Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Liver frozen sections, like frozen sections in general, are required when the results stand to alter the course of the surgical procedure. Indications for frozen section examination can be divided into four major categories:
Evaluation for possible metastatic disease—typically involving the sampling of surface lesions identified during staging procedures or during other abdominal procedures. These may be single or multiple lesions.
Liver resection—evaluation of surgical margins in oncologic resections at the time of partial hepatectomy and biliary resections
Evaluation of a liver mass—typically frozen section is requested to be sure that adequate sampling has been performed for permanent evaluation
Evaluation of hepatic parenchyma—either at the time of another abdominal procedure when the results will affect intraoperative decisions or in the transplant setting when results will affect organ utilization
Most cancer operations of the abdomen include an evaluation of peritoneal and hepatic surfaces to exclude metastatic disease. In some cases, such as the patient with gastrointestinal perforation from colon cancer, the finding of metastatic hepatic disease may not change the need for resection of the primary tumor. In many cases, however, the finding of metastatic disease on the surface of the liver effectively upstages the patient to that of metastatic disease and, as such, may obviate the value of resection of the primary tumor. Tumors over 5 mm are often visible on preoperative cross-sectional imaging but may still be biopsied or removed at the time of surgery for another primary tumor, whereas tumors less than 5 mm are less likely to be visualized on preoperative imaging and might only be identified by visual inspection of the capsule of the liver or by palpation.
The frozen section is obtained whether these lesions are benign or malignant/metastatic and is critical to intraoperative decision making. This information helps the surgeon determine whether or not more radical surgery/definitive/curative resection should be undertaken which, in turn, involves removal of another abdominal organ. For example, in a patient with adenocarcinoma of the pancreas, the finding of metastatic adenocarcinoma in the frozen section evaluation of such liver lesions might obviate a pancreatic resection because the patient is less likely to benefit from resection of a primary pancreatic adenocarcinoma in the context of systemic disease. Metastatic adenocarcinoma is the most likely tumor to require distinction from benign hepatic biliary lesions because adenocarcinoma is comprised of glands that mimic the biliary ductal or ductular structures of biliary lesions.
Visual inspection of the surface of the liver during laparoscopy or laparotomy occasionally identifies enlarged edematous portal tracts that are apparent through the liver capsule as a white area, mimicking a mass lesion.
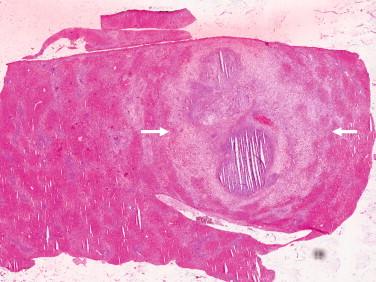
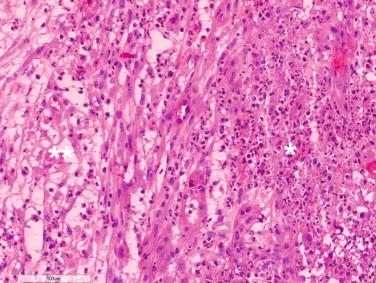
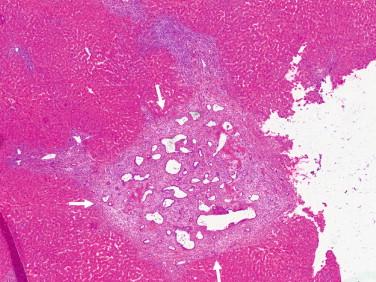
These may be visualized and sampled by the surgeon to rule out metastases. Such lesions may be loosely labeled as “nodule.” This is typically encountered at the time of laparotomy in patients with a large bile duct obstruction such as with periampullary carcinoma (Yantiss, 2011). The sampled portal tracts are edematous or fibrotic with peripheral ductular reaction that may be exuberant and possess an inflammatory infiltrate ( Figures 14-1 and 14-2 ). If ascending cholangitis were present, the bile duct may be dilated and contain variable amounts of neutrophils, occasionally with duct rupture and abscess formation ( Figures 14-3 and 14-4 ). In severe instances, the dilated ruptured bile duct with abscess represents the lesion visualized at the surface of the liver.
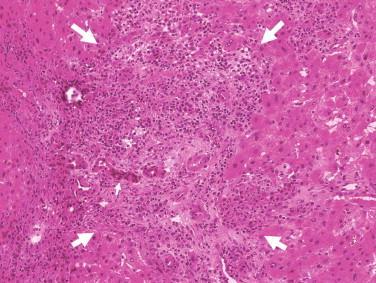
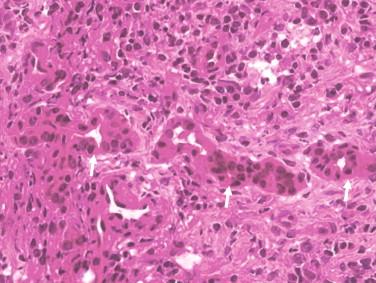
Distinction of these benign ductular reactions/proliferations from malignant glands is aided by the mild degree of cytologic atypia encountered in the benign ductular proliferation.
One of the helpful hints in these cases includes the recognition of the topography of the lesion, including the presence in a portal tract containing a bile duct and/or the hepatic artery, a wreathlike pattern of ductular proliferation in the portal area, mild cytologic atypia, and comparison of cytologic features of lesional ductular structures with those in other portal areas elsewhere in the sampled liver tissue. Distinction from adenocarcinoma can be difficult when the proliferating benign ductules are angulated or compressed. These architectural features, along with reactive or fibrotic stroma, mimic metastatic carcinoma. Preoperative neoadjuvant chemotherapy further confounds frozen section interpretation.
Bile duct hamartomas are benign lesions that may be seen sporadically or in association with cystic kidney and liver disease (Goodman et al, 2012). They were found in 5.6% of adults and 0.9% of children in one autopsy series (Redston and Wanless, 1996). Bile duct hamartomas may be so numerous that they mimic diffuse hepatic metastases (Fritz et al, 2006). Bile duct hamartomas appear as white nodular lesions intraoperatively. They are seldom larger than 5 mm in size (Goodman et al, 2012). In the setting of oncologic resections, the finding of white liver nodules raises the possibility of metastatic disease. Bile duct hamartomas come to frozen section examination to confirm or exclude the diagnosis of metastases, which could preclude further curative resection (Yantiss, 2011). They are composed of variably dilated ductular structures with staghorn (antler horn) shapes. They are lined by flat or cuboidal epithelium without cytologic atypia ( Figures 14-5 and 14-6 ). Their lumens sometimes contain bile concrements. The stroma is usually hyalinized. The lesion is usually well defined, located portally or periportally. Architectural and benign cytologic features are helpful to distinguish hamartoma from adenocarcinoma.
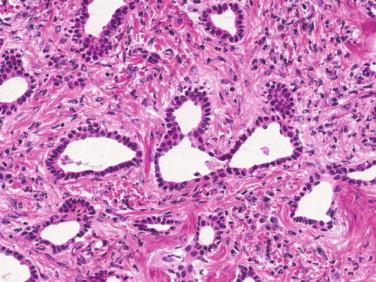
Adenocarcinoma deposits are usually ill-defined, expansile nodules composed of irregularly shaped glands with or without infiltrating single cells embedded in desmoplastic stroma. Carcinomatous glands are variably spaced and haphazardly arranged. Their lining epithelial cells show atypical features such as hyperchromatic nuclei and high nuclear-to-cytoplasmic ratio. Malignant glands do not contain inspissated bile. This presence of inspissated bile in hamartomas is not always seen but, when present, is very helpful. Intraluminal mucin is usually absent in bile duct hamartoma and may be present in adenocarcinoma. Mitoses are seen in adenocarcinoma but not in bile duct hamartoma.
Bile duct adenomas are unusual and, when encountered, usually appear as solitary or multiple white nodules. They are usually subcapsular, well demarcated, and less than 1.5 cm. The lesion is not encapsulated. It is composed of uniform small tubular structures. The epithelial lining of the tubular structures is cuboidal and plump. The densely packed tubules are embedded in a compact, cellular stroma. Cytologic atypia may be present but is usually mild. The lesion does not contain bile. Particularly useful for identifying bile duct adenomas is their lack of infiltrating or displacing growth in relationship to the liver parenchyma (Yantiss, 2011).
Features that favor bile duct adenoma over adenocarcinoma are the well-circumscribed appearance of the adenoma and the presence of only mild cytologic atypia in the lesions. Well-differentiated adenocarcinomas show relatively more variation in shape and spacing of the malignant glands, and infiltrating individual cells or incomplete glands may be present. In addition, they usually show more pronounced cytologic atypia and poor circumscription from the surrounding parenchyma. Perineural and invasive growth into the hepatic parenchyma are diagnostically conclusive for adenocarcinoma.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here