Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The International Association for the Study of Pain (IASP) continues to deliberate the classification of chronic pain as a disease symptom or etiology. Semantics aside, pain is undoubtedly a public health crisis as the Institute of Medicine’s report estimates that over 100 million American citizens are living with chronic pain. Of this group, chronic low back pain is the most prevalent, and this diagnosis more than doubles a given patient’s healthcare expenditures. Besides the higher costs to society, numerous adverse social, emotional, and financial consequences befall the individual patient.
Radiculopathy is a syndrome of neurologic conductive loss (sensory or motor) arising from any compressive force on the nerve root. Radiculopathy is not uniformly associated with radicular pain. Radicular pain, or pain in the distribution of a spinal nerve, is a consequence of inflammation driven by glial production of cytokines and is sometimes termed radiculitis to emphasize the inflammatory component of the disease state. , Diagnosing radicular insult as the putative source of pain can be challenging, as neither magnetic resonance imaging (MRI) nor physical examination findings correlate precisely with symptom severity or response to treatments.
From primary care physicians to spine surgeons, most clinicians concur that conservative non-interventional management is the best initial approach. Because the natural history of radiculopathy secondary to disc herniation is favorable, the goal of successful treatment of radicular pain is to reduce pain and restore function while minimizing risk or harm to the patient. Many guidelines exist to guide nonsurgical best practices, , all of which concur that physical therapy and/or structured exercise programs and oral analgesics should be first line treatments. When these fail, the next step in the management of low back or radicular pain is often epidural steroid injection (ESI).
From 2000 to 2014, the number of injections billed to the United States Medicare system increased to 2.2 million per year. Although total lumbar interlaminar ESI (IL-ESI) and caudal epidural injections decreased by 2% per 100,000 Medicare beneficiaries, this was offset by a 609% increase in lumbar transforaminal ESIs (TFESIs) and 93% increase in cervical epidural steroid injections (CESI) per 100,000 Medicare beneficiaries. Although operative (e.g. spine surgery) management is still far more expensive, two-thirds of non-operative (e.g. ESI) costs can be attributed to spine imaging rather than injection therapy.
Early ESI studies were replete with methodologic deficiencies. Many observational studies were encouraging and were only followed by randomized controlled trials (RCTs) that demonstrated no clinical benefit of the evaluated procedure. The heterogeneity of studies performed in the lumbar, thoracic, or cervical space further complicates the evaluation of overall epidural efficacy given the anatomic differences between regions of the human spine.
ESIs for treatment of radicular syndromes appear, at the very least, to transiently improve pain. In the short term, ESIs may also have a surgery-sparing effect. As always, patient selection is the most important component of any successful interventional procedure, and providers should carefully assess the patient’s history, physical examination findings, and imaging results. This is quite feasible in theory, but the uncertainty surrounding nonsurgical best practices, including concern for serious complications of ESIs, , , poses a significant challenge for interventional physicians offering epidural steroid injections to patients.
In 1934 Mixter and Barr were the first to suggest that intervertebral disc herniation might be responsible for radicular pain via mechanical compression on the exiting spinal nerve root. Four years before this hypothesis germinated, Evans proposed treating sciatica with injections of 120 mL of 2% procaine via the trans-sacral canal. Decades later, in 1951, Lindahl and Rexed examined resected dorsal nerve roots from patients with radicular pain and found lymphocytic infiltration and edema, suggesting that inflammation is responsible for radicular symptoms.
Early work in the post-WWII era on injectable corticosteroids (CSs) was a Nobel Prize-winning effort that culminated in the synthesis of the drug hydrocortisone. Soon after, CSs were used in joint injections, and in 1952 Robecchi and Capra reported the first ESI. In the subsequent year, Li’evre et al. described a case series of 20 patients with positive results from epidurally administered hydrocortisone.
Between 1960 and the late 1980s, interlaminar and caudal approaches to the epidural space predominated, largely via non-image guided techniques using surface landmarks and “loss-of-resistance” techniques. In 1988 a study found that a large percentage of these “blind” epidural injections were either not in the epidural space or were not communicating with the target area of nerve inflammation. In a subsequent review, Johnson and colleagues described 5,489 consecutive image guided injections that resulted in only four complications and only ten patients requiring sedation, thus reassuring providers that ESI procedures could be performed on an outpatient basis. They proposed the use of an epidurogram of contrast dye that allowed more accurate localization within the epidural space while also demonstrating that the injectate reached the target area. In 1986 Benzon discussed the efficacy of ESIs for low back pain and nerve root irritation. He noted that patients with acute radicular pain have better results than those with chronic pain. Although ESIs are most widely performed for radicular pain, they may also be used to treat spinal cysts, spinal fractures, and postherpetic neuralgia and are among the most common procedures performed in pain clinics.
Key factors in the provocation of radicular symptoms include mechanical compression of the spinal nerve root or inflammation due to proinflammatory mediators such as prostaglandins and cytokines. CSs, through their anti-inflammatory effects, reduce these inflammatory changes in or around the nerve, thereby decreasing pain and improving function. ,
The nociceptive neural fibers in the outer third of the annulus fibrosus are small unmyelinated C-fibers activated by peptidergic neurotransmitters such as calcitonin gene-related peptide and substance P. In discography-proven pain-generating discs, these nerve fibers sprout farther into the disc, usually accompanied by neovascularization and further degradation of the disc matrix. This de novo innervation appears to originate from the vertebral end-plate region, which may be the progenitor of the pathologic pain attributed to the disc itself. , Modic changes at the end-plate correlate with radiologic spine degeneration but may not have an association with axial or extremity pain. The disc is relatively avascular, and therefore cellular fuel enters and waste exits via passive diffusion. Homeostatic attempts by the body to improve disc nutrition may explain why new blood vessels (and associated nerve fibers) invade the injured disc from the vertebral end-plate region.
The processes that lead to disc degeneration may ultimately lead to disc herniation. Herniated nucleus pulposus results in the local release of cytokines and other inflammatory mediators that cause chemical radiculitis. Burke and associates found increased levels of the inflammatory cytokines interleukin (IL)-6 and IL-8 in disc material taken from patients with known disc disease. Cytokines tumor necrosis factor-α (TNF-α), IL-1α, IL-1β, IL-6, and IL-17 are also thought to promote extracellular matrix degradation, chemokine production, and changes in the intervertebral disc (IVD) cell phenotype, all of which can lead to degeneration of IVD tissues. Olmarker et al. found that the application of disc material onto spinal nerve roots induced functional and morphologic changes in these nerves. In addition, disc cells express TNF-α, which, when applied to spinal nerve roots, causes similar changes to those observed after the application of disc material. , Selective inhibition of TNF-α reduces the intraneural edema seen in this context, lending further credence to the theory that exposure of the nerve root to disc material can be responsible for radicular pain irrespective of anatomic perturbation.
The approaches used to access the epidural space include interlaminar, caudal, and transforaminal. Published studies and guidelines generally agree that all three approaches afford similar clinical benefits but differ markedly in complication rates. For all injections, the patient was placed in the supine position, the skin was cleansed with a chlorhexidine-based solution unless contraindicated, draped in a sterile fashion, and the skin and subcutaneous tissues along the proposed needle trajectory were anesthetized with 0.5%–2% lidocaine. Non-particulate steroids are increasingly used for transforaminal injections due to the risk of arterial thrombosis from particulate steroid introduction. The procedure should be aborted if paresthesia or cerebrospinal fluid aspirate occurs, and these risks will be discussed in greater detail later in the chapter.
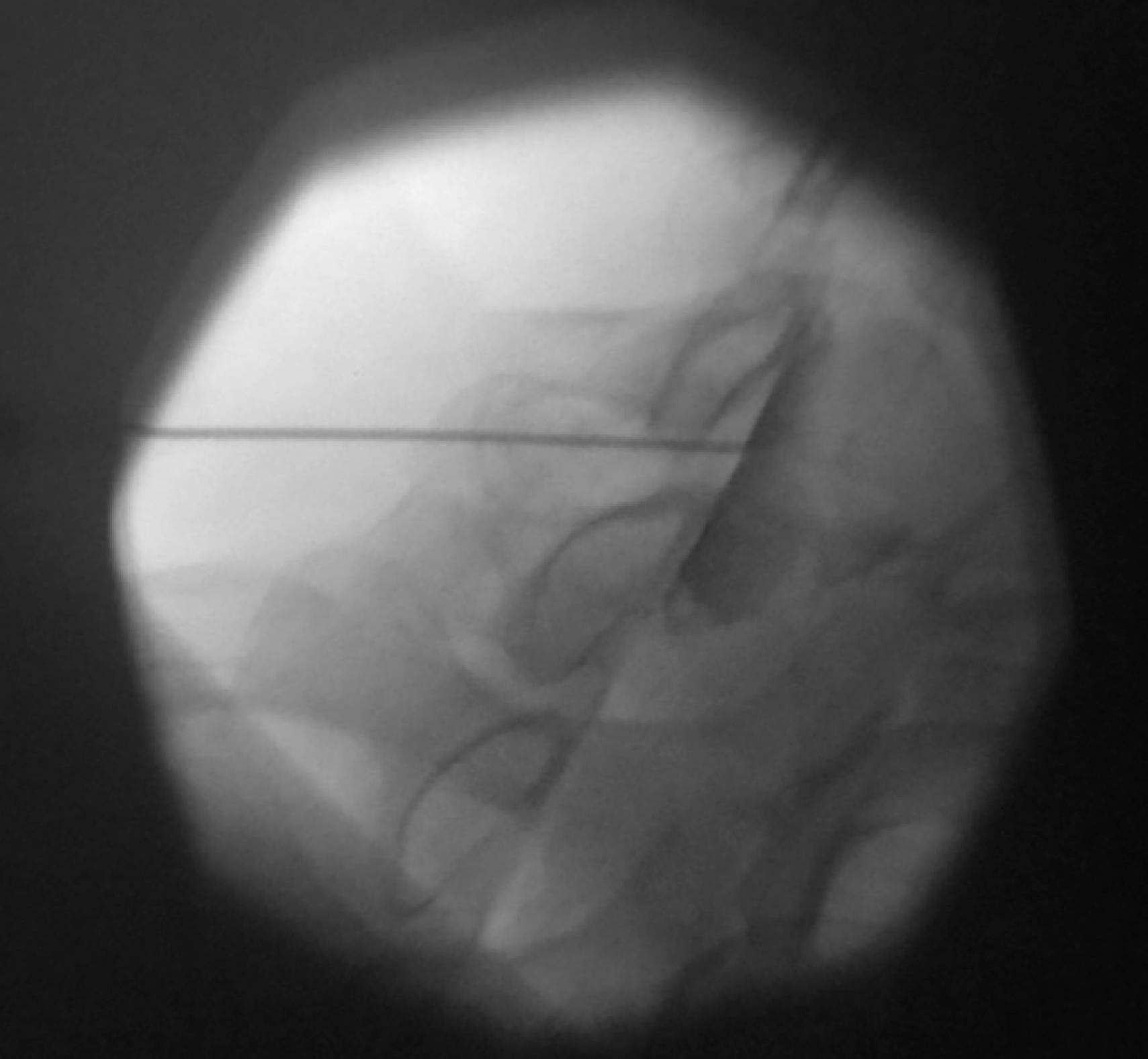
An oblique lateral radiograph is adjusted to maximize the breadth of the intervertebral foramen with the superior articular process (SAP) visualized as a straight line at the posterior aspect of the foramen. A spinal needle was advanced to contact the SAP in the posterior foramen. From the SAP, the needle is “walked off” into the posterior aspect of the foramen, superior to the midpoint. The proceduralist ensures that the needle tip remains superior to the midpoint of the posterior foramina, that is, above the midsagittal plane of the cervical articular pillar in anteroposterior (AP) view, to protect against vascular injury of critical arteries located in the inferior half of the posterior aspect of the intervertebral foramen ( Fig. 65.1 ). , Local anesthetic (LA) test dosing may be used to rule out arterial location of the needle tip, and digital subtraction imaging should be used to substantiate the absence of vascular uptake prior to CS administration. Although we discuss this technique in this chapter, extreme caution must be applied, and rigorous patient selection and consent are required as the risk of vascular penetration at the cervical level is associated with high morbidity and even mortality.
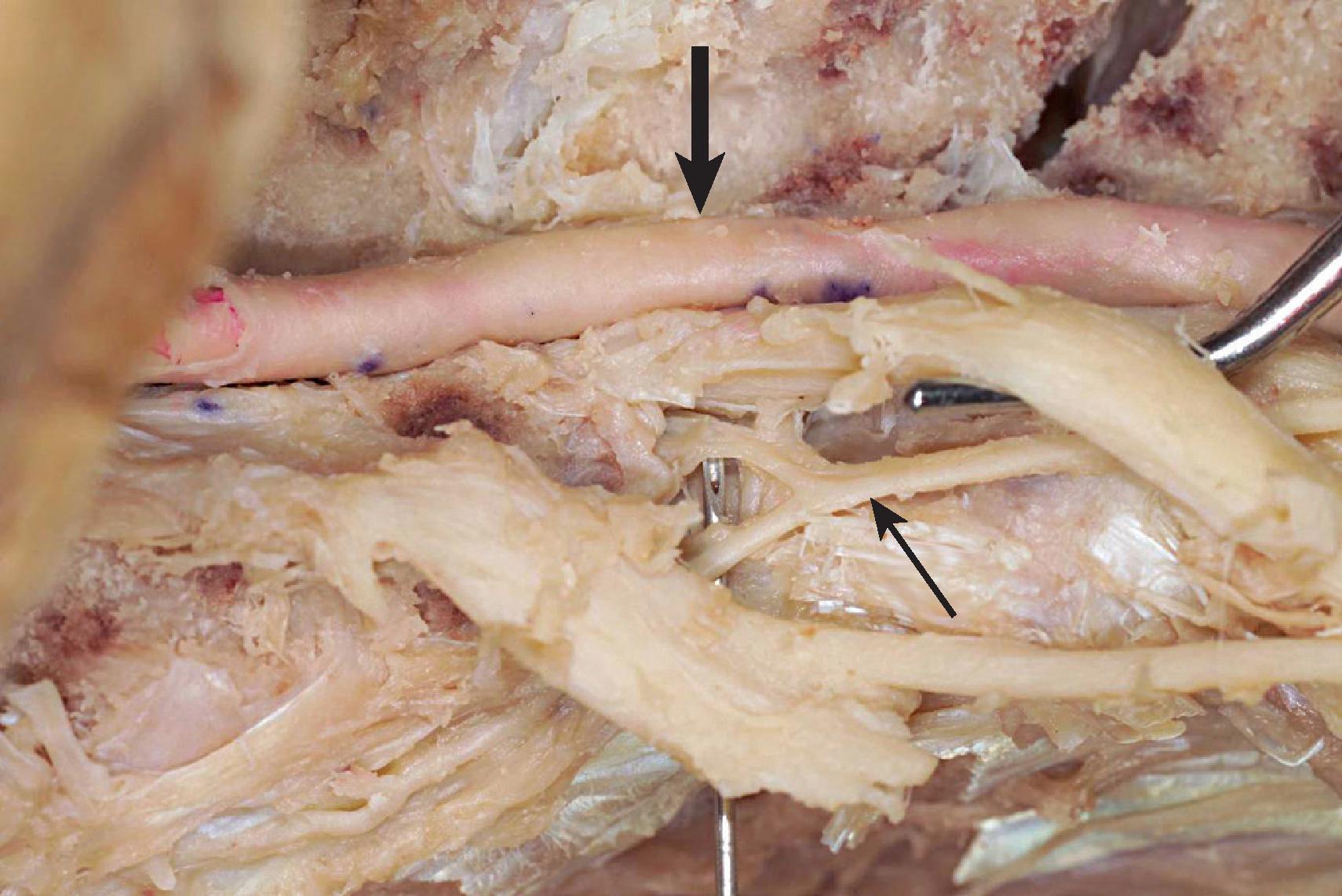
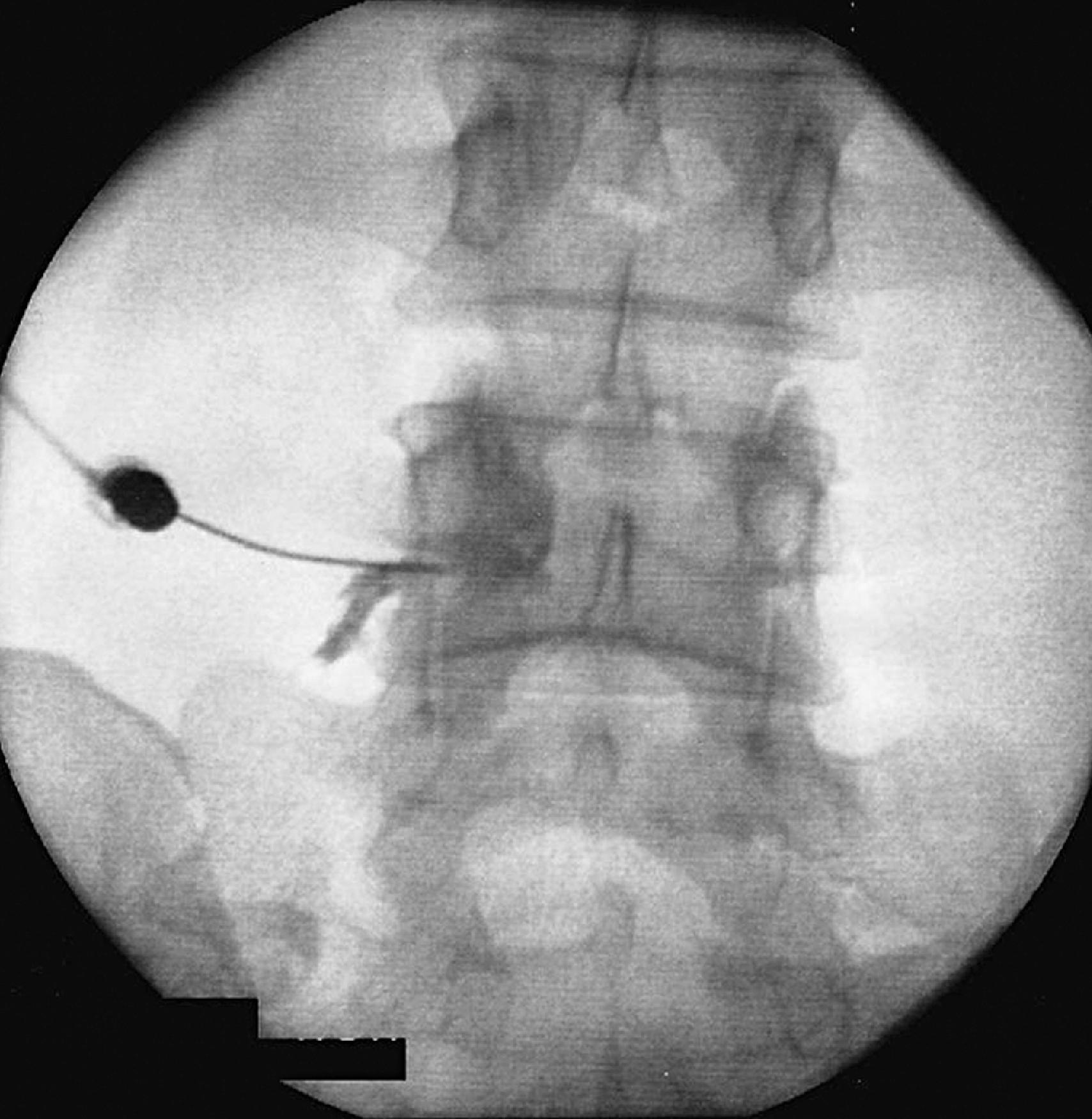
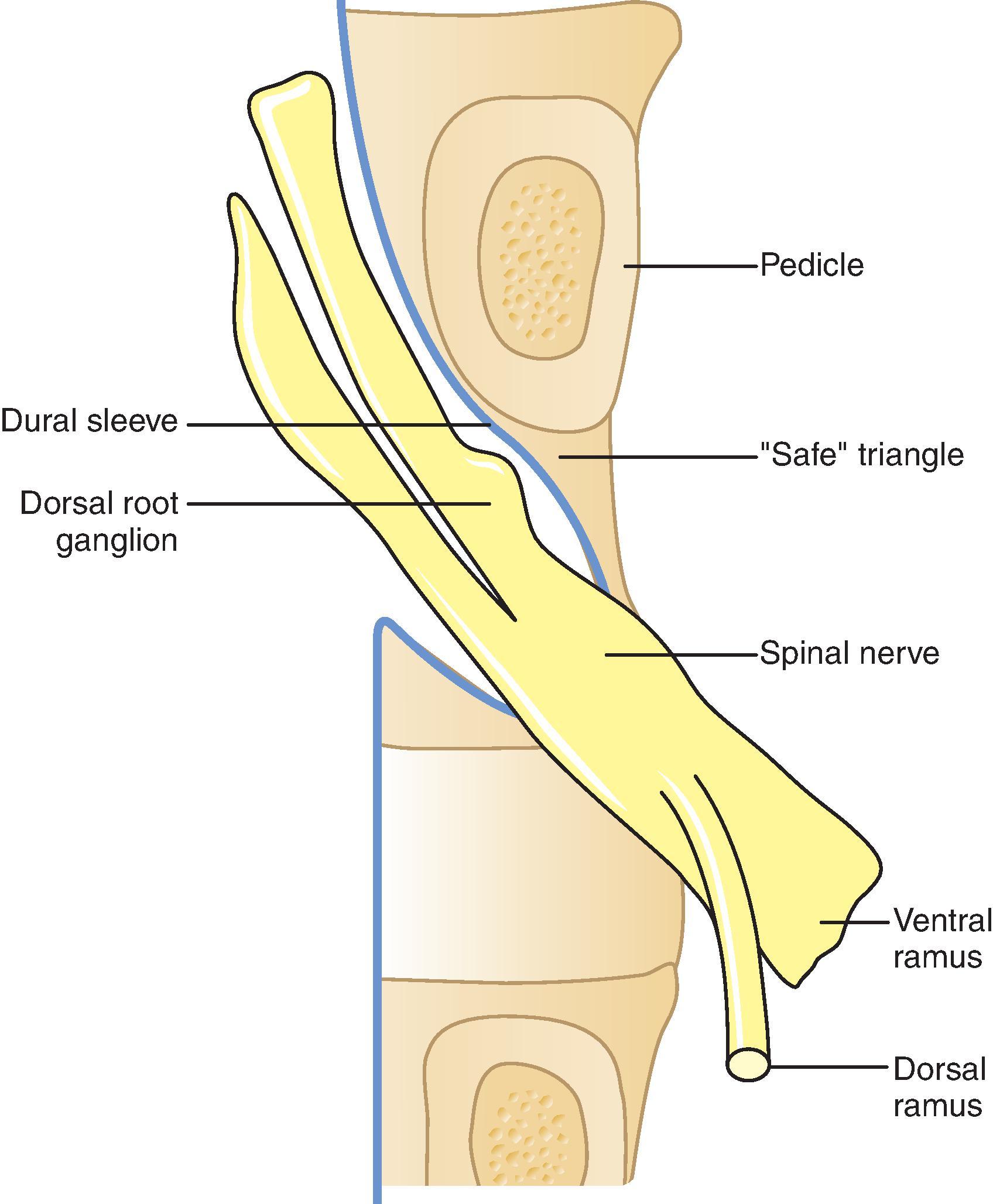
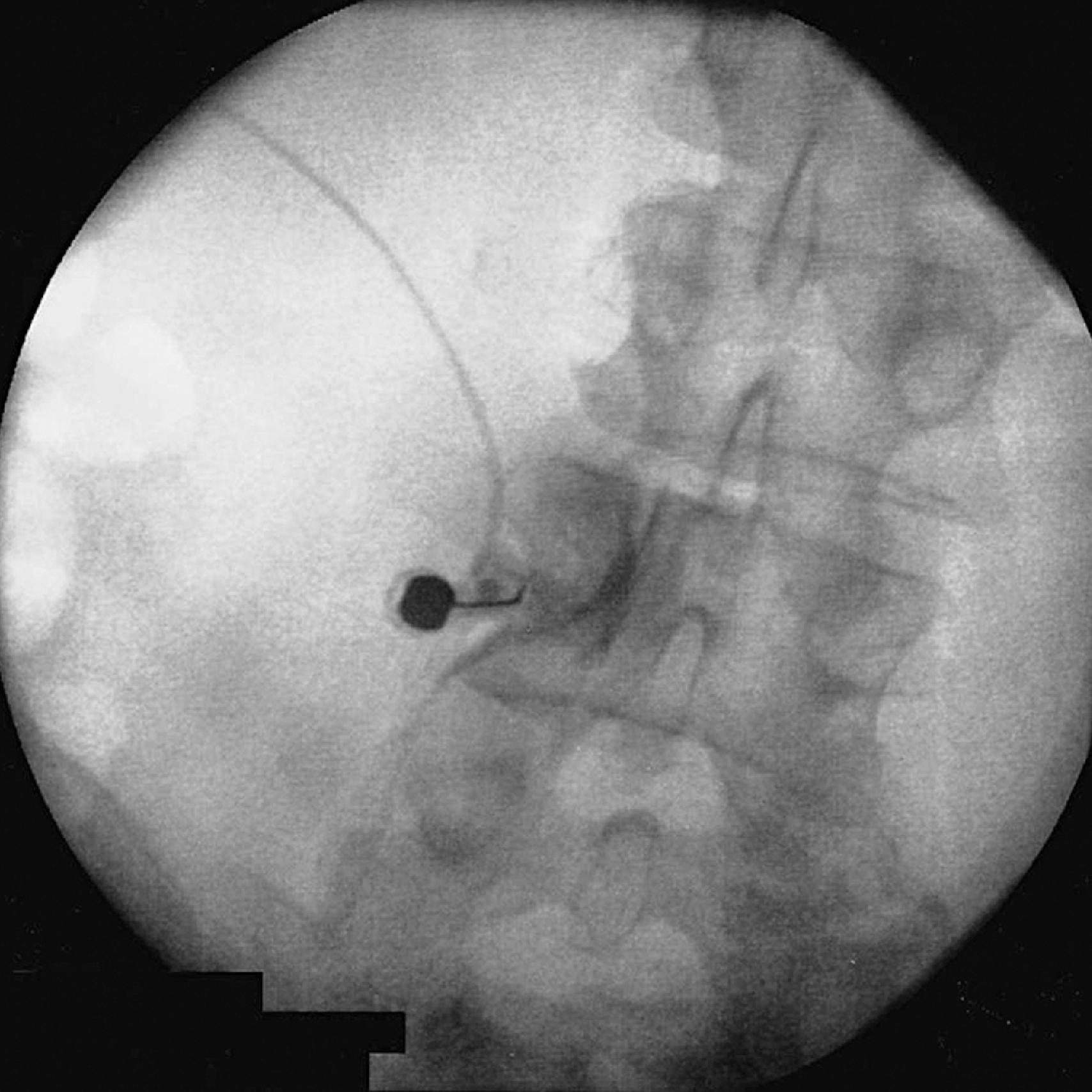
An oblique view is obtained from the lateral surface of the SAP and marked at the six o’clock position along a line that bisects the sagittal plane of the pedicle ( Fig. 65.2 ). Either a cutting-type needle or a blunt needle with a side port opening may be used; some authors contend that a blunt needle may be less apt to enter blood vessels. The needle is advanced incrementally in one of three approaches: the sub-pedicular, the “safe triangle” as proposed by Bogduk and Cherry, or the Kambin triangle ( Fig. 65.3 ). There was no difference in the amount of contrast dye required to visualize epidural spread based on the approach. Injection of contrast medium should demonstrate a neurogram and medial spread into the epidural space ( Fig. 65.4 ). Digital subtraction imaging is useful to substantiate the absence of vascular uptake ( Fig. 65.5 ) as a LA test dosing to detect arterial administration of CSs.

This is most safely performed at the C7-T1 or T1-T2 levels, as the posterior epidural space is 1.5–2 mm greater at these levels than at more superior cervical levels. It is also prudent to review a patient’s MRI prior to the procedure to ensure that the epidural absolute distance is greater than 10 mm at the proposed injection site. , Caudocephalad angulation of the fluoroscope is used to visualize the interlaminar opening in maximal diameter, and an epidural needle is advanced toward the inferior laminar bone at the target level. After contact with the inferior lamina, the needle is walked superiorly until the needle is superior to the lamina. At this point, a loss-of-resistance (LOR) syringe is attached, and the needle is advanced with the operator correlating the tactile LOR technique with a fluoroscopic view of the lateral or the increasingly popular contralateral oblique orientation ( Fig. 65.6 ). Resistance to pressure increases as the needle moves toward the anterior extent of the spinous processes, and a subtle LOR will be detected as the tip enters the epidural space, after which contrast dye and CS may be injected. Occasionally, there are discontinuous areas of the ligamentum flavum in the cervical epidural levels, causing the LOR to be more subtle than in the inferior vertebral levels. An alternative technique uses a needle advanced at a 45-degree angle until the epidural space is accessed, after which a catheter can be threaded cephalad through the needle to the target level.
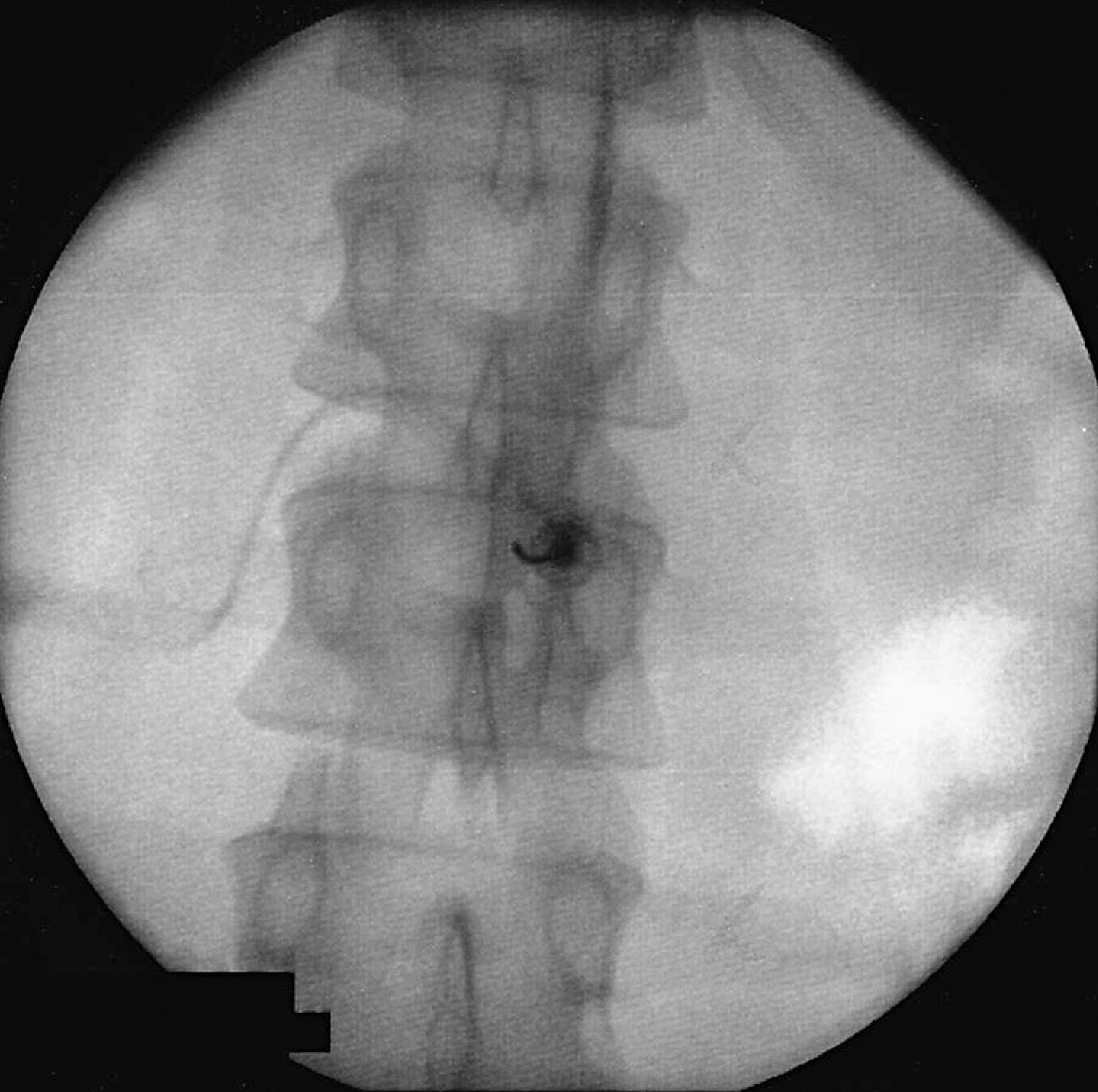
An epidural needle is advanced toward the interlaminar vertebral target, and the epidural space is identified using the LOR technique. The interventional physician may choose to traverse the ligamentum flavum and enter the epidural space in the lateral fluoroscopic view to ensure appropriate placement. Contrast dye demonstrating an epidurogram in both AP ( Fig. 65.7 ) and lateral fluoroscopic views provide support for correct needle placement, after which CS may be administered.
Many techniques have been described for accessing the epidural space via the sacral hiatus. Both cutting and blunt-tipped needles can be used for access, and the procedure can be performed blindly or with fluoroscopic or ultrasonographic guidance. The caudal ESI may be performed in patients even after posterior spine instrumentation and is therefore often used for post-surgical patients that will not have a reliable LOR with an interlaminar approach but also have stenosed foramina that cannot safely accommodate a TFESI.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here