Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Anterior and posterior cervical foraminotomy
Lumbar microdiscectomy
Lumbar laminotomy and foraminotomy
Endoscopic foraminotomy and discectomy
Transforaminal lumbar interbody fusion (TLIF)
A number of surgical procedures are performed in and around the foramina of the spine, commonly in the cervical or lumbar spine and occasionally in the thoracic spine. They generally consist of decompressive procedures such as a foraminotomy. Different approaches to accomplish a foraminotomy and fusion procedures undertaken through the foramen, such as a transforaminal lumbar interbody fusion (TLIF), are discussed briefly, together with a review of the relevant anatomy. The anatomy of the ligaments, their pathological relationships to clinical entities and their importance in spinal stability are reviewed.
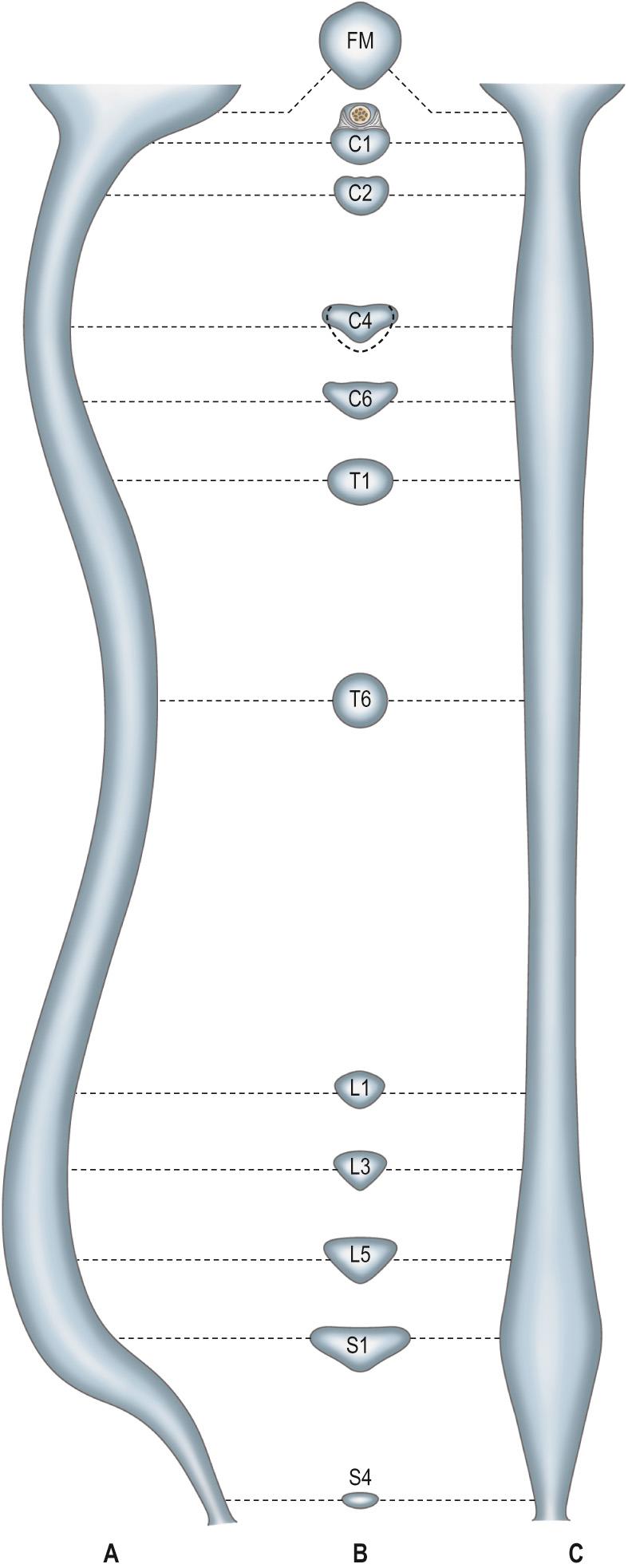
The vertebral canal extends from the foramen magnum to the sacral hiatus and follows the vertebral curves ( Fig. 31.1 ). In the cervical and lumbar regions, which exhibit free mobility, it is large and triangular, but in the thoracic region, where movement is less, it is small and circular. These differences are matched by variations in the diameter of the spinal cord and its enlargements. In the lumbar region, the vertebral canal decreases gradually in size between L1 and L5, with a greater relative width in the female.
For clinical purposes, it is useful to consider the vertebral canal as having three zones: a central zone, between the medial margins of the facet joints, and two lateral zones, beneath the facet joints and entering the intervertebral foramina. Each lateral zone passes into and just beyond the intervertebral foramen, and can be subdivided into subarticular (lateral recess), foraminal and extraforaminal regions. The lateral zone thus described forms the canal of the spinal nerve (the radicular or ‘root’ canal). If the lateral recess is considered to be part of the radicular canal rather than part of the central zone, then the central zone of the canal is a little narrower than the radiological interpedicular distance.
Narrowing (stenosis) of the vertebral canal may occur at single or multiple spinal levels, and mainly affects the lumbar and cervical regions.
Stenosis may affect the central canal and the ‘root canals’ either together or separately. There is a developmental form of the condition which mainly affects the central canal, but more commonly the stenosis is degenerative and results from intervertebral disc narrowing and osteoarthritic changes in the facet joints. This latter combination is more likely to narrow the intervertebral foramen and the ‘root canal’, even though the sectional profile of the vertebral canal in affected lumbar vertebrae typically changes from the shape of a bell to that of a trefoil. The lumbosacral intervertebral foramen, which is normally the smallest in the region, is particularly liable to such stenosis. Severe spinal stenosis may compress the spinal cord and compromise its arterial supply. More localized ‘root canal’ stenosis will present with the clinical features of spinal nerve compression but without the tension signs that characterize the stretching of nerve roots over a prolapsed disc. Ischaemia of the nerves and roots may provoke more damage than the actual physical compression of the neural tissue.
Stenosis can also affect the cervical and thoracic spine. If the central canal is affected, this can manifest as myelopathy. Cervical and/or thoracic radiculopathy may result if the neuroforamina are narrowed in size. This is usually due to a combination of superior articular facet tip hypertrophy and disc degeneration ( Fig. 31.2 ). If needed, this can be treated surgically via a laminoforaminotomy with mesial facetectomy (see below).

Intervertebral foramina are the principal routes of entry to and exit from the vertebral canal and are closely related to the main intervertebral articulations. (Minor routes occur between the median, often partly fused, margins of the ligamenta flava.) The same general arrangement applies throughout the vertebral column, between the axis and sacrum, although there are some quantitative and structural regional variations. Because of their construction, contents and susceptibilities to multiple disorders, the intervertebral foramina are loci of great biomechanical, functional and clinical significance.
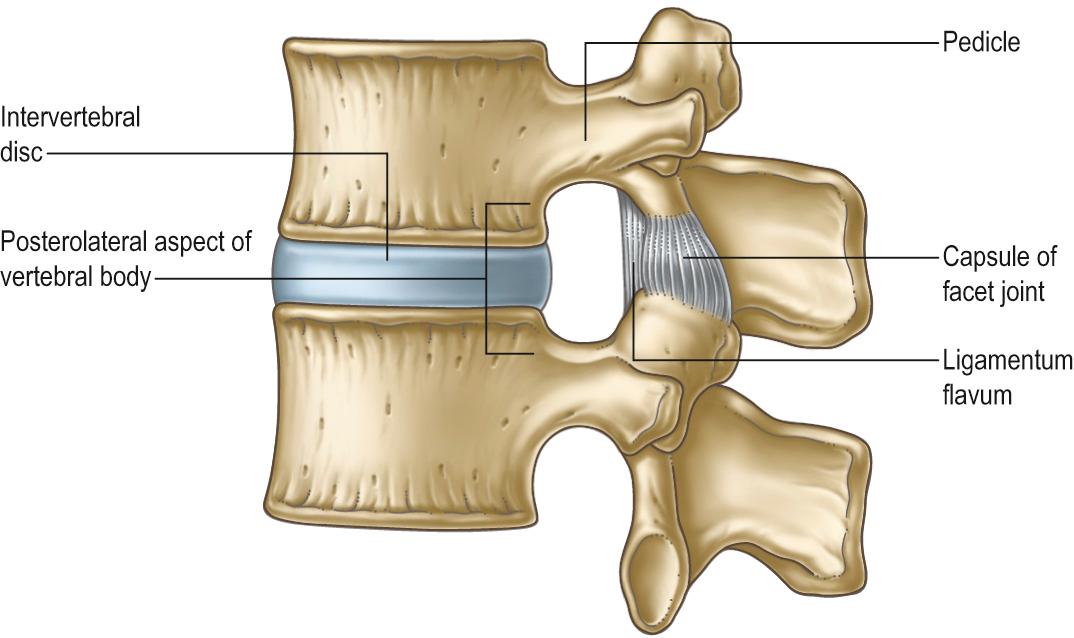
The boundaries of a generalized intervertebral foramen ( Fig. 31.3 ) are: anteriorly, from above downwards, the posterolateral aspect of the superior vertebral body, the posterolateral aspect of the intervertebral symphysis (including the disc), and a small (variable) posterolateral part of the body of the inferior vertebra; superiorly, the compact bone of the deep arched inferior vertebral notch of the vertebra above; inferiorly, the compact bone of the shallow superior vertebral notch of the vertebra below; and posteriorly, a part of the ventral aspect of the fibrous capsule of the facet synovial joint.
The thoracic and lumbar intervertebral foramina face laterally and their transverse processes are posterior. In addition, the anteroinferior boundaries of the first to tenth thoracic foramina are formed by the articulations of the head of a rib and the capsules of double synovial joints (with the demifacets on adjacent vertebrae and the intra-articular ligament between the costocapitular ridge and the intervertebral symphysis). Lumbar foramina lie between the two principal lines of vertebral attachment of psoas major. The walls of each foramen are covered throughout by fibrous tissue, which is in turn periosteal (though the presence of a true periosteum lining the vertebral canal is controversial ), perichondrial, anular and capsular. The more lateral parts of the foramina may be crossed at a variable level by narrow fibrous bands, the transforaminal ligaments (for detail of these ligaments see Bogduk ). The true foramen is the foraminal region of the canal of the spinal nerve (the radicular or ‘root’ canal). A foramen contains a segmental mixed spinal nerve and its sheaths, from two to four recurrent meningeal (sinuvertebral) nerves, variable numbers of spinal arteries, and plexiform venous connections between the internal and external vertebral venous plexuses. These structures, particularly the nerves, may be affected by trauma or one of the many disorders that may involve tissues bordering the foramen. In particular, nerve compression and irritation may be caused by intervertebral disc prolapse, or by bony entrapment as the size of the foramen decreases. This decrease may result from facet joint osteoarthritis, osteophyte formation, disc degeneration and degenerative spondylolisthesis, all of which may lead to lateral or foraminal spinal stenosis.
The anterior longitudinal ligament is a strong band that extends along the anterior surfaces of the vertebral bodies ( Fig. 31.4 ). It is broader caudally and thicker and narrower in thoracic than in cervical and lumbar regions, and is also relatively thicker and narrower opposite vertebral bodies than at the levels of intervertebral symphyses. It extends from the basilar part of the occipital bone to the anterior tubercle of C1 and the anterior surface of the body of C2, then continues caudally to the anterior surface of the upper sacrum. Its longitudinal fibres are strongly adherent to the intervertebral discs, hyaline cartilage end-plates and margins of adjacent vertebral bodies, and are loosely attached at intermediate levels of the bodies, where the ligament fills their anterior concavities, flattening the vertebral profile. At these various levels, ligamentous fibres blend with the subjacent periosteum, perichondrium and periphery of the anulus fibrosus. The anterior longitudinal ligament has several layers. The most superficial fibres are the longest and extend over three or four vertebrae, the intermediate extend between two or three, and the deepest from one body to the next. Laterally, short fibres connect adjacent vertebrae.
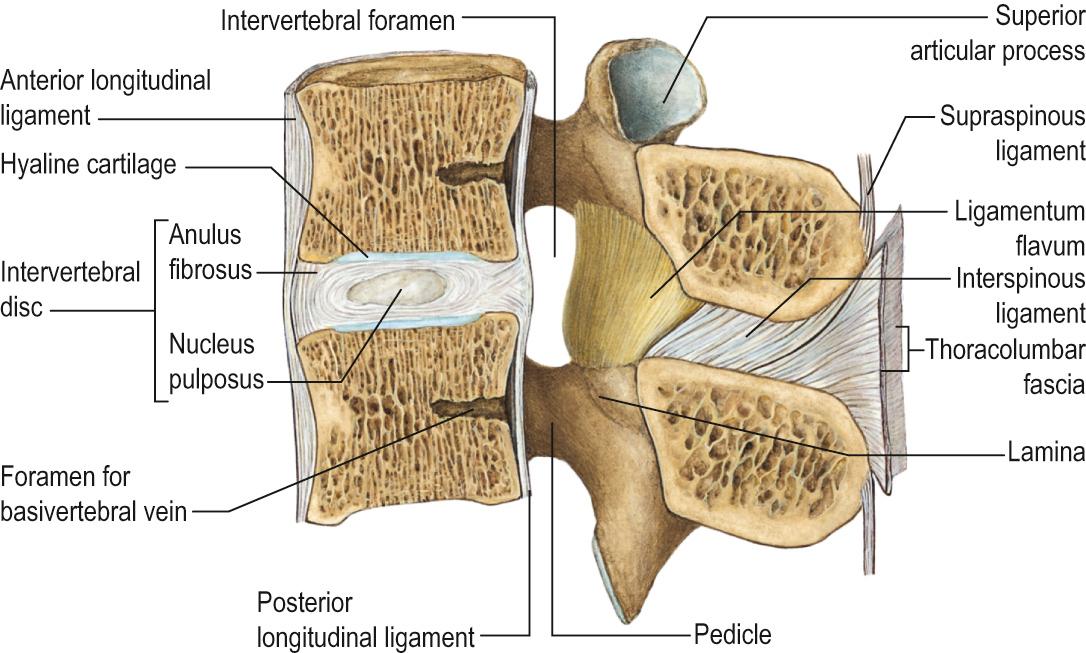
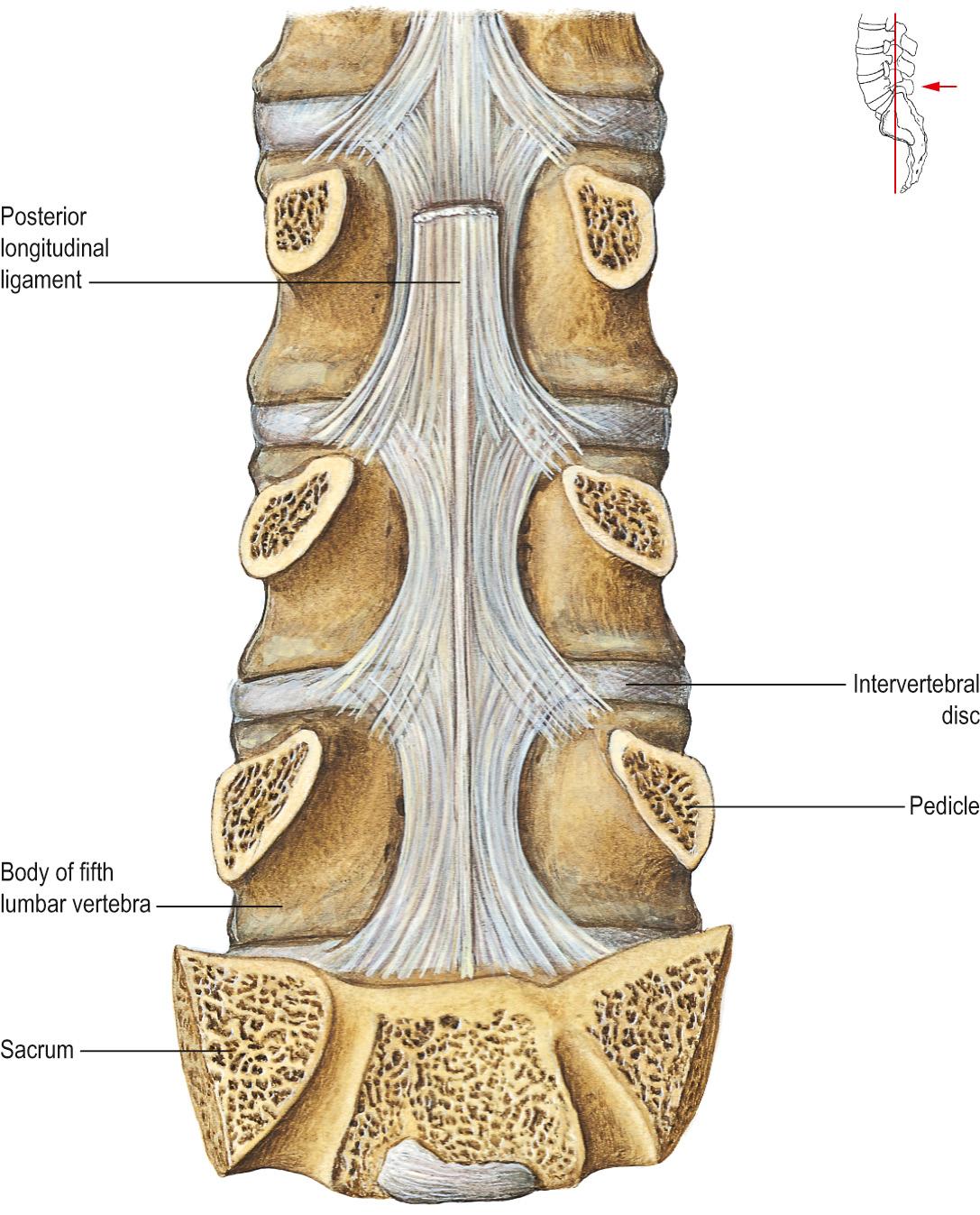
The posterior longitudinal ligament lies on the posterior surfaces of the vertebral bodies in the vertebral canal ( Fig. 31.5 ), attached between the body of C2 and the sacrum, and continuous with the membrana tectoria above. Its smooth, glistening fibres, attached to intervertebral discs, hyaline cartilage end-plates and adjacent margins of vertebral bodies, are separated between attachments by basivertebral veins and the venous channels which drain them into anterior internal vertebral plexuses. At cervical and upper thoracic levels the ligament is broad and of uniform width, but in lower thoracic and lumbar regions it is denticulated, narrow over vertebral bodies and broad over discs. Its superficial fibres bridge three or four vertebrae, while deeper fibres extend between adjacent vertebrae as perivertebral ligaments, which are close to and, in adults, fused with, the anulus fibrosus of the intervertebral disc. The layers of the posterior longitudinal ligament and the relationship of the ligament to associated membranes in the epidural space are fully discussed by Loughenbury et al.
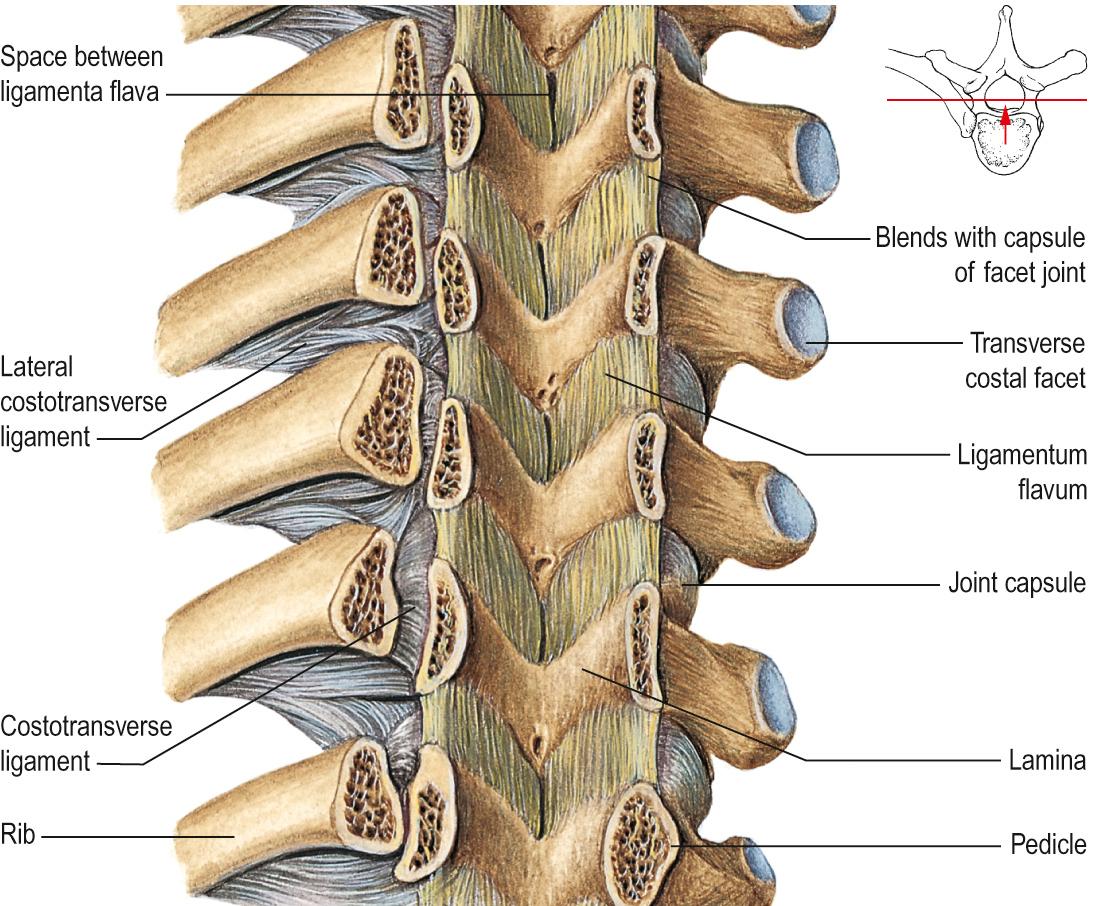
The ligamenta flava connect laminae of adjacent vertebrae in the vertebral canal ( Fig. 31.6 ). Their attachments extend from facet joint capsules to the point where laminae fuse to form spines. Here their posterior margins meet and are partially united; the intervals between them admit veins which connect the internal and posterior external vertebral venous plexuses. Their predominant tissue is yellow elastic tissue, whose almost perpendicular fibres descend from the lower anterior surface of one lamina to the posterior surface and upper margin of the lamina below. The anterior surface of the ligaments is covered by a fine, continuous, smooth lining membrane. The ligaments are thin, broad and long in the cervical region, thicker in the thoracic and thickest at lumbar levels. They arrest separation of the laminae in spinal flexion, preventing abrupt limitation, and also assist restoration to an erect posture after flexion, perhaps protecting discs from injury.
The morphology and histology of the ligamentum flavum has been studied in the thoracolumbar region. On a macroscopic level, it has two layers, superficial and deep, whose fibres run in opposite directions. On a microscopic level, the ligamentum flavum has predominantly elastic fibres. The superficial layer is innervated by a medial branch from the dorsal root of the corresponding spinal nerve. The deep layer is innervated by sinuvertebral nerves.
Interspinous ligaments connect the facing edges of consecutive spinous processes, and extend ventrally as far as the ligamentum flavum and dorsally to the supraspinous ligament, when this ligament is present (see below). They differ structurally in the thoracic and lumbar levels.
The thoracic interspinous ligaments are narrow and elongated, whereas those at lumbar levels are thick and quadrilateral, and occur as closely applied pairs, the left and right ligaments being separated by a narrow or potential cleft. In the lumbar ligaments, collagen fibres run obliquely inferiorly and ventrally, and only the deepest fibres are truly ligamentous. The more dorsal fibres are derived from tendons of longissimus thoracis that dip into the interspinous space to gain attachment to the superior edge of the spinous process rather than to its tip.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here