Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Disease ensues when normal physiological mechanisms and processes are disrupted. These processes take place in the basic unit of living organisms: the cell. It is therefore essential that all clinicians understand normal cellular and molecular mechanisms and processes in order to understand disease. The following chapters address specific mechanisms related to particular areas of human function and systems of the body.
The basic science concepts that attempt to explain disease processes cannot be undervalued. The best diagnostic and most effective therapeutic decisions made by clinicians have to be underpinned by sound scientific principles. The inclusion of all the relevant basic sciences in one book will, hopefully, be useful.
This chapter gives an overview of the principles of mechanisms that enable the body to work as a biochemical system. The functional unit of the human organism is the cell ( Ch. 2 , Fig. 2.39 ). All cells are surrounded by a cell membrane , also known as the plasma membrane . Other cell components are contained in the cytoplasm in which the cellular elements (organelles), including the nucleus, are suspended in the cytosol ( intracellular fluid ( ICF ) or cytoplasmic matrix ). Cells are suspended in fluid composed of water and a variety of biologically active molecules. Movement of these molecules into and out of cells, involving both active and passive transport, triggers the physiological mechanisms that enable the cells to perform their normal physiological functions. Examples include protein synthesis, regulation of cell function (signalling), cell movement, metabolism (glucose and respiration), cell division and death (apoptosis), skeletal and cardiac muscle contraction, the transmission of signals along nerve fibres, the digestion and absorption of nutrients in the alimentary system, the synthesis and secretion of hormones by the endocrine system, transport of oxygen and carbon dioxide by blood, the exchange of respiratory gases and the important functions performed by the renal system. These cells perform different functions, and therefore possess different properties, described in detail in the ensuing chapters on the systems of the body. Understanding cell and molecular biology – the similarities and differences between cell types, their components and functions – is essential to understanding the clinical sciences because disease results from the disruption of normal mechanisms. These principles underpin the development of disease, therapeutics and, in particular, the understanding of cancers and their treatment.
Chapter 3 discusses the cellular mechanisms that enable human beings to produce the energy needed to survive, maintain body temperature and work. Most biological processes are driven by energy in the form of adenosine triphosphate (ATP), produced through metabolism of the food that we eat. The main metabolic fuels are carbohydrate, protein and fat. The most important source of energy is glucose, but the body has intricate and dynamic adaptive mechanisms for using alternate fuels under particular physiological conditions. Metabolism occurs in cells. It is tightly regulated by the actions of enzymes, gene expression and transcription in response to changing demands on the need for energy and by the action of hormones, which may take place rapidly or gradually. Energy metabolism is essential for life, and disturbances can lead to important diseases, such as diabetes mellitus.
This chapter describes how drugs work (pharmacodynamics) and how they are absorbed, distributed around the body (pharmacokinetics), metabolised and then eliminated. Knowledge of cell and molecular biology underpins the understanding of pharmacology and therapeutics. The pharmacokinetics and pharmacodynamics of synthetic drugs depend on their individual properties. Specific classes of drugs share common properties, but there are variations between individual drugs. It is also important to remember that how a drug performs in the laboratory (in vitro) is not necessarily how it performs in the body (in vivo), which is important for the safety and effectiveness of drugs. Generally, pharmacokinetics follows the principles of cell biology. In pharmacodynamics, drugs work by targeting cellular processes to either enhance or inhibit the process. Examples include the targeting of enzymes, transport processes and receptors on cell surfaces. Here, understanding of the autonomic nervous system is essential because most drugs are designed to target elements of this system.
The understanding of genetics dates back to Charles Darwin's (1809–1882) On the Origin of Species (1859), later further explained by Gregor Mendel's (1822–1884) principles of inheritance and mutations. The most exciting modern development in genetics was the Human Genome Project, which mapped the complete set of genetic codes stored as DNA sequences in the whole 23 chromosomes of the human cell nucleus and took place between 1990 and 2003. The Human Genome Project published the working draft of the human genome in 2000; the complete genome was published in 2003.
Taking advantage of the multiplexing capabilities of new sequencing technologies, the 1000 Genomes Project ran from 2008 until 2015, targeting sequence variation in five continental regions. In 2015 Nature published this work, which mapped population genetic variation from more than 2500 human genomes, providing publically available data for research.
In the UK the 100,000 Genomes Project was launched by Genomics England at the end of 2012. Its aim was to provide sequence data from NHS patients diagnosed with cancer or a rare disease with the aim of stimulating the UK genomics industry. With its medicine-focussed approach the 100,000 Genomes Project is currently planned to run until the end of 2018 and has been expanded to include infectious disease. By mid-2017 the project had sequenced more than 36,000 genomes, putting the UK at the forefront of using genomic technology to transform patient care. The importance of partnering with industry is crucial to the project so that frontline clinicians of the future will be provided with the necessary infrastructure to benefit from this exciting future so that we can better understand disease processes and the development of preventive measures, diagnosis, prognosis and therapeutic strategies as genomic medicine moves into the mainstream.
Pathology and immunology are essential for understanding disease processes to enable the clinician to formulate sensible diagnostic and therapeutic decisions. Infectious diseases and the body's response to them, immunology, are discussed. Disorders of the immune system, including autoimmunity and hypersensitivity, are also discussed. In these conditions, it is thought that there is a defect in the genetic regulation of the immune response. The inflammatory response underpins the body's defence mechanisms and needs to be fully understood. This is followed by the pathology of neoplasia; cancers, which cause about 25% of all deaths in the UK. The pathology of common degenerative diseases is discussed in the chapters on systems of the body. Once again, molecular and cellular biology and medical genomics form the basis for understanding these processes.
Chapter 7 is about the epidemiological principles that underpin the discovery of patterns of diseases and their occurrence in populations, and how the effectiveness of therapeutic interventions is evaluated. It is, perhaps, unusual to consider this as a basic science. Epidemiology and the epidemiological approach, however, is the science that underpins the art of clinical medicine. Observational studies form the cornerstone of clinical medicine.
For example, how do we know how to diagnose disease from patient descriptions of symptoms? Our understanding of how disease presents and progresses clinically is based on repeated, multiple observations by many doctors and the sharing of their observations; e.g. whooping cough, which starts like a common cold, before the cough develops and continues for up to 100 days. The cough is characteristic in being spasmodic and prolonged, often ending in a sharp intake of breath – the ‘whoop’.
In the example of John Snow and the Broad Street Pump, Snow found the association between the water from the Broad Street Pump and the cholera epidemic. The actual cause of cholera, the organism Vibrio cholerae , was not discovered until later by Filippo Pacini, an Italian anatomist, and was not widely known until published by Robert Koch some 30 years thereafter. Until the comma-shaped bacterium was identified, treatment and prevention could not be formulated. Careful and systematic observation thus formed the basis for further research into the cause of this disease.
Moreover, how do we select therapeutic interventions, whether pharmacological or surgical? How do we know that this intervention is effective, or more effective than another one? Here, the methodology for experimental studies, e.g. randomised controlled trials, and the statistical concepts that underpin the proof for the likelihood of a positive effect need to be understood. The mathematics might be daunting, but understanding the principles is essential. These principles also apply to diagnostic and screening tests.
The next eight chapters are about all the systems of the body and discuss the cellular makeup of different organs, their functions, normal metabolic processes in health and the biological basis for disturbance leading to disease. Understanding these processes forms the rationale for diagnostic and therapeutic decisions. Despite their separation, the systems interconnect so that the body functions as a whole. Rather than describe each chapter in detail, it might be more helpful to think about the cellular mechanisms that ensure normal physiological function. These basic mechanisms are common to all living organisms, including Homo sapiens .
As mentioned previously, the basic unit of the human organism is the cell. Normal biological functioning is determined by molecular and cellular processes and controlled by human genomics and epigenetic modification, as outlined in Chapter 5 . The cells in each system vary according to their physiological function. For example, hepatic (liver) and muscle cells both store glycogen, but the primary function of the liver is to release glucose converted from glycogen (glycogenolysis) into the circulation when there is a shortage of glucose, whereas muscle cells (myocytes) are primarily need to break down the stored glycogen for generating ATP for muscle contraction. Skeletal muscle lacks the enzyme glucose-6-phosphatase (G6Pase); glucose-6-phosphate generated from muscle in glycogenolysis instead enters the glycolytic pathway after glucose, preserving one of the ATP molecules consumed at the start of glycolysis.
A more obvious example of the influence of genomics is sickle cell disease (SCD). This is a condition where there is a mutation in the haemoglobin gene (β-globin gene), leading to the red cells assuming a sickle shape and becoming rigid. Sickle cells confer a resistance to malarial infection, and the mutation arose historically among populations in tropical and subtropical regions where malaria is endemic. The disadvantage is that, under conditions of reduced oxygenation, infection, cold or dehydration, the sickle haemoglobin elongates and cannot flow smoothly through small blood vessels. It sticks to the vessel lining, leading to occlusion of the vessels and causing sickle cell crises, which may be life-threatening. An understanding of molecular and cell biology and human genomics for the cells in each system is therefore necessary for understanding disease processes.
Chapter 16 is about the nutritional needs for humans to stay alive and, more importantly, the principles for assessing these needs in health and disease. What makes a human being eat or not eat is also addressed, with implications for dietary control of conditions such as obesity and some therapeutic diets for chronic conditions such as inflammatory bowel disease. The association between diet and disease is also discussed. Nutritional support during severe illness, artificial nutrition, and associated complications are discussed. Artificial nutrition includes enteral feeding, i.e. putting feeding liquid directly into the stomach or small intestine, and parenteral nutrition, which is intravenous feeding. The makeup of the feeding fluid will depend on the nutritional needs of the patient. These principles are important, especially during the foundation years. Inclusion of nutrition as a basic science in this book is perhaps unusual, but clinicians need to know about these principles for sustaining life.
To maintain the normal physiological processes for sustaining life, all living organisms and cells have to maintain a stable internal environment in response to changes in external conditions. Physiologists have called this function homeostasis , from the Greek homeo meaning same or unchanging, and stasis meaning standing still. When an attribute of the organism or cell (such as pH or temperature) changes for any reason, this complex system of processes adjusts the attribute back to the set constant level needed for physiological functioning. Such an attribute is labelled a variable , something that is changeable.
Homeostatic systems are multiple, dynamic mechanisms that are regulated (or controlled) for making the adjustments necessary for a stable internal environment; this is unlike simple dynamic equilibrium or steady states that are not regulated. Many examples of human homeostasis are discussed in the following chapters. Disease ensues when homeostatic mechanisms break down and the body exhibits symptoms (what the patient experiences) and signs (what the clinician finds on clinical examination).
Many physiological parameters, such as blood glucose level (discussed in detail in Ch. 3 , Energy and metabolism), water and electrolyte (sodium, potassium, calcium, etc.) balance and body temperature, are examples of precise control by homeostatic mechanisms. Of the homeostatic mechanisms that control body fluids, fluid balance (the control of fluid volumes) and acid–base balance (the control of acidity [H + ions]) are important to understand.
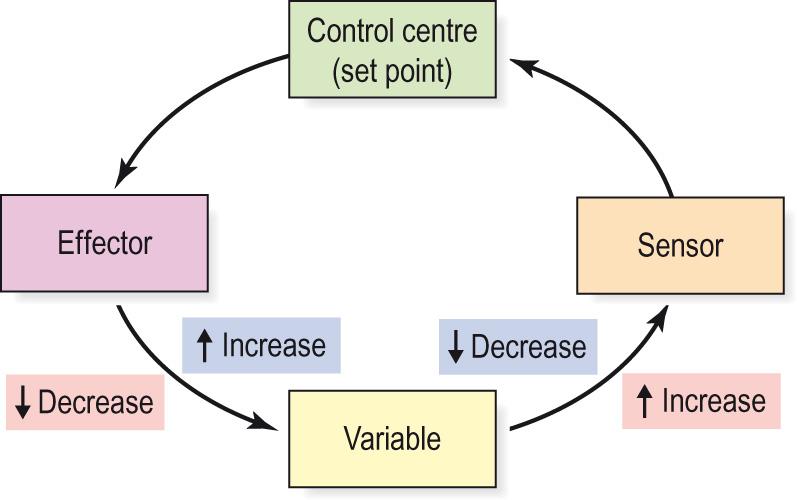
Homeostatic control mechanisms have three (sometimes more) interdependent components for the variable being regulated.
A receptor that detects, monitors and responds to changes (sometimes wide variation) in a variable in the external environment; known as the sensor .
The sensor sends information to a control centre that sets the physiological range for the variable, and determines the necessary response for bringing the variable back to the set point. In humans, the control centre is usually in the brain. Many examples are discussed in Chapter 8 .
The control centre sends signals to the tissues and organs, known as the effectors , that have to effect, i.e. make the adjustment, to changes in the relevant variable to bring it back to its set point.
A simplistic analogy would be ambient temperature control in air-conditioning systems, where the thermostat is the sensor responding to changes in environmental temperature, set at a comfortable level. It also acts as the control system that switches heating or cooling systems on and off. The effector would be the heating and cooling systems with their own, separate mechanisms.
Once the control centre receives the stimulus that a variable has changed from the set point, it sends signals to effectors to correct the change by:
Negative feedback to depress the change if the variable level has increased beyond the narrow, set range. This is the commonest mechanism.
Positive feedback to affect an increase or acceleration in the output variable that has already been triggered. The result is to push the level beyond the physiological range.
Feedforward control to either depress or enhance the level of a variable before the change is needed, i.e. anticipatory (or open loop). Open-loop systems have no way to calibrate against the set point and so always need an accompanying closed-loop negative feedback to correct any over- or underanticipation.
Negative feedback mechanisms can either increase or reduce the activity of tissues or organs back to normal, set levels, and the system is sometimes called a negative feedback loop ( Fig. 1.1 ) . Numerous examples of negative feedback exist in the metabolic processes of all physiological systems.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here