Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Access the accompanying videos for this chapter online. Available on ExpertConsult.com .
Achalasia is a rare disorder of esophageal dysmotility in which there is absent or incomplete relaxation of the lower esophageal sphincter (LES) in addition to generalized abnormal peristalsis of the esophageal body. The pathophysiologic basis of achalasia is thought to be related to the degeneration of the inhibitory myenteric nerve plexus of the LES and esophageal body. The incidence in adults is 1 per 100,000, but it is much less in children, estimated to be 0.1 per 100,000. Although the prevalence of achalasia is 80 per million, only 5% of achalasia patients are diagnosed at younger than 15 years of age.
Idiopathic disease predominates, but achalasia has been associated with Chagas disease, trisomy 21, eosinophilic esophagitis, familial dysautonomia, congenital hypoventilation syndrome, and alacrima, achalasia, and adrenocorticotropic hormone (ACTH) insensitivity (AAA) syndrome. Various nonsurgical therapies for achalasia have been utilized over the years but have largely produced only temporary results and/or required repeated interventions. These include medical therapies such as calcium channel blockers, sildenafil, and isosorbide dinitrate, and endoscopic treatments including pneumatic balloon dilation, esophageal stenting, and botulinum toxin (Botox) injection into the LES.
Definitive surgical management of achalasia has evolved over time to less invasive approaches. The two primary techniques utilized today are the laparoscopic esophagomyotomy (LEM) (with or without partial fundoplication) and the peroral endoscopic myotomy (POEM) procedure.
Indications for operation include ineffective treatment results from alternatives to surgical myotomy such as esophageal dilation, LES Botox injection, or pharmacologic therapies. Preoperative studies documenting the diagnosis of achalasia should include an esophagram demonstrating a dilated proximal esophagus and “bird beak” tapering at the esophagogastric junction (EGJ) ( Fig. 3-1 ), an esophagogastroduodenoscopy (EGD) with or without pH-metry study to evaluate for gastroesophageal reflux or stricture, and esophageal manometry to document nonperistaltic esophageal body contractions and failure of LES relaxation after swallowing.

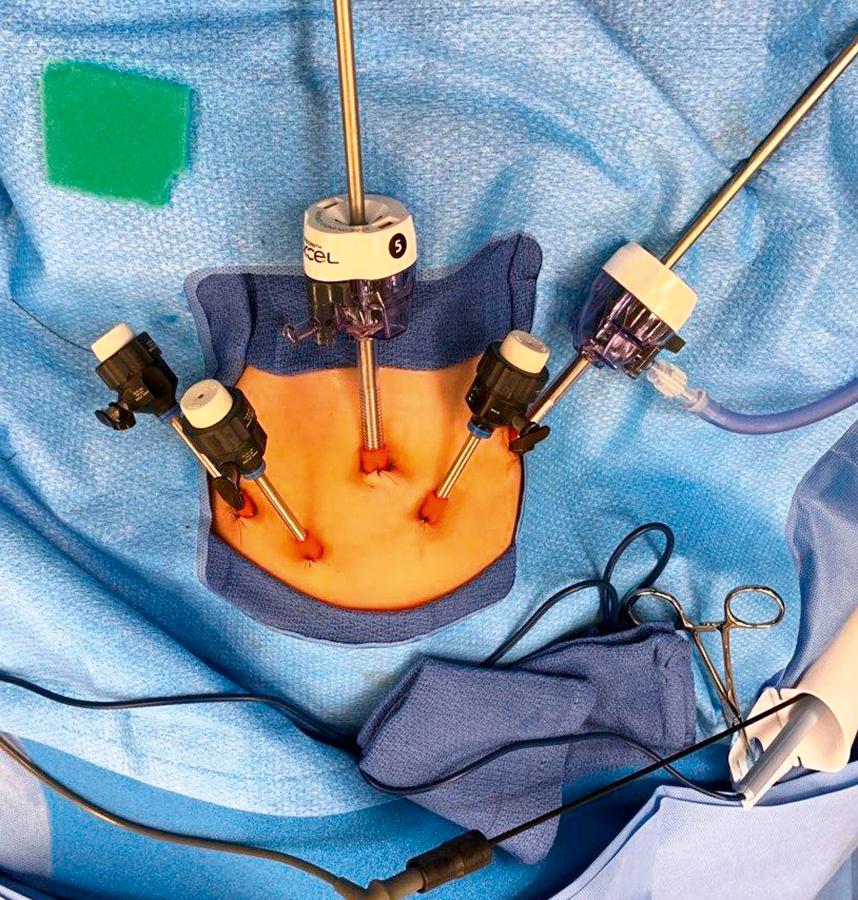
The patient is positioned supine on the operating table with legs straight (older patients) or frog-legged at the end of the operating table (children < 5 years of age) with the table rotated into a reverse Trendelenburg position. The surgeon can stand on the patient’s right or left side with the assistant on the opposite side. The monitor will be situated at the head of the bed. Five ports are used (as for laparoscopic fundoplication) and range from 3.5 mm to 10 mm size depending on the size of the patient ( Fig. 3-2 ). Our preferred access is via a vertical umbilical incision using an open cutdown technique. After the initial umbilical port is inserted, we confirm its intra-abdominal positioning before initiating CO 2 insufflation.
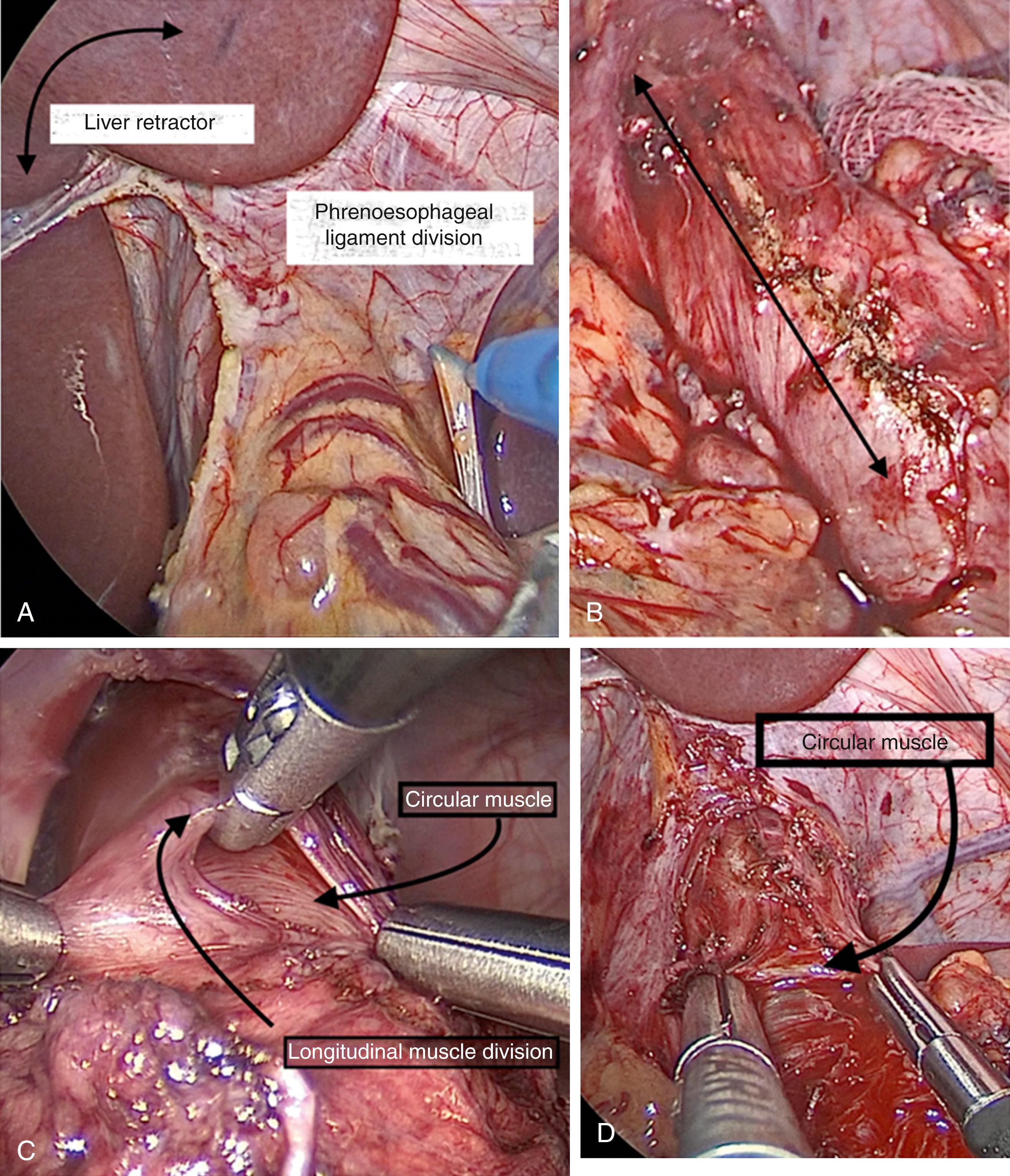
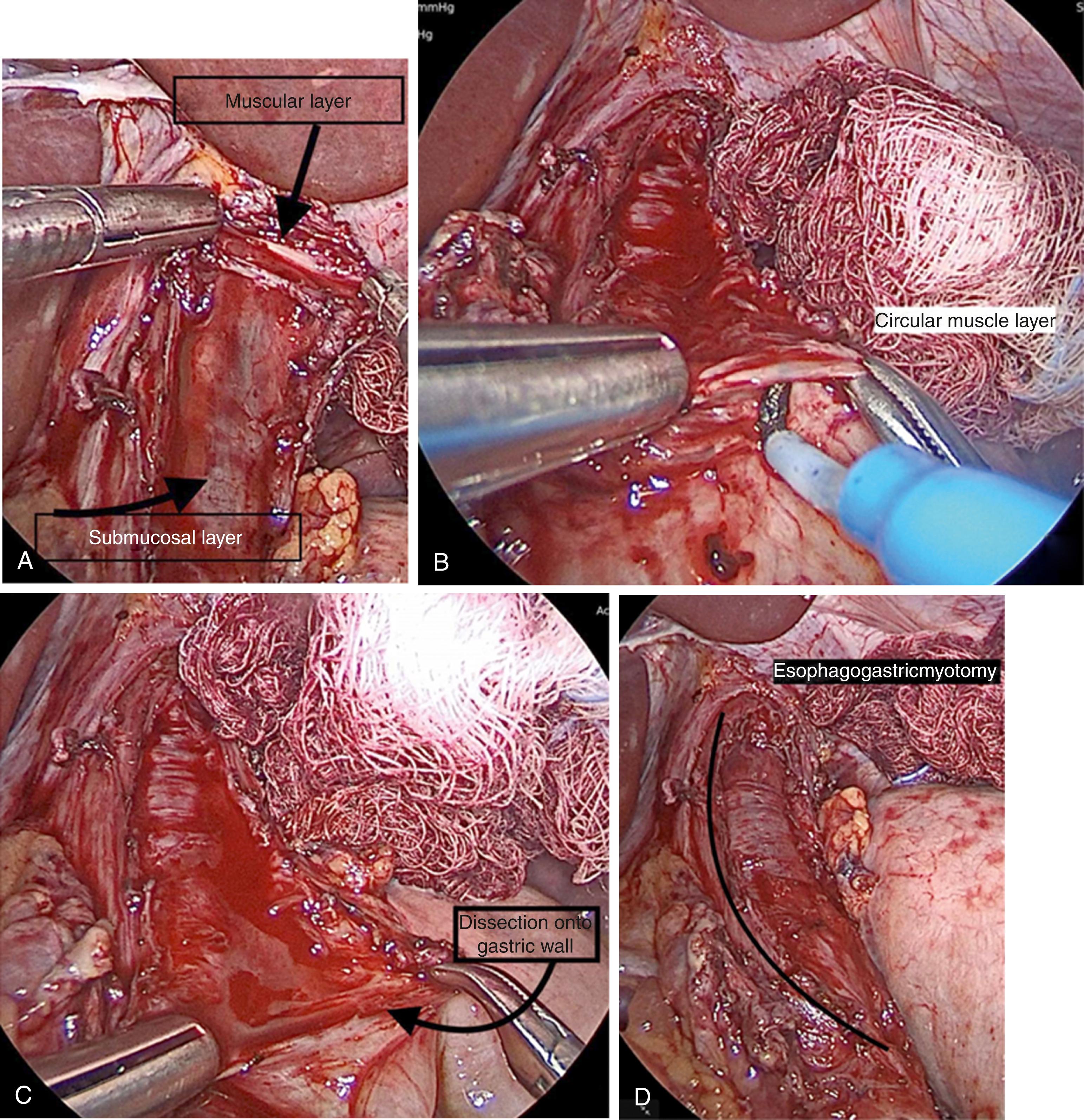
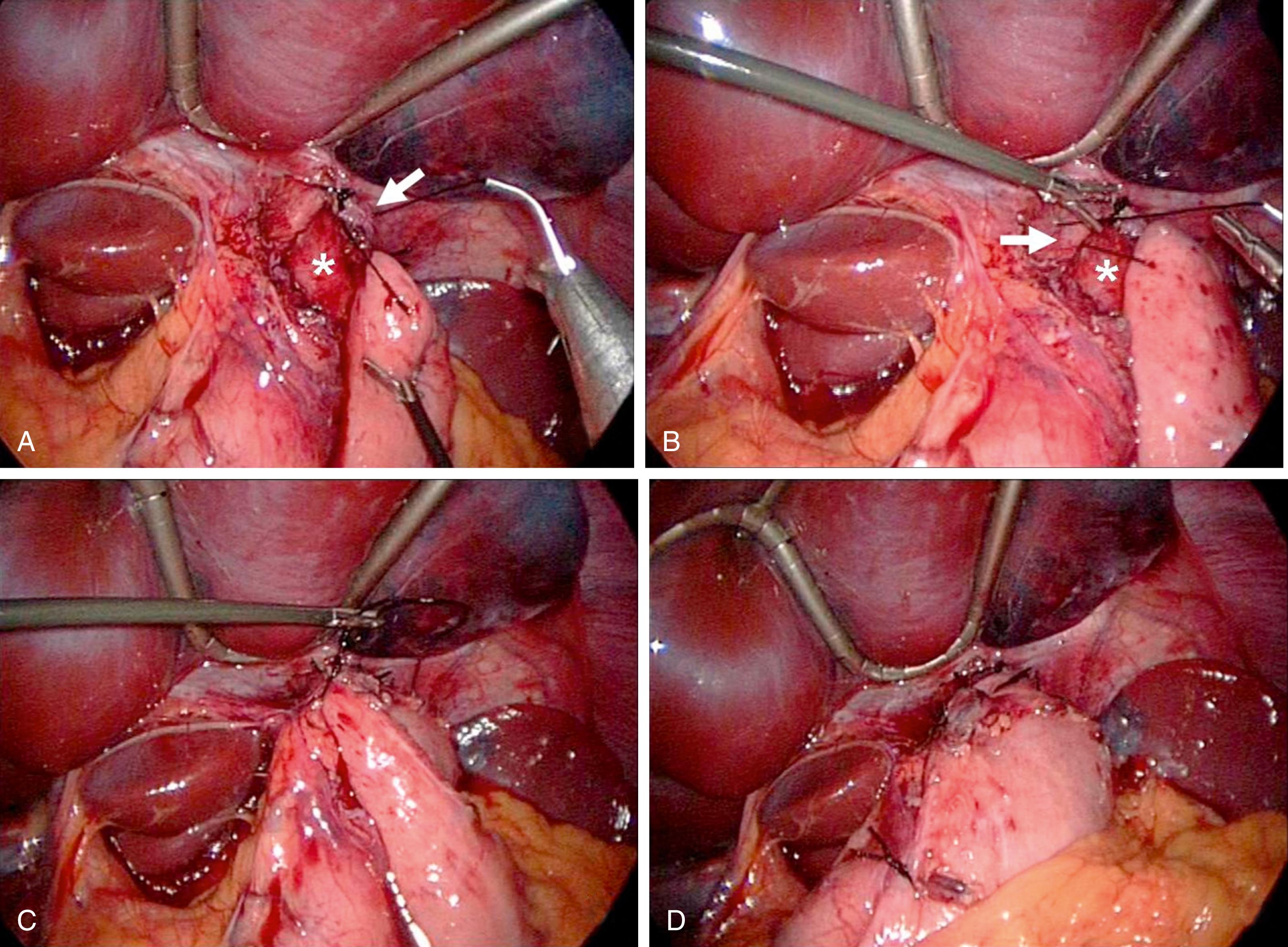
Insufflation pressures will range from 10 to 15 mm Hg, again dependent on patient age and size. We routinely use flexible endoscopy intraoperatively for assessment and measurement of the location of the EGJ, and prefer to leave the endoscope in the stomach during the LEM (with the endoscope light off). In addition, we utilize the endoscopic functional lumen imaging probe (EndoFLIP, Medtronic, Minneapolis, MN) to calibrate the cross-sectional area of the EGJ prior to and following esophagomyotomy to assess the adequacy of the myotomy. A 5-mm liver retractor is inserted and positioned to elevate the left lobe of the liver off the stomach, esophagus, and hiatus ( Fig. 3-3A ). The esophagus is exposed by dividing the gastrohepatic and phrenoesophageal ligaments and the phrenoesophageal fat pad with hook electrocautery. This anterior hiatal dissection will expose the distal esophagus, and identification of the anterior vagus nerve will determine whether the esophagogastric myotomy will be more readily accomplished on either the patient’s right or left of this nerve. The esophagus and stomach are marked with electrocautery along the proposed course of the myotomy for a length of 5 to 7 cm on the esophagus and 2 to 3 cm onto the stomach ( Fig. 3-3B ). The myotomy is initiated on the esophagus by incising the longitudinal muscle with hook electrocautery. The longitudinal fibers can be pulled apart with blunt graspers proximally and distally to carry the dissection more deeply to expose the circular muscle layer ( Fig. 3-3C and 3-3D ). Once the circular muscle layer is encountered, the muscle is lifted away from the submucosal layer and divided with a hook electrocautery. Once this dissection plane is achieved, dissection proceeds cephalad ( Fig. 3-4A ) and then distally ( Fig. 3-4B ) by dividing the circular muscle layer completely to the submucosal level. Circular muscular division is enhanced by elevating these muscle fibers with graspers or a Maryland instrument (see Fig. 3-4B ). It is very important to carry this dissection into the gastric wall for 2 to 3 cm ( Fig. 3-4C ). One should periodically measure the length of the myotomy for reference (esophageal plus gastric myotomy length) ( Fig. 3-4D ). Repeat endoscopy can be performed at any time to assess the EGJ and ensure it has been opened adequately (2 to 3 cm on the gastric side and 5 to 7 cm on the esophageal side). If an antireflux procedure is added to the myotomy, we perform an anterior Dor fundoplication. The fundus is mobilized and attached to the anterior aspect of the myotomy. This is done with silk or other permanent suture by placing two to three sutures first on the patient’s left side of the myotomy to the fundus, followed by two to three more sutures from the fundus to the patient’s right side of the myotomy ( Fig. 3-5 ).
The patient is left nothing per os (NPO) following the LEM and an esophagram is performed on postoperative day 1. This study is obtained not so much to look for an esophageal leak (as this usually would have been identified on intraoperative endoscopy), but to document a baseline appearance of the postmyotomy EGJ. In the event of recurrent symptoms in the future (e.g., dysphagia, chest pain, or regurgitation), a new esophagram can be performed for comparison. Assuming a normal postoperative esophagram, a liquid diet is commenced and discharge typically occurs on postoperative day 1 or 2. A soft diet (no hard, solid food) is recommended for 2 to 3 weeks post-LEM (or until outpatient follow-up). Pre- and postoperative Eckardt scores are recorded to assess the results of the myotomy and these scores are monitored long term ( Table 3-1 ).
| Patients | 25 | |
| Female | 13 | 52% |
| Male | 12 | 48% |
| Mean | ||
|---|---|---|
| Age at operation (years) | 12.9 | 0.75-18 |
| Operative time (minutes) | 120 | 45-180 |
| Length of stay (days) | 1.9 | 1-6 |
| Follow-up (months) | 32 | 8-94 |
| Operation | n | |
|---|---|---|
| LHM | 11 | 44% |
| LHM + DF | 13 | 52% |
| ∗ LHM + takedown DF | 1 | 2% |
| Complications | Management | |
|---|---|---|
| Mucosal perforation | 1 | Laparoscopic repair |
| Esophageal leaks | 0 | |
| Open conversion/death | 0 | |
| Recurrent dysphagia | 5 | Balloon dilation (1-3×) |
| Redo Heller myotomy | 0 | |
| Reflux | 1 | Antacid medications |
| Outcomes | ||
|---|---|---|
| Normalization of Eckardt scores (< 3) | 25 | 100% |
| Mean | ||
|---|---|---|
| Preoperative Eckardt score | 9.7 | (3-11) |
| Postoperative Eckardt score | 0.9 | (0-3) |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here