Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A wide variety of congenital, developmental, and acquired abnormalities may affect the pediatric spine. The decision for surgical intervention must be tailored to the disease pathology as well as each patient’s clinical situation. Spinal instability may be iatrogenic or caused by the disease process, requiring installation of spinal instrumentation. Placing instrumentation in the pediatric spine is challenging given the small anatomy of a child, lack of “pediatric-specific” instrumentation, and, at times, inability to adapt adult techniques to the pediatric patient.
This chapter discusses some posterior and anterior spinal instrumentation techniques used in the pediatric spine. Posterior instrumentation techniques are far more widely used than anterior techniques. Advantages and disadvantages of various biomaterials used in the pediatric spine are discussed. Lastly, we briefly discuss the effect of spinal instrumentation on a growing spine, a problem unique to the pediatric population.
Most of the limitations of occipitocervical fixation systems reside in the cranial part of the construct. , The occiput does not easily accommodate instrumentation. The slope of the occipital bone and the angle it makes with the cervical spine impose unique geometric constraints. In addition, the thickness of the occipital bone in children is approximately 3.8 mm compared with 6.7 mm in adults. These limitations may lead to poor occipital screw purchase, screw loosening, pullout, breakage, and difficulties with screw insertion, culminating in catastrophic hardware failure.
Numerous methods of obtaining occipitocervical stabilization have been described, including the use of methylmethacrylate, onlay bone graft with wires, contoured rods with wires, metal plates with wires or screws, contoured rod with either screws or hooks at the occipital level, and occipital condyle screws. , Internal fixation is advised to guarantee postoperative stability and to enhance the rate of arthrodesis. We will be focusing on the occipital screws insertion techniques and nuances here.
In a biomechanical investigation of occipital screw pullout strength, the bicortical pullout strength was found to be 50% greater than unicortical; wire pullout strength was not significantly different from that of unicortical screws, although some authors find a posteriorly wired contoured rod less likely to provide a good fusion environment because of less stabilizing potential and greater potential and greater likelihood of loosening with fatigue.
Although bicortical screw placement may result in superior holding strength secondary to greater cortical purchase, caution is needed to avoid overpenetration and potential neurologic injury. Bicortical occipital screw insertion risks dural laceration, cerebrospinal fluid (CSF) leakage, dural venous sinus injury/thrombosis, and subdural/epidural hematoma formation. CSF leakage and sinus bleeding can be stopped with placement of the occipital screws; if a screw cannot be placed, bone wax may be used to plug the drill hole in the bone.
Bicortical screw failure is directly related to screw length, and screw length is dictated by bone thickness. Because the occiput is thickest in the region of the midline keel, multiple bicortical fixation points directed toward the midline have been advocated.
Like much of pediatric spine surgery, instrumentation techniques are adapted from the adult spine surgery experience. Careful preoperative study of a thin-cut computed tomography (CT) including the occiput is mandatory to confirm enough midline bone thickness to accommodate the shortest 6 mm occipital screw inserted obliquely.
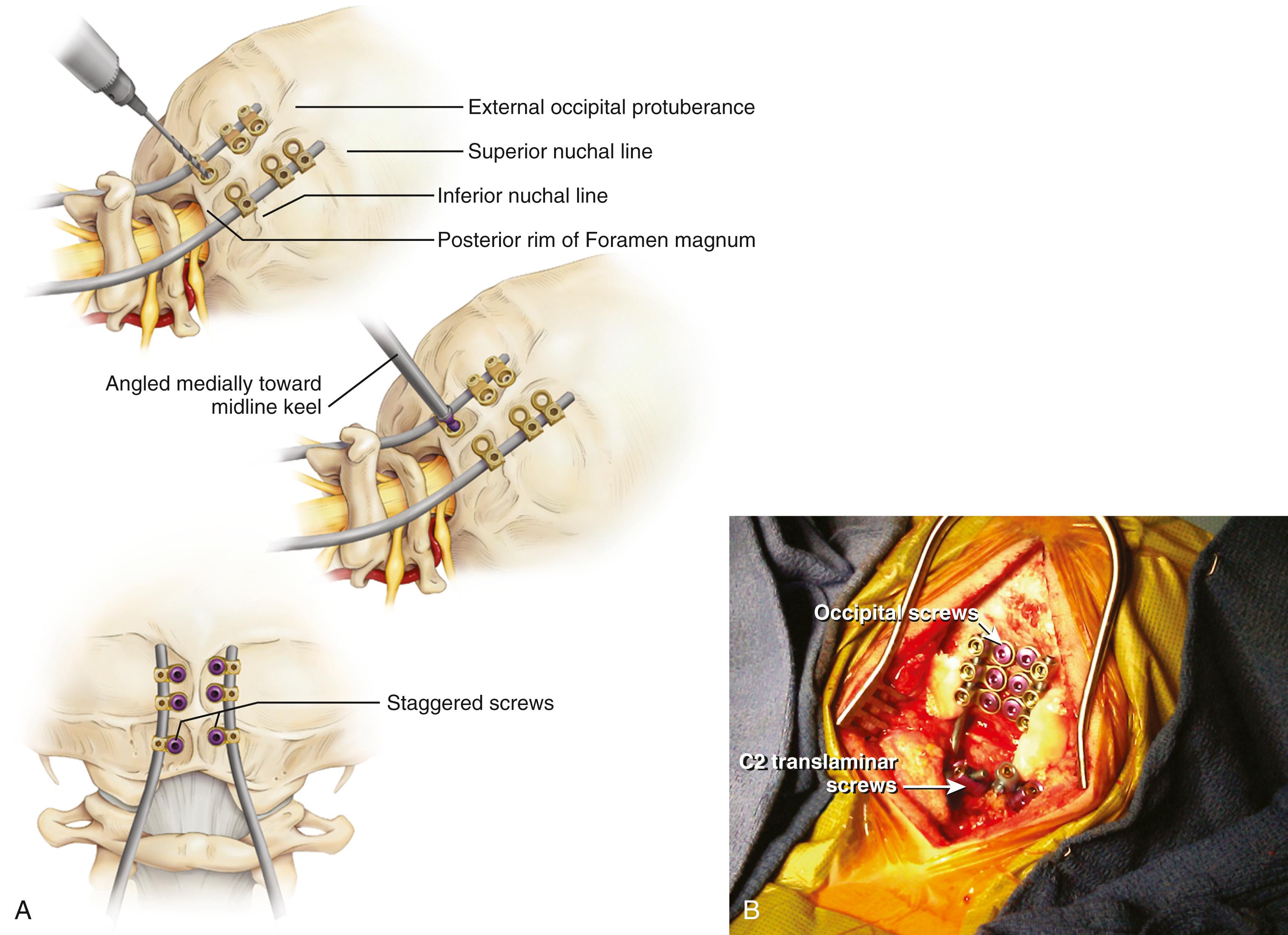
The basiocciput below the external occipital protuberance and posterior to the foramen magnum represents the squamous portion and is the site of occipitocervical fusion. Screw fixation is more secure in the bone above the inferior nuchal line because bone below this landmark is thin. Screw purchase is improved closer to the superior nuchal line and external occipital protuberance. However, the superior nuchal line does not reflect the location of the transverse sinus accurately, ranging from 15 mm below the superior nuchal line and 17 mm above. Unicortical screw purchase at and above the superior nuchal line may be warranted to decrease risk of dural venous sinus penetration.
Careful drilling with triangulation toward midline should be performed millimeter-by-millimeter until the inner table of the occiput is breached; the dura should be palpable with a ball-tipped probe. This “stop-drill” technique is routinely used. With left- and right-sided screws directed toward midline, screw paths may intersect causing even more unwanted difficulty with screw placement. It is useful to stagger the screws on each side of midline, being conscientious to direct the next screw trajectories slightly more cephalad or caudad away from the previous trajectory ( Fig. 78.1 ).
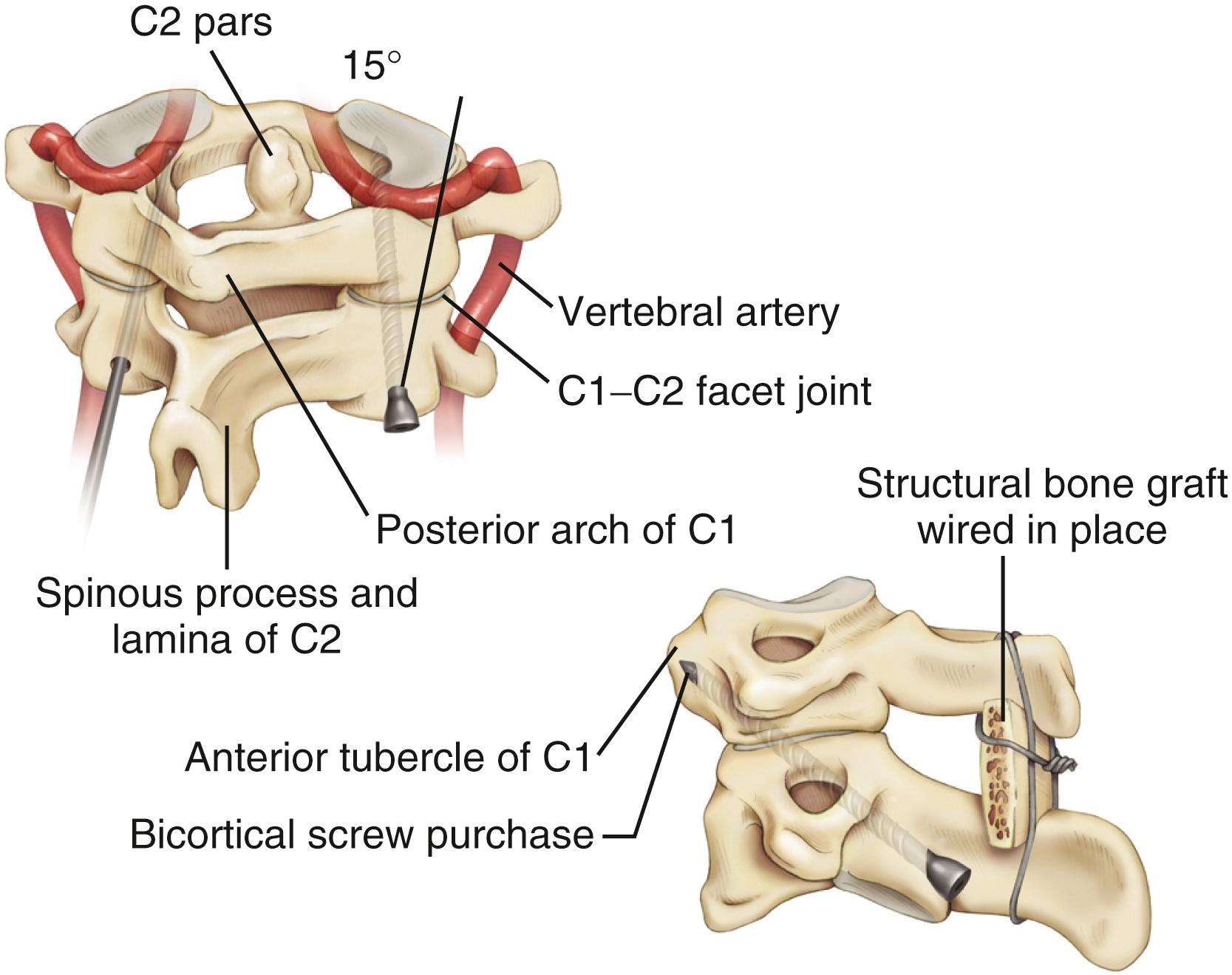
Transarticular C1-2 screws as described by Magerl provide a very rigid and biomechanically sound construct with the incorporation of four cortical surfaces, but the insertion procedure is technically demanding because of the danger of vertebral artery injury, especially in cases where atlantoaxial subluxation remains irreducible preoperatively. Although successful transarticular screw fixation of the atlantoaxial complex has been extensively reported in adult series, there have been only a handful of reports in the pediatric population. Analysis of clinical experience in the largest series of pediatric patients suggested a 4% rate of vertebral artery injury during screw placement; none of these injuries resulted in any long-term morbidity or mortality ( Fig. 78.2 ).
Because of the anatomic limitations complicating transarticular screw placement in adults and even more so in children, variations of C1-2 screw fixation have been reported in adult patients in whom independent C1 lateral mass screws and C2 pars/pedicle screws were connected with either a plate or a rod. Atlantoaxial screw-rod fixation has been suggested as a safer procedure, and perhaps, as we have found, the technique is applicable in more patients despite anatomic variations, even in the smallest of pediatric patients. It is an ideal technique to fix and reduce occipitoatlantoaxial deformities that remain irreducible with closed reduction ( Fig. 78.3 ).
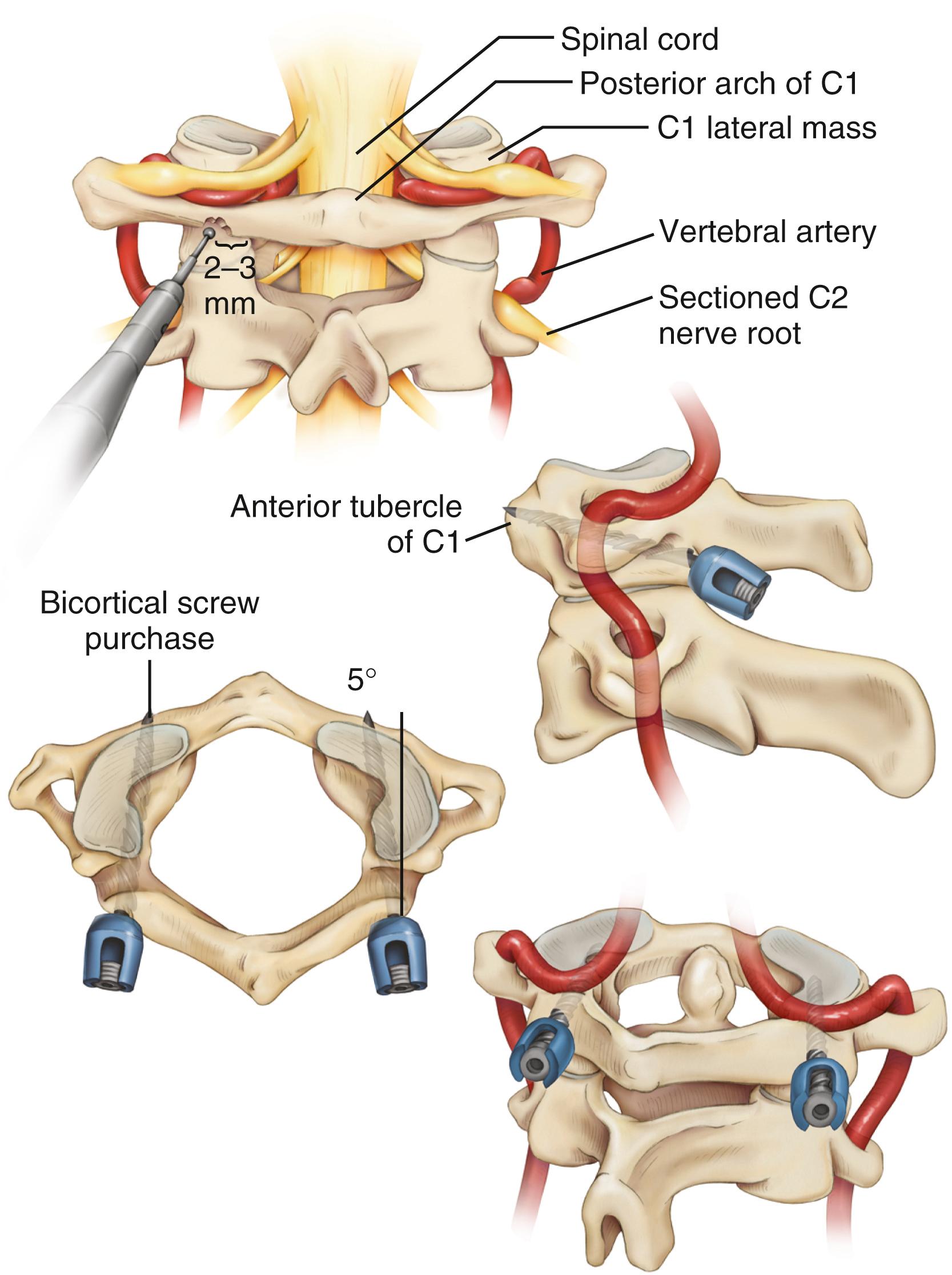
It is imperative that the entry point for the C1 lateral mass screw in the pediatric spine be placed at the confluence of the C1 lamina and the C1 lateral mass. The pediatric spine is unsuitable to accept a C1 lateral mass screw at alternative entry sites, such as the C1 lamina itself because of the high risk of violating the superior wall the lamina and injuring the vertebral artery in the sulcus arteriosus.
It is also important to note how the pediatric atlas differs from the adult atlas. In the adult atlas, the medial side of the C1 lamina is typically flush with the medial C1 lateral mass. However, in the pediatric atlas, the medial aspect of the C1 lamina is typically 2 to 3 mm laterally stepped-off from the medial surface of the C1 lateral mass. An entry point based on the medial aspect of the C1 lamina will place the entry of the C1 lateral mass screw dangerously lateral in extreme proximity to the vertebral artery. Instead, the medial surface of the C1 lateral mass itself must be used as a landmark for starting the C1 lateral mass screw ( Fig. 78.3 ).
Bleeding from the venous plexus around the C2 nerve root can be substantial as dissection down to the junction of the C1 lamina and C1 lateral mass is carried out. This blood loss can be life-threatening in small children without a large blood volume to begin with and may lead to unwanted blood transfusions. Bipolar coagulation of the venous plexus and division of the C2 nerve root may obviate much of this venous hemorrhaging while improving exposure without incurring any significant neurologic sequelae.
Although C1 lateral mass screw placement is still technically challenging and the potential risk of vertebral artery injury persists, our and others experience has shown that it is a feasible, efficacious, and mechanically solid part of an occipitocervical or atlantoaxial screw-rod construct in young patients.
C1-2 transarticular screw placement is technically demanding because of the close proximity of the vertebral artery to the screw path. Vertebral artery injury has been reported to occur in 2% to 8% in several large series. Pars/pedicle screws may have a lower incidence of arterial injury, but these screws still place the vertebral artery and spinal cord at risk.
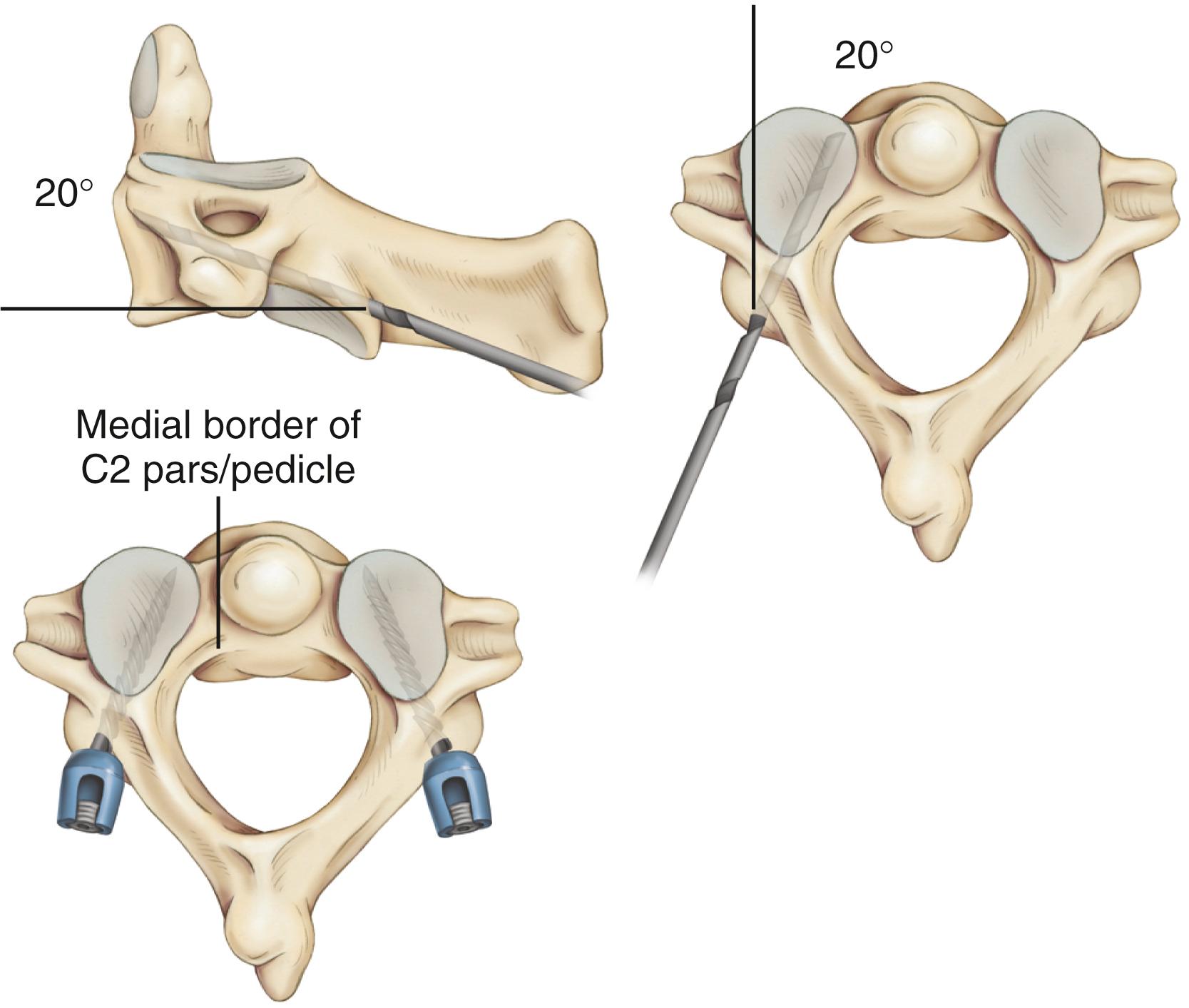
Wright , described the translaminar screw technique that involves rigid screw fixation of the axis by insertion of polyaxial screws into the laminae of C2 in a bilateral crossing fashion and their feasibility for placement in the general adult population. Because the C2 translaminar screws are not in proximity to the vertebral artery, this technique allows rigid fixation of C2 through a safer technique. It has been reported in the literature that this technique of crossing and noncrossing screws is safe and effective C2 fixation in small series of children ( Fig. 78.5 ). Screw constructs are selected on the basis of the patient’s specific atlantoaxial vascular and osseous anatomy, the pathological lesion, and the experience and comfort level of the surgeon. Although a recent meta-analysis of cadaver studies brought concern with the lateral bending stability in C1 lateral mass-C2 translaminar screws, the difference was not statistically significant, and it should be noted that only few studies addressed this particular construct in the literature. From the small series of children and slightly larger patient series in adults using C2 translaminar screws reported in the literature, the follow-up and fusion rate are quite satisfactory.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here