Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The exact pathogenesis of bile duct carcinoma has not been described, but predisposing factors include long-standing inflammation, parasitic infestation, toxin and drug exposures, and genetic abnormalities. It is believed that repeated inflammation leads to chronic bile duct injury with formation of premalignant lesions. DNA alterations secondary to genetic mutations, bile salt exposure, or other carcinogens can predispose to biliary epithelial proliferation and subsequent tumorigenesis. Intrahepatic cholangiocarcinoma and hepatocellular carcinoma likely arise from a common progenitor cell based on experiments in patients with chronic liver disease.
Intrahepatic cholangiocarcinoma is the second most common primary hepatic cancer after hepatocellular carcinoma. Patients are older (50 to 60 years), with a male preponderance. Survival rates are initially high (50% at 1 year), but because of early metastasis, decline quickly (5% to 15% at 5 years). Established risk factors for the development of bile duct cancer include a family history of hepatic fibrosis, choledochal cysts, parasitic infestation (e.g., Clonorchis sinensis ), biliary stones, cholangitis, inflammatory bowel disease, chronic pancreatitis, thorium dioxide [Thorotrast] exposure, and certain medications. Factors that predispose specifically to intrahepatic cholangiocarcinoma include chronic hepatitis C virus infection, nonalcoholic liver disease, smoking, and obesity.
Symptoms of cholangiocarcinoma result from biliary obstruction. Thus, intrahepatic tumors manifest late in the course of disease. Patients develop jaundice and pruritus and may also complain of acholic stools and bilirubinuria. Other symptoms resulting from liver dysfunction also may be the presenting symptom.
Prolonged biliary obstruction is associated with cholangitis, cirrhosis, renal dysfunction, and progressive malnutrition.
Intrahepatic cholangiocarcinoma metastasizes early, with a poor prognosis, and early surgical resection is the only chance for curative treatment.
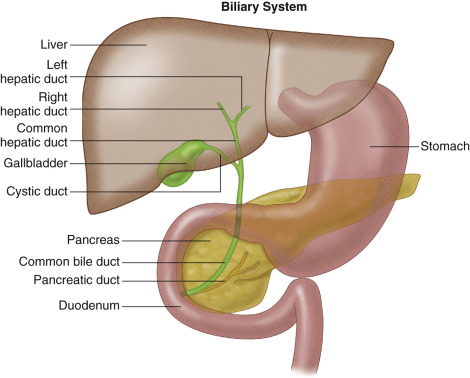
The liver consists of bile-secreting hepatocytes draining into bile canaliculi, which merge into hepatic ductules to form the intrahepatic main right and left hepatic ducts. These converge just outside the liver to form the common hepatic duct ( Figure 54-1 ).
Bile duct tumors are classified as extrahepatic (87% to 92%) or intrahepatic (8% to 13%). Intrahepatic tumors develop in the small ductal branches within the liver. Morphologically, intrahepatic cholangiocarcinomas may exhibit mass-forming (most common), intraductal-growing, periductal-infiltrating, or combined growth patterns.
The majority of intrahepatic cholangiocarcinomas are solitary, well-circumscribed tumors. Tumors may be peripherally or centrally located. A single hepatic duct is involved in 8% to 13% of cases. Satellite nodules surrounding the main tumor occur in approximately 65% of patients. Ten percent of tumors have a diffuse multicentric distribution with no dominant mass.
Cholangiocarcinomas most commonly disseminate via perineural invasion and lymphatics with involvement of the cystic and common bile duct nodes in 15% of patients. Hematogenous spread is extremely rare. Tumors also can directly infiltrate adjacent liver or cause peritoneal seeding.
Staging of intrahepatic cholangiocarcinoma is performed using the American Joint Committee on Cancer Staging Tumor, Node, Metastasis (TNM) system of classification ( Table 54-1 ).
| TNM Definition | Tumor Location |
|---|---|
| TX | Primary tumor cannot be assessed |
| T0 | No evidence of primary tumor |
| Tis | Intramucosal carcinoma (intraductal tumor) |
| T1 | Solitary tumor without vascular invasion |
| T2a | Solitary tumor with vascular invasion |
| T2b | Multiple tumors, with or without vascular invasion |
| T3 | Tumor perforating the visceral peritoneum or involving the local extrahepatic structures by direct invasion |
| T4 | Tumor with periductal invasion |
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | Regional lymph node metastasis present |
| M0 | No distant metastasis |
| M1 | Distant metastasis |
Benign biliary tumors such as adenomas, hamartomas, cystadenomas, and papillomas are extremely rare compared with malignant cholangiocarcinomas.
Histologically, the majority (95%) of malignant cancers are mucin-secreting adenocarcinomas with varying levels of differentiation. Pathologic subtypes include scirrhous, nodular, and papillary cancers. The scirrhous type creates fibrotic annular thickenings with low cellularity and is generally seen in the proximal ducts and hilum.
Microscopic findings of anisonucleosis and distended intracytoplasmic lumina support the diagnosis of bile duct cancer. Immunohistochemical staining for carcinoembryonic antigen (CEA), carbohydrate antigens (CA 50 and CA 19-9), and mucins may facilitate diagnosis. The pathologic findings of cholangiocarcinoma and metastatic adenocarcinoma of unknown origin can be especially difficult to differentiate. Cytokeratin (CK) 7 suggests a gastric or colorectal primary, and CK-20 suggests cholangiocarcinoma. Mutations in the KRAS oncogene are seen in intrahepatic and perihilar tumors. Studies have also identified mutations in the TP53 tumor suppressor gene, c-erb oncogene, chromosomes 5 and 17, epidermal growth factors, and nuclear antigens.
Bile duct tumors are variable in location and morphology and may require multiple modalities for complete characterization. In general, intrahepatic tumors are larger than their extrahepatic counterparts and more conspicuous on imaging. Imaging is also used to evaluate vascular and ductal anatomy, secondary signs of obstruction, and metastatic disease.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here