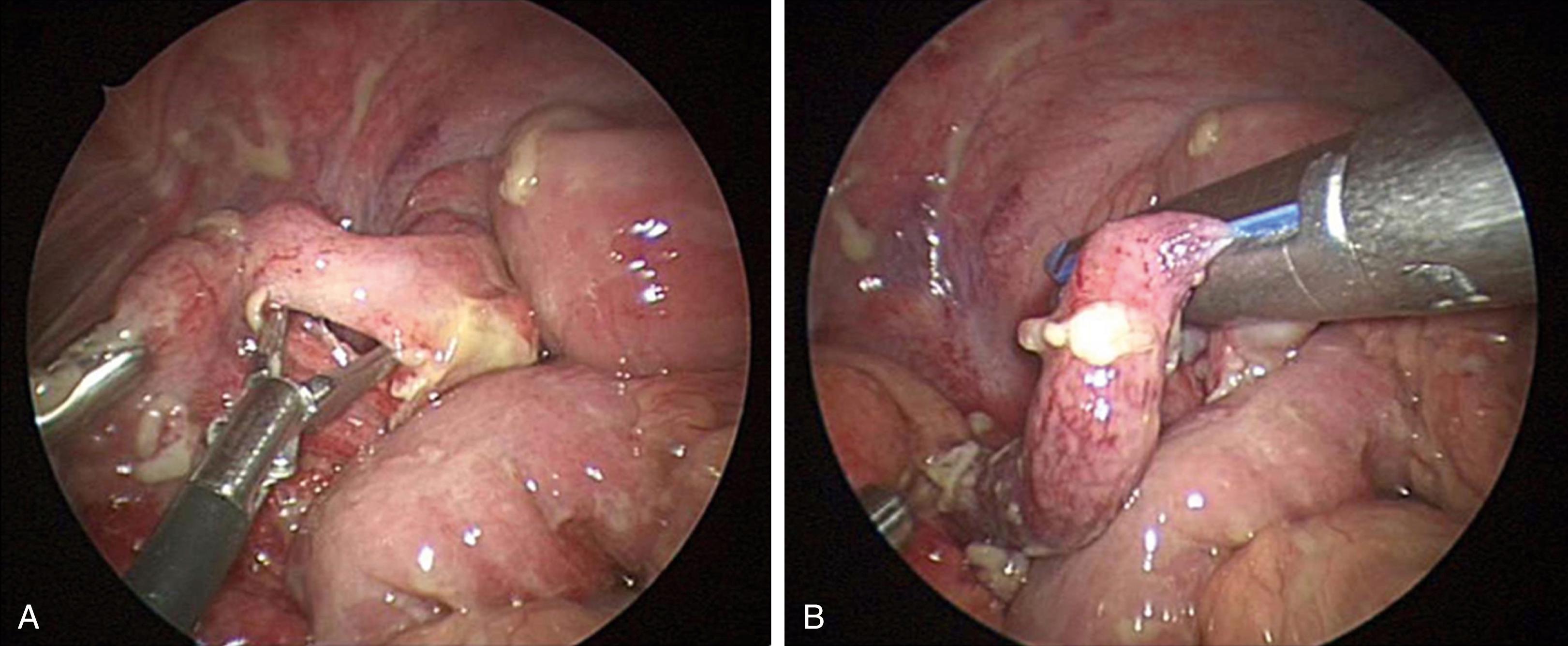
Depending on stapler availability, the 5-mm and 10-mm ports can accommodate the 5-mm stapler (Bolder Surgical, Louisville, CO), but the umbilical port must be upsized to a 12-mm port if a 10-mm stapler is used. The laparoscope should be reinserted via the LLQ port for visualization if the stapler is introduced via the umbilical cannula. The stapler is opened and manipulated across the appendix ( Fig. 10-2B ) or mesoappendix, depending on which seems best to ligate/divide first. After closing the jaws, the field should be thoroughly examined to ensure that no other structures are inadvertently included within the instrument prior to firing the stapler. (It is important to note the type of stapler load being used, as the 10-mm stapler has staples that are bowel or vascular specific.) If the mesoappendix was ligated and divided first, the stapler is then positioned across the appendix and fired.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here