Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The illustrations were drawn by Joseph L. Mills, Jr.
Lower extremity arterial reconstruction is most commonly performed in patients with moderate to severe limb ischemia due to atherosclerotic peripheral artery disease (PAD). Although the techniques described below may also be applied to patients with traumatic, aneurysmal, and nonatherosclerotic conditions, this chapter focuses exclusively on patients with PAD. Infrainguinal bypass is defined as any major arterial reconstruction using a bypass conduit, either autogenous or prosthetic, that originates at or below the inguinal ligament. Inflow sites therefore include the common, deep, and superficial femoral arteries as well as the popliteal or even the tibial arteries. The bypass insertion site may be the femoral, above- or below-knee popliteal, tibial, peroneal, or pedal artery. During the past two decades, progress in patient evaluation and selection and in the conduct of infrainguinal bypass operations has resulted in a more aggressive and generally more successful approach to distal arterial reconstructions, especially for patients with chronic limb-threatening ischemia (CLTI), many of whom would otherwise face major limb amputation. CLTI is a spectrum of disease. Determining whether revascularization is required for wound healing and, if performed, whether open bypass or endovascular therapy is the best initial option is still contentious due to observer bias, widely variable levels of technical expertise and lack of prospective, randomized data to support any given approach. Although graft patency and limb salvage rates have demonstrated continuous improvement, there remains a critical need for detailed clinical studies examining the cost-effectiveness of infrainguinal bypass as well as patient quality of life (QoL) outcomes to ensure the appropriate use of these procedures and to permit meaningful comparison with less invasive endovascular therapies.
The two primary indications for infrainguinal bypass are CLTI and claudication.
Patients who are truly disabled by claudication, such that they are unable to perform their primary occupations or comfortably carry out the activities of daily living, and those whose lifestyles are significantly limited are potential candidates for infrainguinal bypass. A trial of smoking cessation, lifestyle modification, and exercise, with or without medical therapy, is usually indicated before operative intervention (see Ch. 108 , Lower Extremity Arterial Disease: Decision Making and Medical Treatment). There is consensus that bypass is preferable to angioplasty in patients with TransAtlantic Inter-Society Consensus (TASC) type D lesions, that is, complete common femoral artery (CFA) or superficial femoral artery (SFA) occlusions or complete popliteal and proximal trifurcation occlusions; however, bypass may also be applied to patients with types B and C lesions. Operation should be offered only if the benefit-to-risk ratio is high and if anatomic characteristics suggest a favorable and durable result. The primary reason for intervention in claudicants is to improve lifestyle or QoL, given that the risk of severe clinical deterioration (20%) or major limb amputation (5%) during a 3- to 5-year period is low. , In most centers with extensive infrainguinal bypass experience, claudicants constitute only 15% to 30% of patients, with the majority of patients undergoing bypass for CLTI. These data reflect practice patterns in tertiary referral centers and may not reflect the realities of community-based practices.
Patients with advanced CLTI generally require intervention. Such patients previously fell into Fontaine III and IV and Rutherford 4 to 6 categories (see Chs. 107 , Lower Extremity Arterial Occlusive Disease: Epidemiology and Natural History and 108 , Lower Extremity Arterial Disease: Decision Making and Medical Treatment). The most recent European consensus document defines CLI as follows: persistent, recurring ischemic rest pain requiring opiate analgesia for at least 2 weeks and ankle systolic pressure lower than 50 mm Hg or toe systolic pressure lower than 30 mm Hg; or ulceration or gangrene of the foot or toes and ankle systolic pressure lower than 50 mm Hg; or toe systolic pressure lower than 30 mm Hg (or absent pedal pulses in diabetics). Wolfe and Wyatt further subdivided patients meeting the longstanding definition of CLI into critical or subcritical ischemia on the basis of subsequent, observed amputation risk. Subcritical ischemia is present in patients with rest pain and ankle pressure higher than 40 mm Hg. Critical ischemia is defined as rest pain and tissue loss or ankle pressure lower than 40 mm Hg. This distinction is based on a retrospective analysis of 20 publications analyzing 6118 patients. At 1 year, 27% of patients with subcritical ischemia achieved limb survival without revascularization, in contrast to only 5% in the group of patients with critical ischemia. In practice, these data indicate that certain extremely high-risk patients with subcritical ischemia might be managed medically (nonoperatively) but that virtually all patients who are expected to live more than 1 to 2 years with true “critical ischemia” require either bypass or major limb amputation. Because of inconsistencies with terminology and the inappropriate application of the term critical limb ischemia to patients with diabetes, the Society for Vascular Surgery Lower Extremity Guidelines Committee created a more comprehensive threatened limb classification system intended to stratify amputation risk in patients across the spectrum of CLTI. This system is based on objective grades Wound (W), Ischemia (I) and Foot Infection (FI) to calculate a threatened limb clinical stage from 1 to 4 and has been validated in multiple studies to be highly predictive of 1-year major limb amputation risk, including a recent systematic review and meta-analysis. This classification has subsequently been incorporated into the Global CLTI Guidelines, which also include a new anatomic classification system, known as GLASS. GLASS has yet to be validated for infrainguinal bypass.
It is broadly recognized that patients requiring infrainguinal bypass frequently have medical comorbidities, which may include diabetes mellitus, chronic obstructive pulmonary disease, and renal insufficiency; there is a particularly high prevalence of associated coronary artery disease (CAD). The incidence of perioperative myocardial infarction ranges from 2% to 6.5% after lower extremity arterial reconstruction; approximately 70% of both perioperative and late mortality in these patients is due to concomitant CAD. Significant CAD is a nearly universal accompaniment of PAD. What remains controversial is determining which individuals are most likely to benefit from a detailed preoperative cardiac assessment and possible coronary intervention before undergoing infrainguinal bypass. Proposed algorithms have ranged from routine cardiac evaluation of all PAD patients to an almost nihilistic approach.
Patients with CLTI pose a more complex problem because, especially for WIfI Stage 3 and 4 patients, there is a high anticipated amputation rate without lower extremity arterial reconstruction. CLTI patients have an even greater prevalence of CAD than claudicants do as well as a significantly reduced 5-year mortality, primarily due to associated CAD. However, because CLTI patients also tend to be older and have more comorbidities, cardiac intervention in such individuals has higher reported morbidity and mortality rates than in the general population of patients with isolated CAD targeted for intervention. My approach in CLTI patients is to assume they all have significant CAD. Perioperative blood pressure control, anti-anginal regimens, and treatment for congestive heart failure are optimized. I would recommend postponement of infrainguinal bypass in CLTI patients to allow further cardiac evaluation only in the presence of frequent or unstable angina, recent myocardial infarction, poorly controlled congestive heart failure, critical aortic stenosis, or symptomatic/untreated arrhythmia. Even in these instances, the cardiac evaluation should be focused and expeditious. Invasive coronary intervention should be pursued only if patient and anatomic characteristics are favorable, the benefit-to-risk ratio is high, and the delay to perform the limb intervention is not prolonged. In the absence of such cardiac instability, CLTI patients are best treated with meticulous perioperative medical care and expeditious lower extremity revascularization. , Prolonged delays before limb revascularization in CLTI patients increase morbidity and amputation risk. In patients requiring vascular reconstruction, the focus has turned sharply toward maximizing medical therapy rather than performing multiple, expensive, and sometimes ambiguous preoperative cardiac tests so that the patient can be “cleared for surgery.” A large, well-designed prospective randomized trial failed to show a benefit of cardiac revascularization before vascular surgery in patients with stable cardiac symptoms (see Ch. 34 , Preoperative Evaluation and Management).
Infrainguinal bypass requires a careful assessment of arterial disease extent as well as detailed anatomic characterization of the inflow and outflow arteries (see Chs. 27 , Arteriography and 108 , Lower Extremity Arterial Disease: Decision Making and Medical Treatment). Standard arteriography remains the “gold standard” for most patients. Computed tomographic angiography has improved and is now the dominant preoperative imaging modality for aortic aneurysm disease; however, in the periphery, the small caliber of the infrainguinal arteries and the presence of calcification in multiple vessels (associated with increasing age and diabetes) limit the applicability of computed tomographic angiography, especially in CLTI patients. Magnetic resonance angiography is continually improving, and particularly for patients with claudication, preoperative duplex imaging, also referred to as duplex arterial mapping (see Ch. 22 , Vascular Laboratory: Arterial Duplex Scanning), , may provide sufficient anatomic information to proceed directly to the operating room without formal arteriography. In this circumstance, immediate pre-bypass arteriography in the operating room is a reasonable approach. For most patients, however, especially for those with CLTI, I prefer to perform the initial diagnostic angiography in a separate setting, for several reasons. One reason is that for an increasing number of CLTI patients, endoluminal techniques are a reasonable initial option.
On the basis of a careful assessment before angiography, including the indications for intervention, anatomic considerations (based on duplex imaging), and the patient’s functional status, comorbidities, and availability of vein conduit (see Ch. 108 , Lower Extremity Arterial Disease: Decision Making and Medical Treatment), I try to determine whether a given patient with GLASS III (TASC type C or D) disease would be best served by endoluminal therapy or open bypass. If endoluminal therapy is the preferred option, I vigorously pursue endoluminal treatment at the time of diagnostic arteriography. If open bypass is preferable, I focus on optimal visualization of potential target arteries and obtain multiple views, as required, to ascertain that no unexpected inflow disease is present that would require treatment before proceeding with infrainguinal bypass. Detailed high-quality diagnostic arteriograms can be obtained and reviewed carefully before proceeding with bypass. In some patients, selection of outflow arteries may be difficult, and this area of decision making can be improved if films are reviewed and discussed with colleagues. Confining the initial procedure to diagnostic or therapeutic angiography obviates time constraints and scheduling difficulties that arise in the operating room when trying to perform angiography and open reconstruction in one sitting. I reserve that approach for carefully selected patients whose arterial anatomy has already been fairly well delineated by preoperative magnetic resonance angiography or duplex scanning. This confines the “one-stop approach” primarily to claudicants undergoing bypass for isolated, single-level femoropopliteal disease.
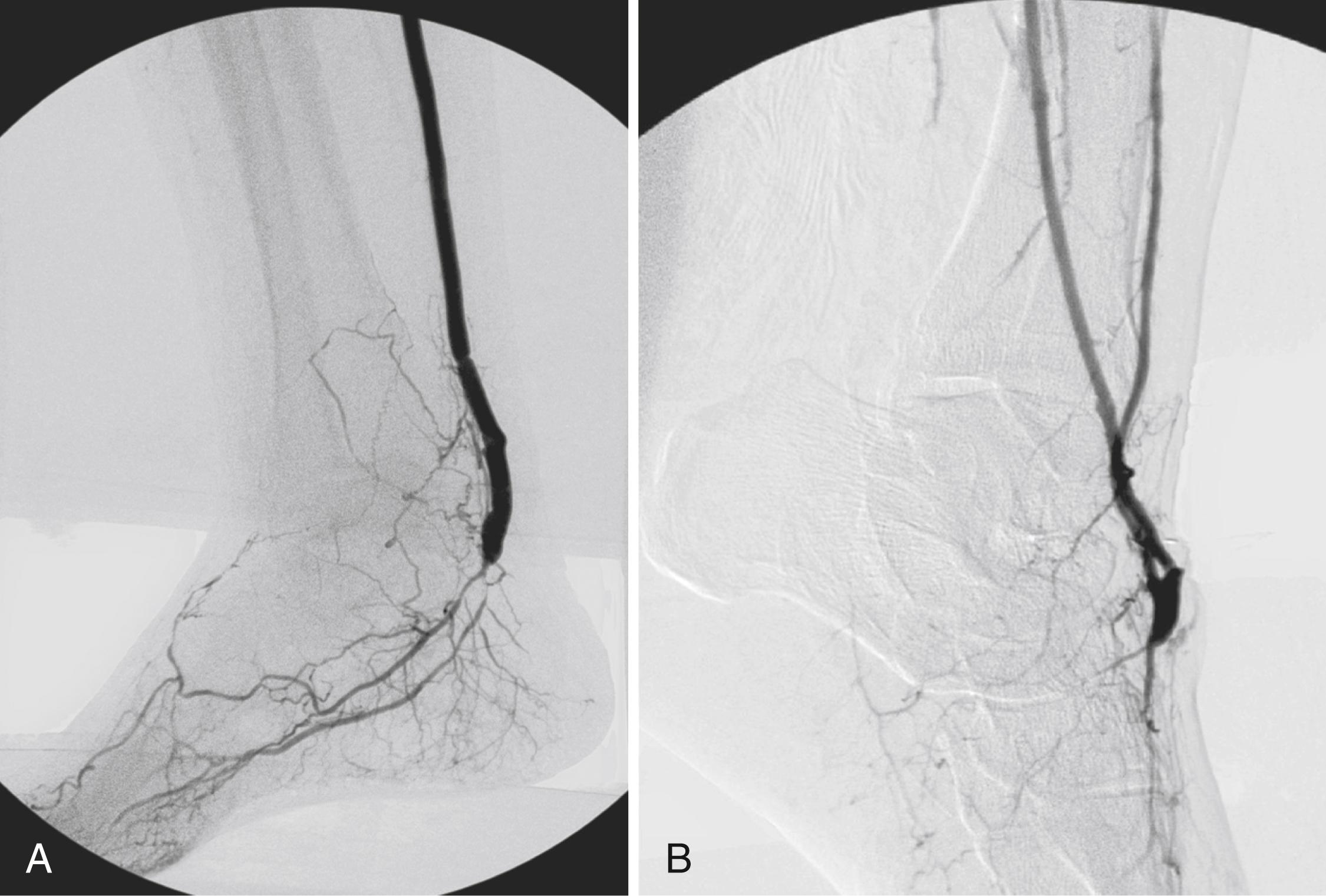
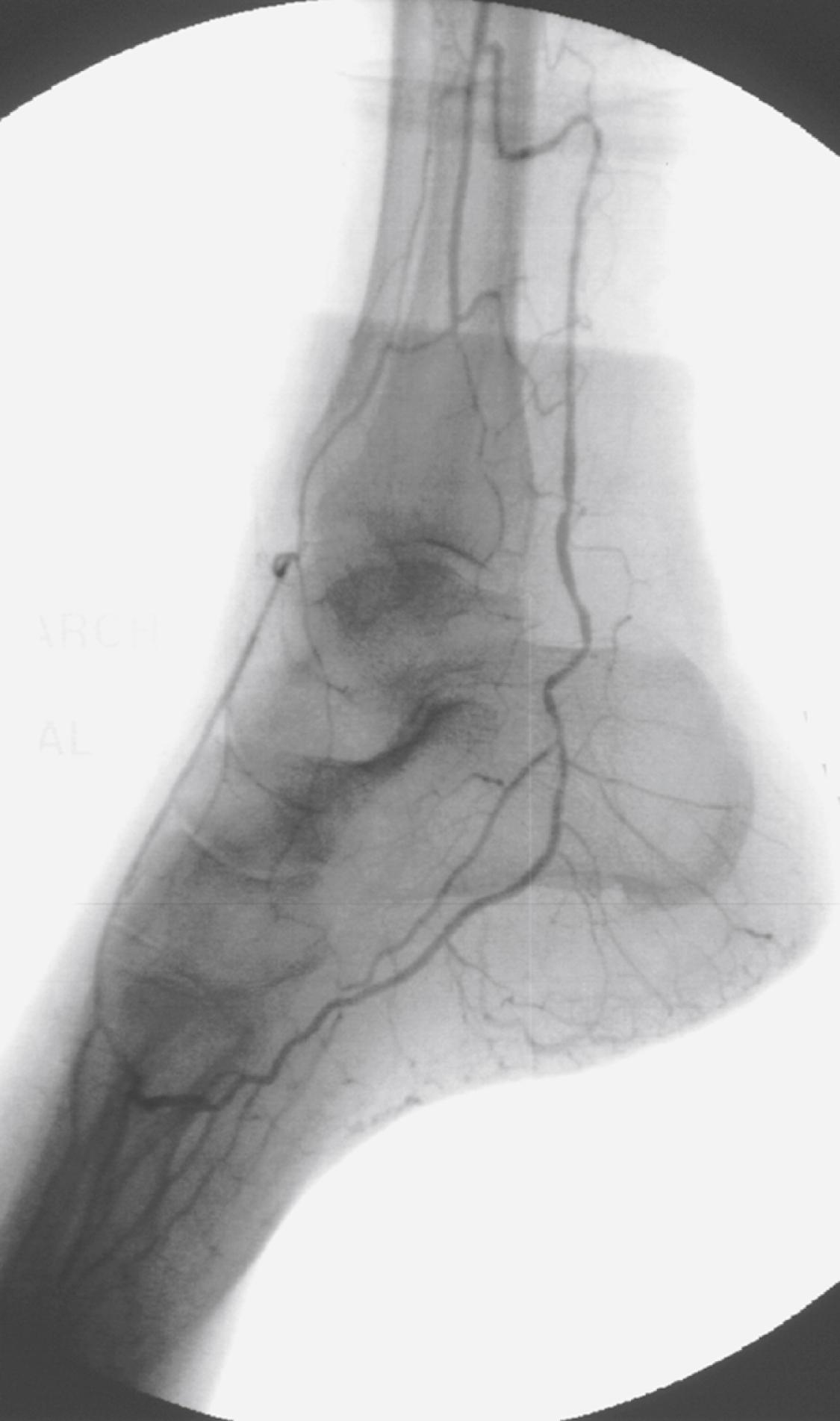
In the vast majority of patients in whom infrainguinal bypass is indicated, suitable target arteries can be identified ( Fig. 112.1 ) if diagnostic angiography is properly performed. , Only a tiny fraction of individuals, usually those following multiple failed reconstructions, have no identifiable target artery. Detailed runoff views are necessary, including magnified lateral views of the foot. Such films can be obtained in nearly all patients with adjunctive techniques such as foot warming, local administration of intraarterial vasodilators, and proper positioning of the diagnostic catheter. It is frequently helpful to advance the catheter selectively into the SFA or popliteal artery to obtain adequate views of the infrapopliteal and pedal circulations, especially in patients with diabetes mellitus. Intraarterial runoff films with bolus injections performed while the diagnostic catheter is positioned in the aorta may fail to adequately define the runoff. If percutaneous access has been achieved from a contralateral, retrograde femoral approach, selective films can be obtained by advancing a wire and an appropriate diagnostic catheter over the aortic bifurcation and selectively down the affected extremity. In selected patients with normal inflow based on physical examination and noninvasive studies, an ipsilateral antegrade approach may be more expeditious to identify suitable runoff vessels, with the additional advantage of requiring a reduced contrast load ( Fig. 112.2 ). Such an approach is especially useful in diabetic patients with renal insufficiency and noninvasive studies that suggest isolated infrapopliteal disease.
Despite optimal angiographic techniques, there may be a small number of patients in whom no suitable target can be identified. Selective exploration of dorsal pedal or distal posterior tibial arteries with flow detectable by Doppler or duplex imaging may identify a graftable recipient artery. Pomposelli et al. reported a surprisingly high success rate under these circumstances, although I believe that this situation is relatively uncommon if diagnostic angiography has been optimally performed. In short, there are relatively few patients who are truly unreconstructible from an anatomic standpoint owing to the lack of a suitable outflow target vessel.
Since Kunlin’s first description of the successful use of autogenous femoropopliteal vein bypass for arteriosclerosis obliterans, , there has been universal agreement that autogenous vein is the best conduit for infrainguinal bypass at all levels. , Great saphenous vein (GSV) is the most readily available and durable conduit. Assessment of vein availability and quality is critical and should be carried out before embarking on the operation. I routinely perform preoperative duplex mapping of the GSV (see Chapter Algorithm). If ipsilateral GSV is absent, unsuitable, or of insufficient length for the anticipated bypass, I also scan the ipsilateral small saphenous vein, the contralateral great and small saphenous veins, and the upper extremity veins, to locate a suitable vein and to be able to deal with any extenuating circumstances that might arise during the conduct of the operation. Patients are scanned with a light tourniquet in place and with the limb dependent, as described by Blebea et al. I prefer to use veins that are soft, compressible, and at least 3 mm in diameter. Calcified or sclerotic veins are rejected. Soft, compressible veins between 2 and 3 mm in diameter are worthy of exploration, but if they do not distend appropriately, the operation should be modified either by harvesting a better-quality vein (based on preoperative duplex studies) or by shortening the length of the proposed bypass, if possible, by selecting alternative inflow or outflow sites. The type and quality of the bypass conduit are the most important determinants of infrainguinal bypass success; efforts to maximize conduit quality will be rewarded.
Vein harvesting can be performed through long continuous incisions, skip incisions, or endoscopically. Endoscopic vein harvest has become common in cardiac surgery. Although there are a few enthusiasts, it has not been widely adopted by vascular surgeons for leg bypass, likely owing to equipment costs, learning curve issues, and concerns about damaging vein segments when a long conduit is needed. There are no convincing data to support any specific harvesting technique. Regardless of the harvesting technique, poor-quality or marginal vein should be rejected. The search for high-quality vein is worth the time and effort, even if vein splicing or bypass shortening is required. Every effort should be made to perform all infrainguinal bypasses with vein conduit (all-autogenous policy). Long-term results should not be sacrificed for the sake of expediency at the initial operation. Saphenous vein performs well in the reversed, nonreversed, and in situ configurations; the technique chosen is dictated primarily by conduit availability, anatomic considerations, and surgeon preference and experience.
Operative planning for infrainguinal bypass requires complex decision making by the vascular surgeon. More than any other operation, infrainguinal bypass taxes one’s ingenuity, and requires the surgeon to anticipate and carefully consider numerous alternatives and potential complications both during preoperative evaluation and in the conduct of the reconstruction itself. Foremost, the major anatomic lesions and their hemodynamic significance must be identified.
Adequate inflow should be ensured before commencing with infrainguinal bypass. Selected inflow lesions can be treated either percutaneously in advance, at the time of preoperative diagnostic arteriography, or at the same operative sitting (hybrid procedure). Iliac artery lesions of hemodynamic significance should be addressed in nearly all claudicants before proceeding with infrainguinal bypass. For patients with CLTI, an iliac lesion with a resting gradient of less than 5 to 10 mm Hg may be acceptable if the pulse and Doppler waveform at the selected inflow site (e.g., femoral artery) are normal. In patients with claudication or CLTI presenting with rest pain alone in the absence of tissue loss (WIfI: W0, I3, fI 0), an isolated iliac angioplasty without concomitant infrainguinal bypass may suffice if the iliac lesion is of sufficient hemodynamic importance. In such patients with tandem lesions, the profunda–popliteal collateral index may be helpful in predicting whether an inflow procedure alone will be sufficient to alleviate the patient’s symptoms. An index greater than 0.25 indicates a large pressure gradient across the knee joint and suggests that inflow disease correction and profundaplasty alone are unlikely to be adequate.
Before operation, the surgeon must define the inflow source; it need not be the CFA. There is abundant evidence that originating shorter bypasses from the deep femoral, superficial femoral, popliteal, or, in rare cases, one of the tibial arteries results in patency rates equivalent to those achieved when the CFA serves as the bypass origin. Short bypasses are frequently useful in patients with diabetes mellitus and primary infrapopliteal arterial occlusive disease as well as in individuals with limited available vein conduit who present after failure of a previous reconstruction. Based upon hemodynamic data and anatomic imaging, the surgeon should commence the operation with the optimal inflow site in mind. However, if unanticipated arterial disease is identified or vein quality and length are worse than anticipated once the operation is under way, the surgeon should have alternative bypass origins in mind that can be used to shorten the bypass length without compromising hemodynamics. If there is uncertainty about the appropriateness of the inflow site at exploration, its hemodynamic suitability can be assessed by direct intraarterial pressure measurements that can be compared with the transduced radial artery pressure. A resting gradient exceeding 10 mm Hg is significant, as is a drop in pressure exceeding 15% after the administration of intraarterial papaverine. , , If a significant gradient is identified at the selected inflow site, a more proximal inflow site above the culprit lesion should be selected, or the responsible lesion should be addressed by local endarterectomy or angioplasty. This problem occasionally arises with iliac or common femoral lesions whose hemodynamic significance was not appreciated at the time of preoperative arteriography, particularly lesions consisting primarily of posterior plaque that may have been masked if appropriate oblique projections were not obtained.
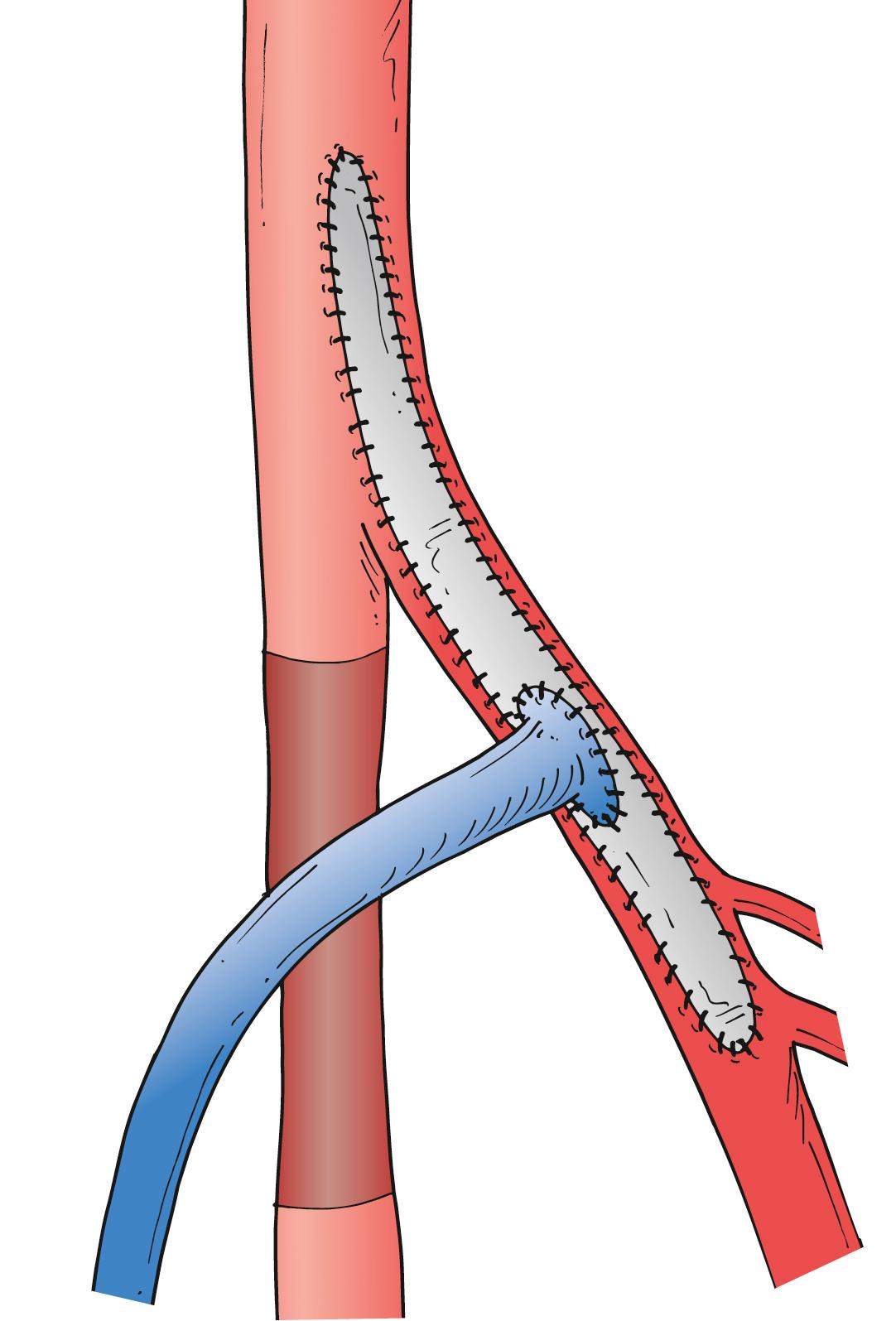
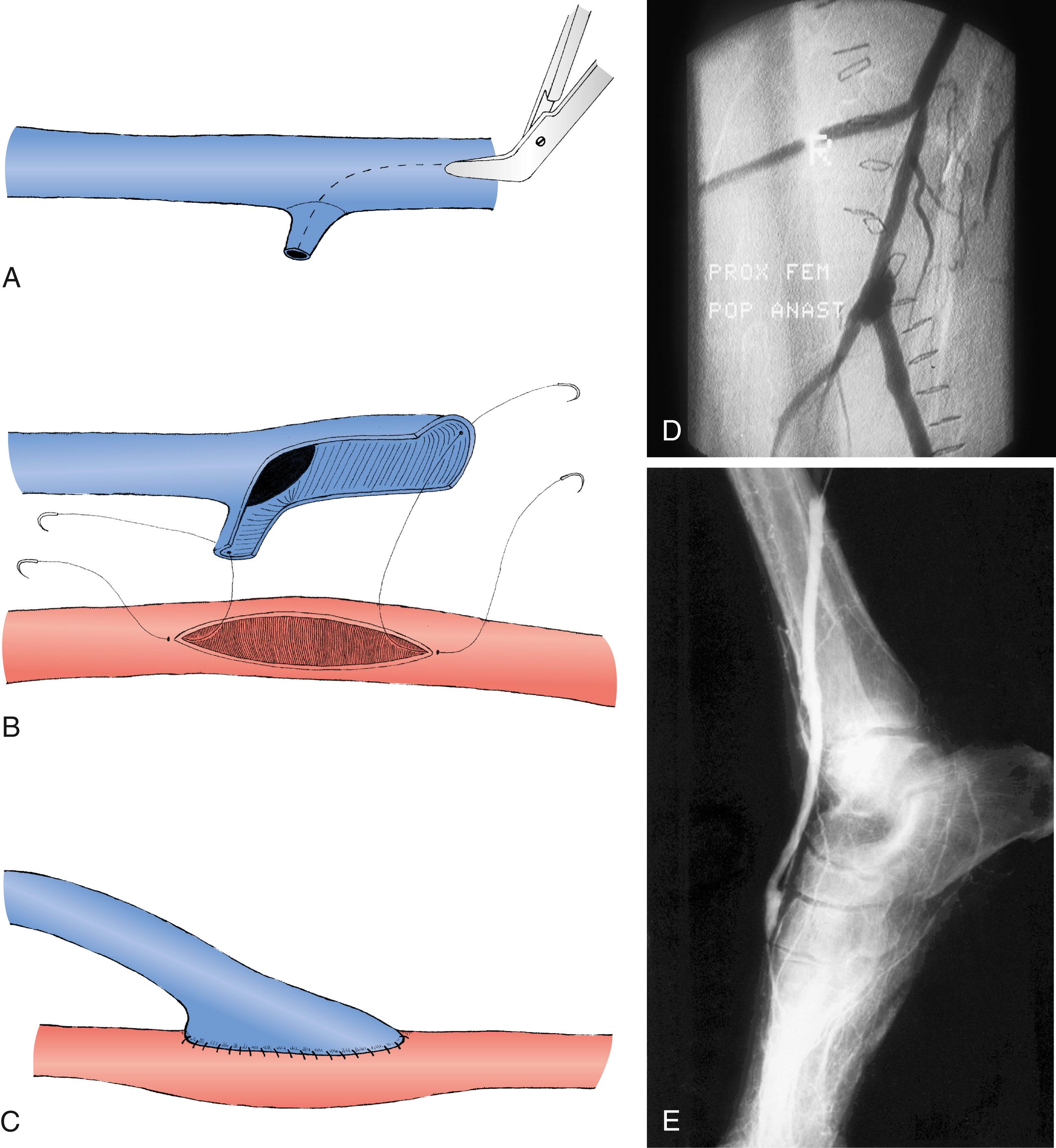
Whenever the CFA is used as the site of origin for bypass, significant occlusive disease involving the origin and proximal deep femoral artery should usually be addressed concomitantly. The endarterectomy often begins in the CFA. After the division of veins that cross the anterior surface of the deep femoral artery, the femoral arteriotomy is carried out beyond the posterior tongue of disease that extends a variable distance down the deep femoral artery, usually at least to its first or second portion. Tacking sutures may or may not be needed at the distal endpoint. The arteriotomy can be closed with a vein patch or a segment of endarterectomized SFA. This patch can then be opened longitudinally to serve as the origin for the infrainguinal bypass (modified Linton patch technique; Fig. 112.3 ). Alternatively, if the vein caliber is excellent (>4 mm), a longer venotomy can be made in the vein conduit, which then serves simultaneously as a profundaplasty patch and the bypass origin; this technique should not be used if the arterial wall is markedly thickened or if the caliber of either the native donor artery or the vein conduit is small to avoid compromising the origin of the vein graft at the proximal anastomotic heel. Incorporation of a venous side branch as part of the anastomotic heel is another useful technique when the donor arterial wall is thick or there is a caliber mismatch between the donor artery and the vein bypass conduit ( Fig. 112.4 ). Correction of significant deep femoral disease at the time of infrainguinal bypass is clinically important; should the bypass ever fail, adequate deep femoral artery perfusion may prevent the development of severe, recurrent limb ischemia.
Although inflow artery selection is generally straightforward, outflow site selection frequently requires greater judgment. The general principle of infrainguinal reconstruction is to bypass all hemodynamically significant disease and to insert the bypass into the most proximal limb artery that has at least one continuous runoff artery to the foot. Thus, if the popliteal artery reconstitutes distal to an SFA occlusion and at least one tibial or peroneal artery is in continuity with the foot, the popliteal artery would be selected as the outflow site. It is possible, however, and sometimes desirable to bypass to an isolated or so-called blind popliteal segment.
An isolated popliteal artery is defined as a patent popliteal artery segment at least 5 cm long but with only geniculate collaterals and no major distal tibial or peroneal runoff artery in direct continuity with the foot. Such bypasses function surprisingly well and are especially useful in patients with limited vein availability. They may also be more useful in patients with claudication or rest pain than in those with frank tissue necrosis, for whom anything less than providing pulsatile flow directly to the foot may be insufficient for healing. In the presence of tissue loss, I prefer bypass to an artery in direct continuity with the foot. Five-year assisted primary or secondary patency rates of 50% to 74% have been reported for such blind-segment popliteal bypasses. Successful bypasses to isolated tibial artery segments have also been reported.
Although most claudicants require only femoropopliteal bypass, a high proportion of patients with CLTI require tibial or pedal bypass. In general, the most proximal segment of tibial or peroneal artery that is continuous with the foot should be chosen as the outflow site. Thus, a patent anterior tibial or posterior tibial artery in direct continuity with the foot and pedal arch would be chosen over the peroneal artery as an outflow site if suitable vein length is available. There is still some controversy about whether one should choose the proximal or mid peroneal artery or a patent pedal artery for patients with tissue loss. Most authors have found no adverse effects on graft patency or limb salvage for peroneal bypasses compared with tibial or pedal bypasses, but Pomposelli and others have made a strong case for pedal bypass, particularly in diabetic patients with tissue loss. They emphasize the importance of restoring a pedal pulse to maximize forefoot reperfusion. The pedal arteries are also more superficial and more easily exposed than the anatomically disadvantaged, deeply located peroneal artery. If the bypass must originate in the groin and the proximal or mid peroneal artery is of good quality on arteriography and has abundant collaterals with the foot (see Fig. 112.2 ), I generally perform a shorter bypass to the peroneal artery, especially if vein conduit length is a limiting factor. If the peroneal artery is diseased or does not appear to collateralize well with the foot, I preferentially bypass to the foot or ankle and splice vein if required to obtain sufficient length. I prefer dorsal pedal or paramalleolar posterior tibial–plantar artery insertion sites for short bypasses originating from the popliteal artery in diabetic patients with tissue loss. Shortening the bypass in such patients allows one to optimize vein conduit quality, and the choice of an inframalleolar target artery maximizes forefoot perfusion.
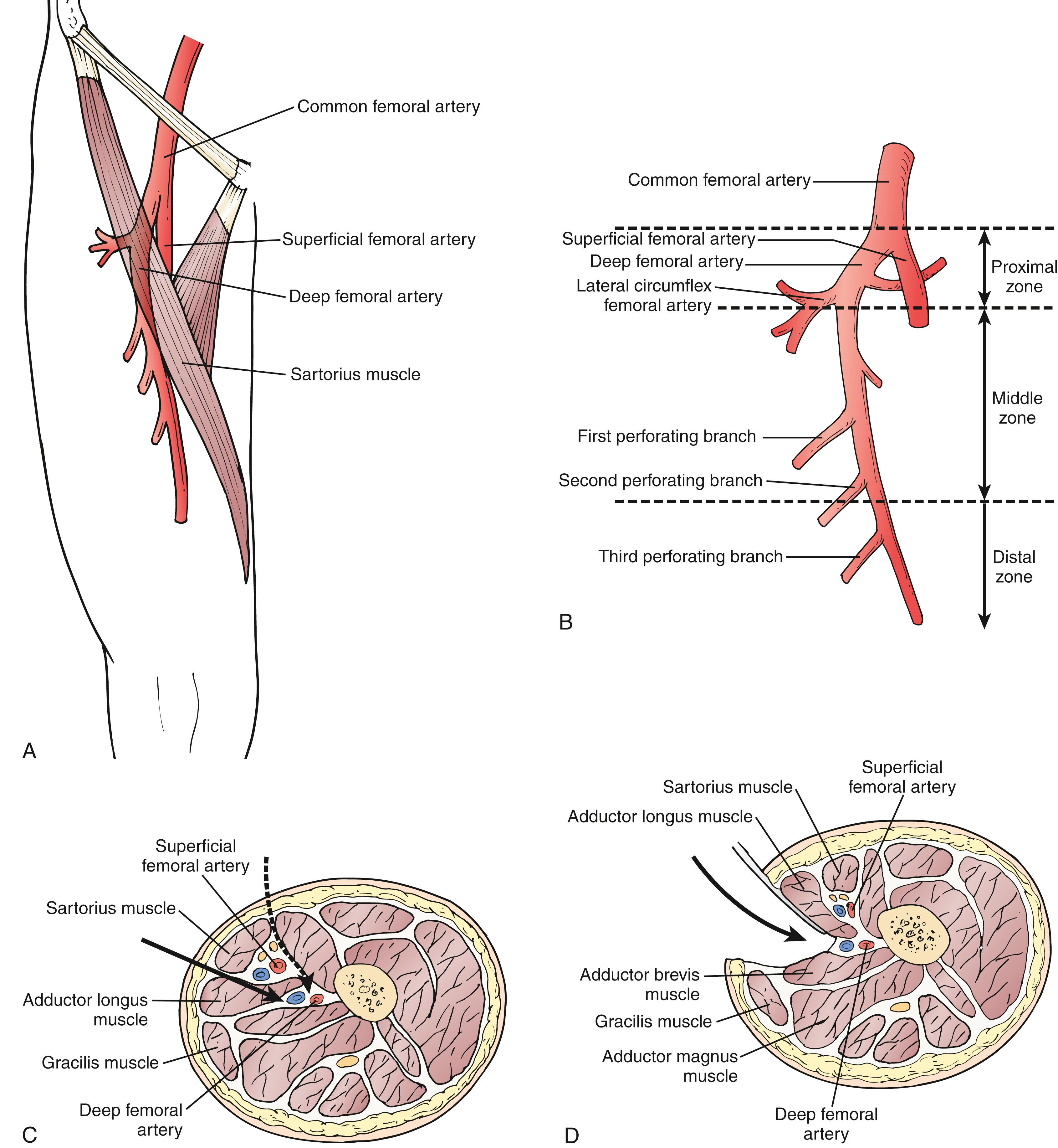
Thorough knowledge of anatomy and facility with multiple surgical exposures are critical to the success of infrainguinal bypass. The standard approach to the CFA and the profunda femoris artery (PFA) is provided by a vertical incision overlying the CFA. This anterior approach allows complete exposure and mobilization of the CFA and its bifurcation; more proximal exposure can be obtained by dividing the recurrent portion of the inguinal ligament or the entire ligament (Peter Martin incision). Distal extension allows exposure of the PFA. Division of the lateral femoral circumflex vein offers access to the proximal PFA; careful progressive division of numerous crossing veins allows extensive exposure of the PFA. In selected patients, alternative exposures have been described.
If previous infection or scarring from multiple previous reconstructions makes standard exposure difficult and if there are no significant occlusive lesions in the CFA or proximal PFA, the mid or distal PFA can be approached laterally, anteromedially, or posteromedially ( Fig. 112.5 ). , The lateral PFA approach is the most useful for infrainguinal bypass. The incision is placed in the upper thigh lateral to the sartorius muscle. The sartorius and SFA are retracted medially. The raphe between the adductor longus and vastus medialis is incised to expose the PFA. This approach is useful when vein conduit length is limited or femoral triangle scarring is prohibitive (hostile groin). The surgeon must be certain that there are no hemodynamically significant lesions proximal to the PFA if this approach is used. With these caveats in mind, use of the PFA origin for distal bypass does not compromise long-term patency. , Similarly, the SFA and popliteal artery can be used as inflow sources in carefully selected patients without compromising graft patency.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here