Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Central nervous system (CNS) infections can be due to multiple pathogens; however, viral and bacterial infections are the most common ( Table 5.1 ). The CNS injury that results from the infection depends on the timing of infection, pathogen, immune response, and medical treatment.
| Developmental Stage | Pathogenic Agents |
|---|---|
| Congenital (Torch) | Viral Cytomegalovirus (CMV) Toxoplasmosis Herpes simplex virus (HSV) Rubella Syphilis Varicella Human immunodeficiency virus (HIV) Lymphocytic choriomeningitis virus infection Zika virus |
| Perinatal | Bacterial Group B Streptococcus (GBS) Escherichia coli Listeria monocytogenes Viral Herpes simplex virus (HSV) Fungal Candidiasis |
| Infants | Bacterial Group B Streptococcus Staphylococcus aureus Escherichia coli Pseudomonas aeruginosa |
| Children/adolescents | Bacterial Haemophilus influenzae type B Streptococcus pneumoniae Neisseria meningitides Mycobacterium tuberculosis |
Viral infections can lead to brain malformations when acquired in utero or lead to meningoencephalitis in infants and children. Congenital infections that occur earlier in pregnancy typically have more severe brain developmental sequelae than those occurring later in pregnancy. Although improvements in laboratory testing have improved detection of viruses, in many viral infections the causative pathogen goes unidentified. Several viral infections are discussed in this chapter, with a focus on those viral infections that cause in utero infections, perinatal infections, and infections later in childhood.
Bacterial infections can lead to meningitis, abscesses, and empyemas and can result in significant injury to the brain. Unfortunately, bacterial meningitis can lead to death in approximately 10% of patients, and survivors remain at high risk for neurologic sequela. Bacterial meningitis is most common in the first year of life, which leads to challenges for clinical diagnosis. Neonates and infants may present with a wide range of nonspecific clinical symptoms of meningitis, including fever, hypothermia, poor feeding, irritability, seizure, and bulging fontanelle. Fortunately, pediatricians are well trained to consider meningitis as the cause of these signs and symptoms and to appropriately perform blood cultures, and lumbar puncture for cerebrospinal fluid (CSF) analysis and culture to diagnose meningitis. Imaging is performed to assess for complications of meningitis, provide supportive evidence of meningitis, and assess for adequacy of treatment. Bacterial meningitis can occur through hematogenous seeding and direct extension from an extracranial source. The bacterial toxins and inflammatory response can subsequently cause complications, including vascular occlusions leading to infarcts, cerebritis, abscess formation, CSF obstruction, and disruption of CSF absorption leading to hydrocephalus.
Atypical infectious pathogens include fungi, tuberculosis, parasites, and amoebic infections. These are much less commonly clinically encountered. They are discussed briefly in this chapter to highlight some features that should alert the radiologist to the potential for an atypical infection.
Neuroimaging is often performed to assess safety of lumbar puncture procedure; identify findings supportive of bacterial meningitis when CSF culture is negative; assess for complications of meningitis, including abscess, empyema, infarct, and hydrocephalus; and to reevaluate the status of a known infection.
Ultrasound, CT, and MRI are commonly used neuroimaging techniques for CNS infections. Ultrasound is often used in neonates and infants when the anterior fontanelle remains open. Ultrasound is useful for following ventricular size; however, other imaging findings are often difficult to identify. Noncontrast CT is often used at initial presentation to assess safety of a lumbar puncture and prevent delay in obtaining CSF and starting antibiotics. CT is also commonly performed to assess complications of meningitis including hydrocephalus. Noncontrast CT and contrast-enhanced CT (CECT) are less commonly performed when MRI is available because of the ionizing radiation and reduced accuracy of CT compared to MRI for detection of findings and complications of meningitis. MRI is the modality of choice for definitive evaluation of intracranial infection. This chapter illustrates the common and uncommon causes of CNS infections in children with emphasis on imaging patterns and helpful clinical features, including the age of the patient.
Cytomegalovirus (CMV) is a member of the herpesvirus family and is acquired by direct contact of mucosal surfaces with the virus via infected body fluids and, similar to other herpesviruses, has the potential for latency and reactivation.
Congenital CMV is the most common congenital viral infection in children and most common cause for nongenetic sensorineural hearing loss.
Maternal-fetal transmission is primarily due to a primary maternal CMV infection, which has a 32% risk of transmission compared to 1% with recurrent CMV infection. Primary maternal infection results in greater number of symptomatic infants.
Approximately 10% of congenital CMV infections are symptomatic at birth. Clinical findings include hepatosplenomegaly, petechiae, jaundice, small size for gestational age, microcephaly, sensorineural hearing loss, seizure, and chorioretinitis. Laboratory studies include thrombocytopenia, elevated liver transaminases, and elevated direct and indirect bilirubin.
Long-term neurologic outcomes include cerebral palsy, developmental delay, intellectual disability, sensorineural hearing loss, seizures, and vision impairment.
Sensorineural hearing loss is present in 33% to 50% of symptomatic infants, has a delayed onset in 18% to 30%, and is bilateral in 71% of symptomatic and 43% of asymptomatic infants. Progressive hearing loss occurs in 18% to 63% of patients, and hearing loss becomes severe to profound in 78% of affected ears.
Timing of infection during pregnancy correlates with the severity of disease.
Presence of abnormal imaging findings portends abnormal neurodevelopmental outcome.
Confirmed diagnosis is made by detection of CMV with polymerase chain reaction (PCR) or shell vial culture of newborn saliva, or urine within 3 weeks of birth. Intrauterine infection may be diagnosed with PCR of amniotic fluid.
Treatment with antiviral medication may improve hearing and developmental outcomes.
Normal fetal MRI and normal fetal neurosonology are good predictors of favorable neurodevelopmental outcome.
Third trimester or perinatal infection may result in an anatomically normal appearing brain.
Fetal MRI is superior to fetal US, especially regarding dysplasia and myelination abnormalities.
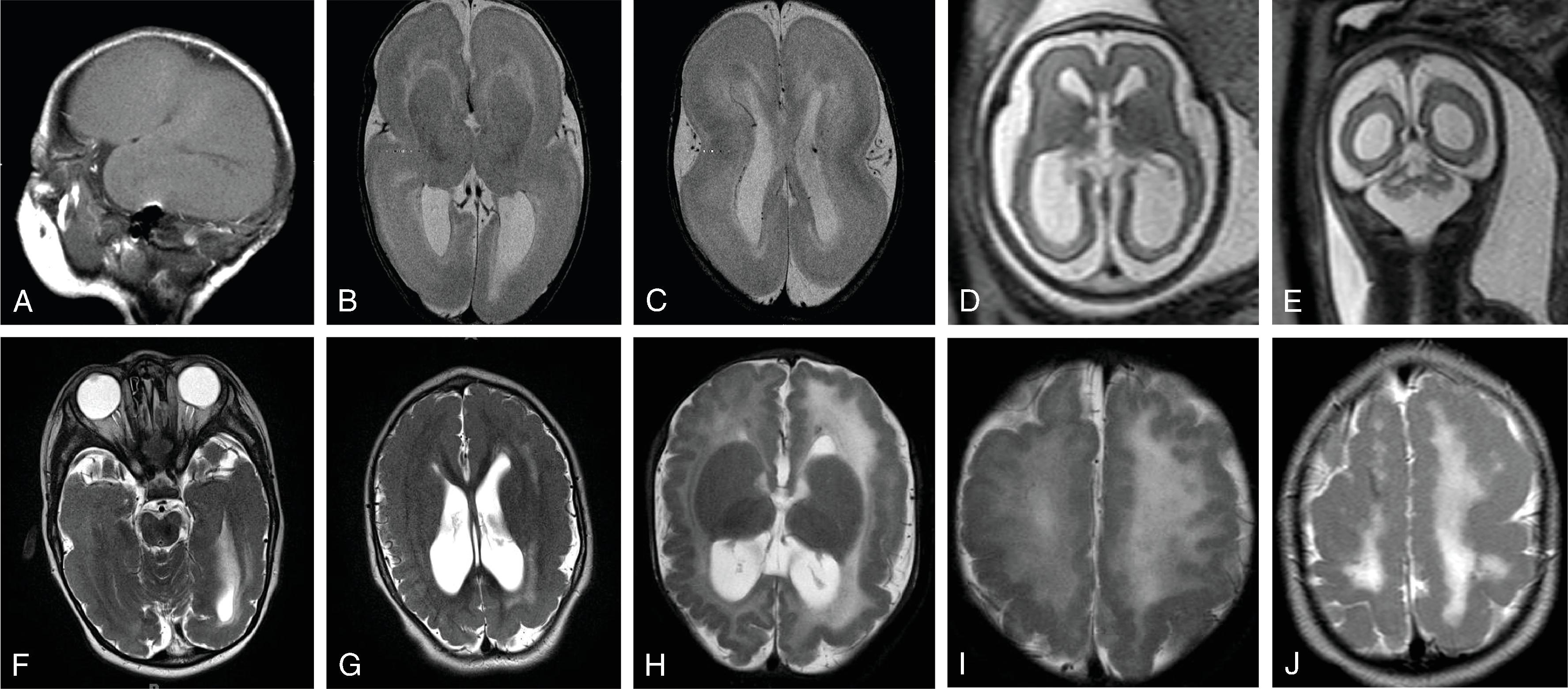
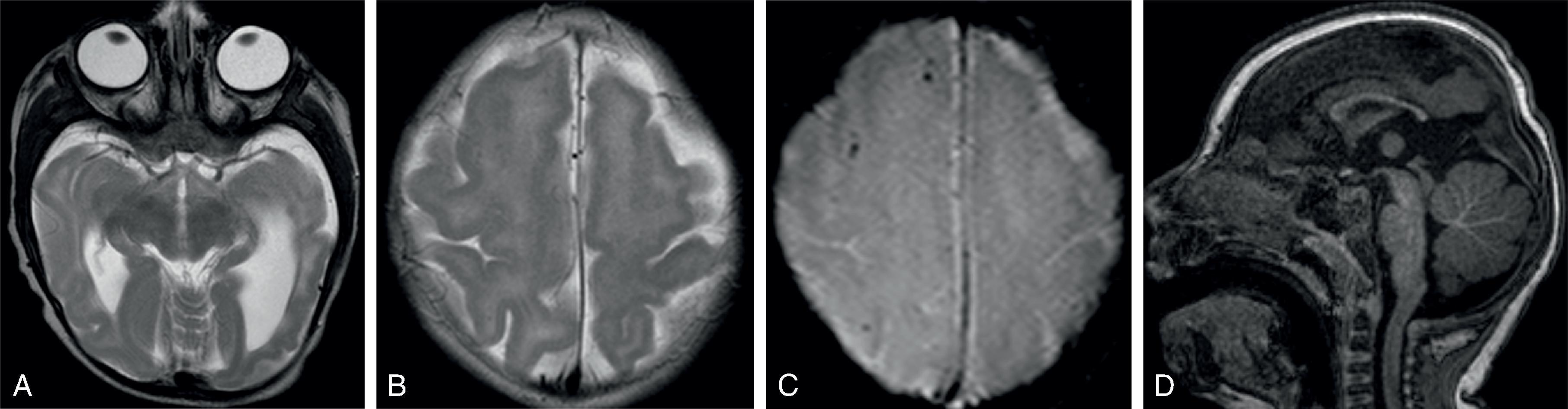
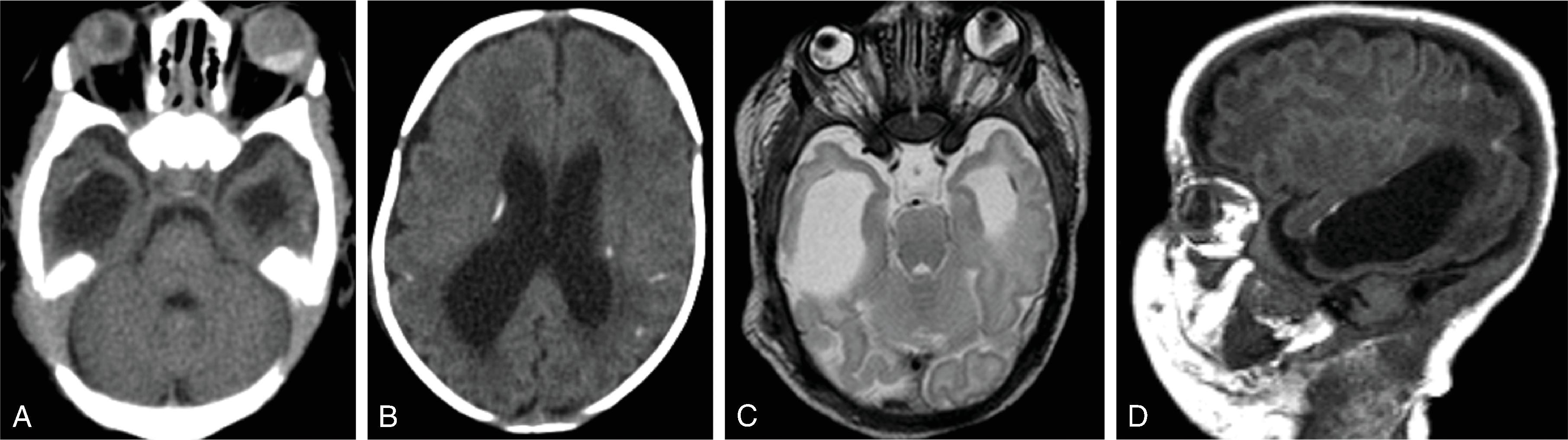
MRI
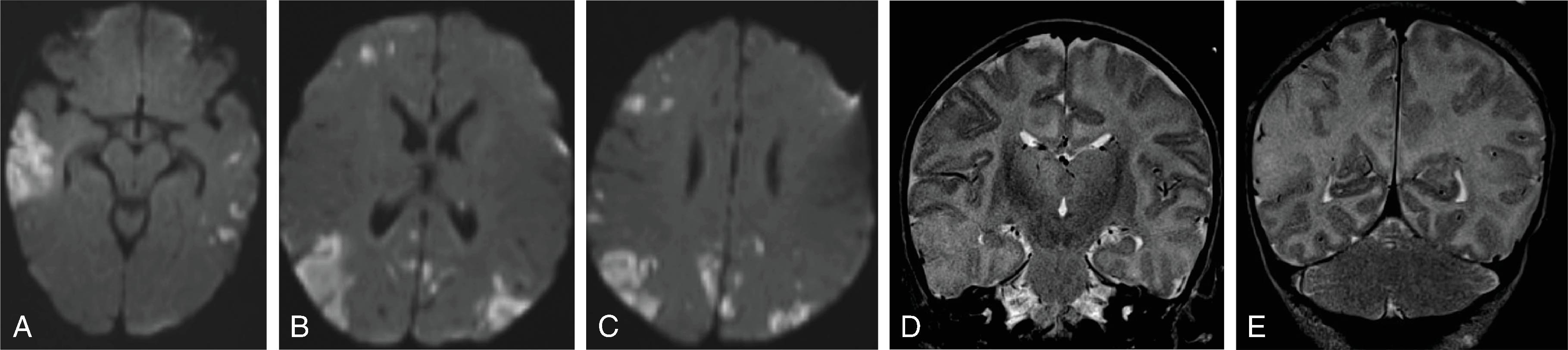
Ventricles: Ventriculomegaly, ventriculitis (rare), intraventricular septations, and hemorrhage
Parenchyma
Cortical malformations: Lissencephaly, polymicrogyria, schizencephaly
Early infections around 16 to 18 weeks of gestation result in microlissencephaly.
Infections around 18 to 24 weeks of gestation may cause polymicrogyria (most common).
Leukodystrophy : Periventricular T2W hyperintensity
Temporal polar cysts and germinolytic cysts
Calcifications (predominantly periventricular, may also be seen in central gray matter and elsewhere in white matter)
Parenchymal volume loss; porencephaly
Cerebellar dysplasia/hypoplasia
Hemorrhage
Differential Diagnosis (DDx): Other TORCH infections, and Aicardi syndrome
First discovered in 1947 in Zika Forest in Uganda
Single-strand RNA virus transmitted by female Aedes aegypti mosquito
Endemic in Asia, and Africa
Historical outbreaks have occurred; large outbreak in the Americas in 2014–2016
80% of infections are asymptomatic, 20% are symptomatic
Fever, headache, joint/muscle pain, rash, conjunctivitis, and Guillain-Barré (rare)
Maternal infection may cross the fetal placenta barrier and cause fetal neural infection; fetuses may be normal despite maternal infection
Maternal infection may occur via the mosquito transmission or by unprotected sex with an infected partner, even if partner is asymptomatic
Zika infection in the first trimester has a 1% to 13% risk of microcephaly
Confirmed diagnosis is made by positive detection of Zika virus in the infant serum, urine, or CSF within first 2 days after birth. A probable diagnosis is made in the setting of negative PCR with positive immunoglobulin M (IgM) antibodies. Diagnosis is excluded if both PCR and IgM are negative.
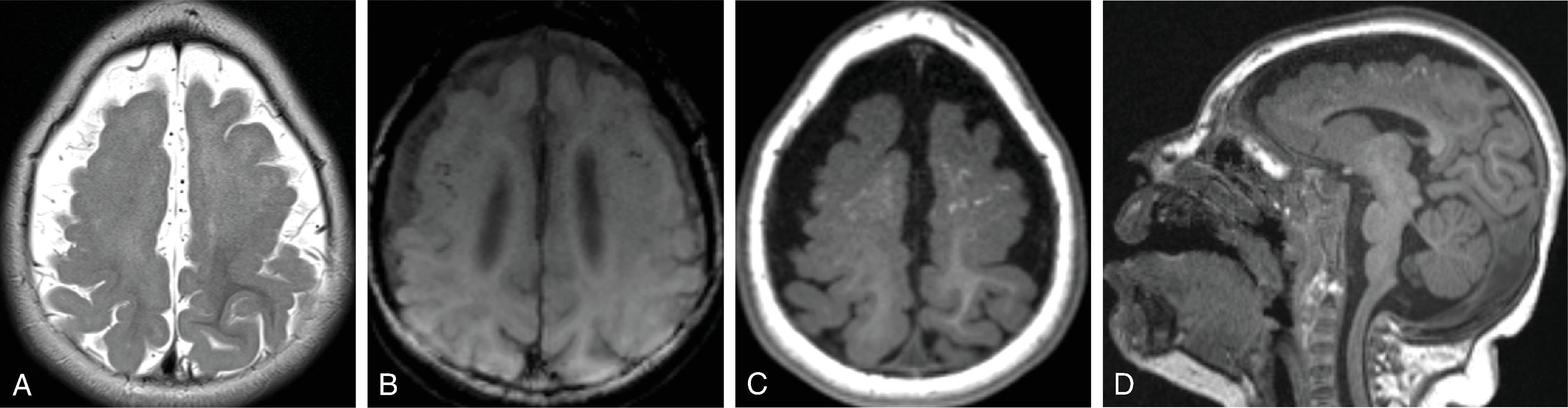
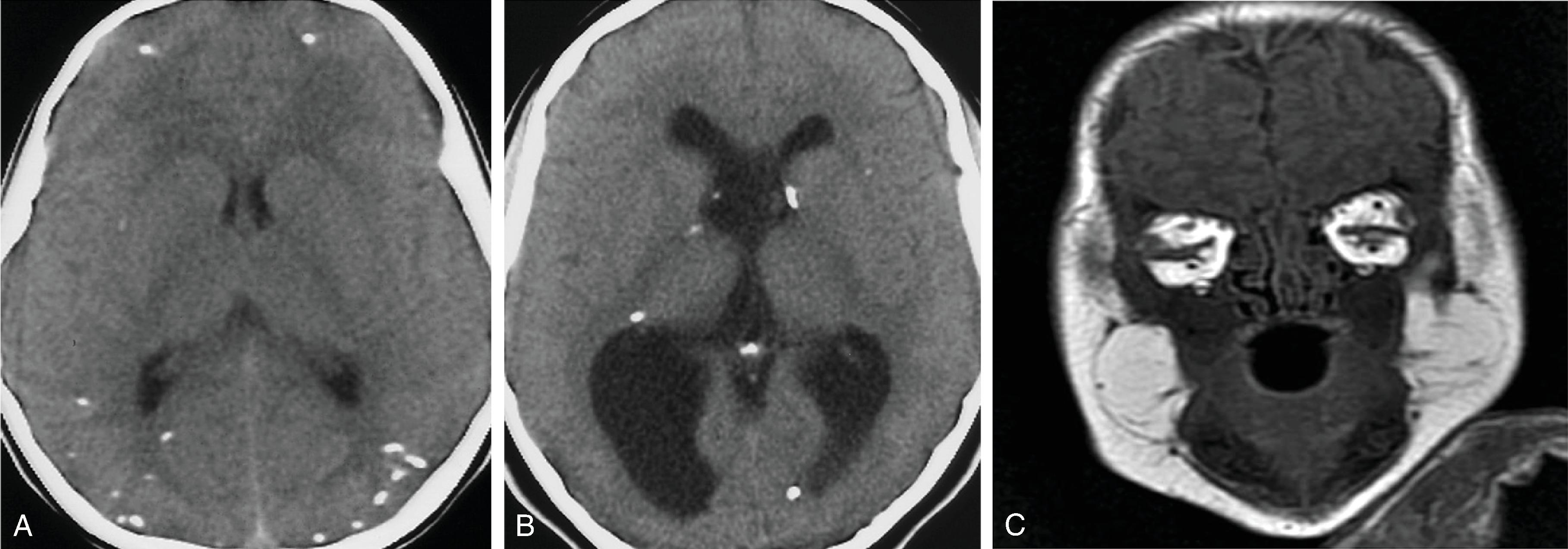
Brain
Microcephaly , overlapping sutures with secondary redundancy of scalp tissue
Ventricles: Ventriculomegaly, intraventricular septations especially in occipital horns, subependymal cysts
Parenchyma
Cortical malformation: Lissencephaly/microlissencephaly, pachygyria, polymicrogyria
Parenchymal volume loss
Calcifications predominantly and characteristically peripheral at gray-white junction, may also be seen in central gray matter and elsewhere in white matter (less common in posterior fossa)
Corpus callosum: Agenesis/dysgenesis/hypoplasia
Cerebellar dysplasia/hypoplasia
Brainstem hypoplasia/volume loss
Other
Arthrogryposis
Spine: Spinal cord volume loss, decreased number of ventral nerve roots
Orbits: Herniation of orbital fat into the cranial vault, intraocular calcifications, coloboma, cataracts, microphthalmia, and lens subluxation
Toxoplasma gondii is a protozoan parasite with infection occurring through infected domestic cats, ingestion of meats containing viable parasite, or contaminated water or soil.
Maternal infection may be asymptomatic; infection may cross the fetal placenta barrier and result in adverse neurologic and ophthalmologic sequelae.
In utero infection occurs in approximately 1/1000 to 1/10,000 births.
Transplacental infection rates increase during progressing pregnancy.
Infection later in pregnancy is more common but results in less severe disease.
If the fetus is infected before 20 weeks of gestation, findings may be severe, including the presence of microcephaly, hydrocephalus, tetraparesis, seizures, cognitive impairment, migrational disorders, microphthalmia, and blindness due to chorioretinitis.
Confirmed diagnosis is made with positive IgG with positive IgM and/or IgA, positive PCR, increasing IgG titers in the first year or relative to maternal IgG titer, or positive IgG beyond 12 months.
Classic triad:
Chorioretinitis, hydrocephalus, and intracranial calcification occur in a minority of patients; the majority of infected neonates have subclinical infection.
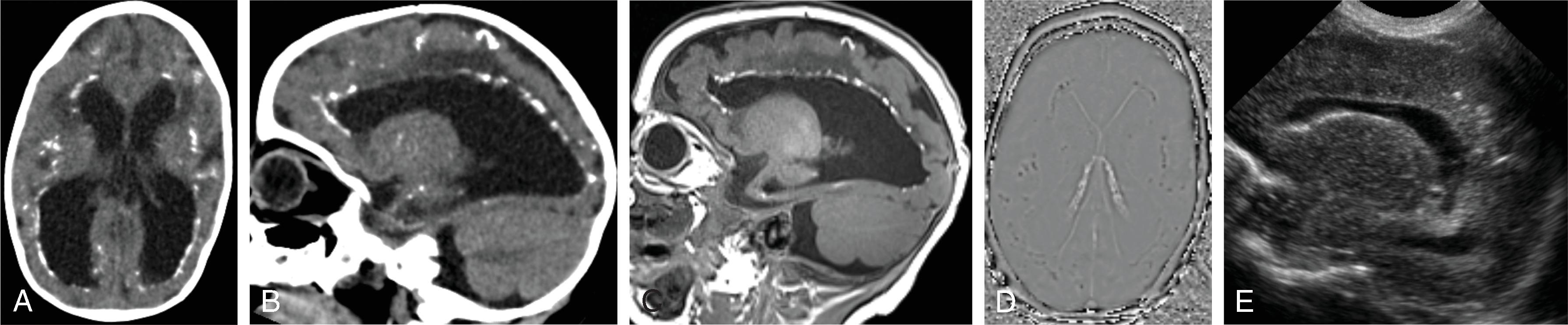
Ventricles
Ventriculomegaly , hydrocephalus (rare with infection after second trimester); ventriculitis that causes hydrocephalus. Predilection for dilatation of the atria of the ventricles
Parenchyma
Parenchymal volume loss, parenchymal injury/necrosis
Parenchymal injury may be severe and diffuse with early in utero infection
Volume loss may be mild, especially in late in utero infection
Calcifications are scattered throughout the basal ganglia, periventricular white matter, and cortical and subcortical parenchyma without site predilection
Larger calcification associated with earlier infection
Migrational anomalies are not present
Cysts
Orbits
Microphthalmia, chorionic calcifications, and lens deformity
Caused by a togavirus of the genus Rubivirus , which can infect and replicate within the placenta.
Congenital rubella is rare in countries with rubella immunization.
Maternal-fetal transmission occurs from maternal viremia and placental transmission and is spread through the fetal vasculature. The greatest risk of maternal-fetal transmission risk occurs during the first 10 weeks of gestation.
Clinical manifestations depend on timing of maternal infection. Maternal infection prior to 8 weeks typically results in cardiac and eye defects and hearing loss in maternal infections up to 18 weeks. Infections after 18 to 20 weeks are unlikely to cause defects.
Congenital rubella syndrome classically includes cataracts/glaucoma (25%), congenital heart disease (50% of patients; usually patent ductus arteriosus or peripheral pulmonary artery stenosis), and sensorineural hearing loss (66%) but can also include:
Brain injury, microcephaly
Neurocognitive, motor abnormality
Liver, spleen, lung, hormonal abnormalities
Low birth weight
Skin rash (blueberry muffin rash) due to extramedullary hematopoiesis
Diagnosis of congenital rubella syndrome made when one or more clinical signs or symptoms are present and laboratory evidence of congenital rubella infection through detection of rubella IgM antibodies, infant rubella IgG antibody that does not drop at an expected rate of twofold dilution per month, culture isolation of rubella virus, or PCR positive testing for rubella.
Ventricles: Ventriculomegaly, subependymal cysts
Parenchyma
Parenchymal volume loss, parenchymal injury/necrosis may be due to vasculitis
Parenchymal injury may be severe and diffuse with early in utero infection
Volume loss may be mild, especially in late in utero infection
White matter T2 signal abnormality from edema, gliosis, necrosis, myelination abnormalities
Calcifications in basal ganglia, periventricular white matter, cortex
Migrational anomalies are not a feature
Cysts
Orbits: Chorioretinitis
Bones: Radiolucent metaphyseal bands known as “celery stalk metaphysis”
Vertical transmission may occur at any time during gestation, during delivery (majority), and via breastfeeding.
Congenital HIV has remarkably decreased in the developed world due to screening, mitigation measures including antiretroviral, and avoiding breastfeeding but remains a significant public health issue elsewhere, especially sub-Saharan Africa.
Manifestations in neonates and children differ significantly from those encountered in the adult population.
Neonates are commonly asymptomatic.
Infants and children may go on to develop variety of symptoms, including systemic symptoms and neurologic symptoms in up to 50%, including such as encephalopathy, spasticity, motor weakness, seizures, and microcephaly.
Opportunistic infections are less common than in adult acquired HIV but CMV, progressive multifocal leukoencephalopathy (PML), varicella zoster virus (VZV), and fungal infection may occur.
CNS lymphoma occurs in a minority.
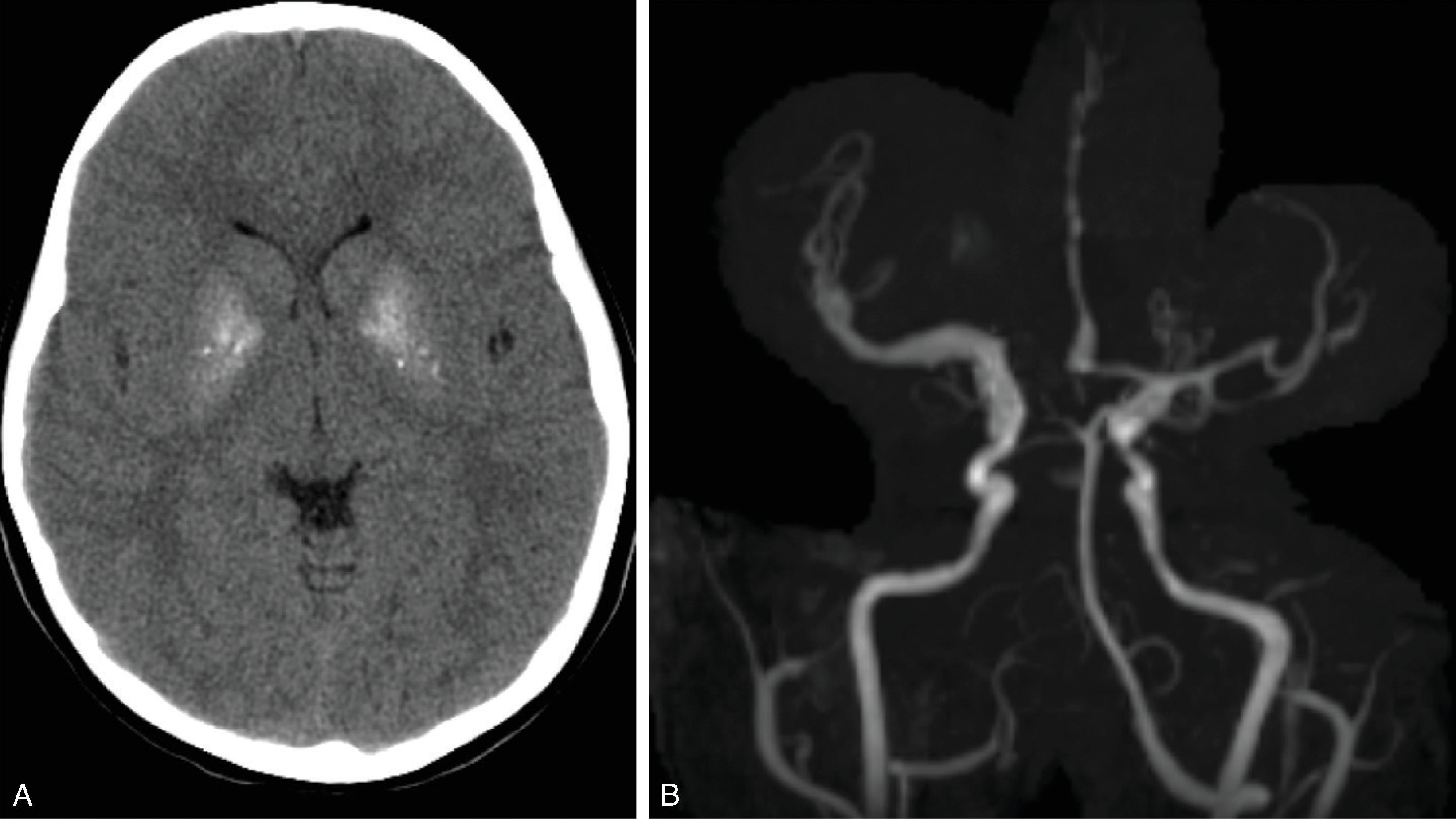
Ventricles: Ventriculomegaly
Parenchyma
Calcifications of the basal ganglia and subcortical white matter with congenital HIV; degree of calcification correlates with viral load
Volume loss (long term)
Vascular (long term)
Vasculopathy with alternating stenosis and ectasia/aneurysmal dilatation
May result in infarction, and/or hemorrhage
Other (long term): Lymphadenopathy, lymphoepithelial cysts
Differential Diagnosis of basal ganglia calcification: Aicardi-Goutieres, Cockayne syndrome, sequela of hypoxic ischemic injury, Down syndrome, hyper- or hypoparathyroidism, mitochondrial disorders, toxoplasmosis, and idiopathic

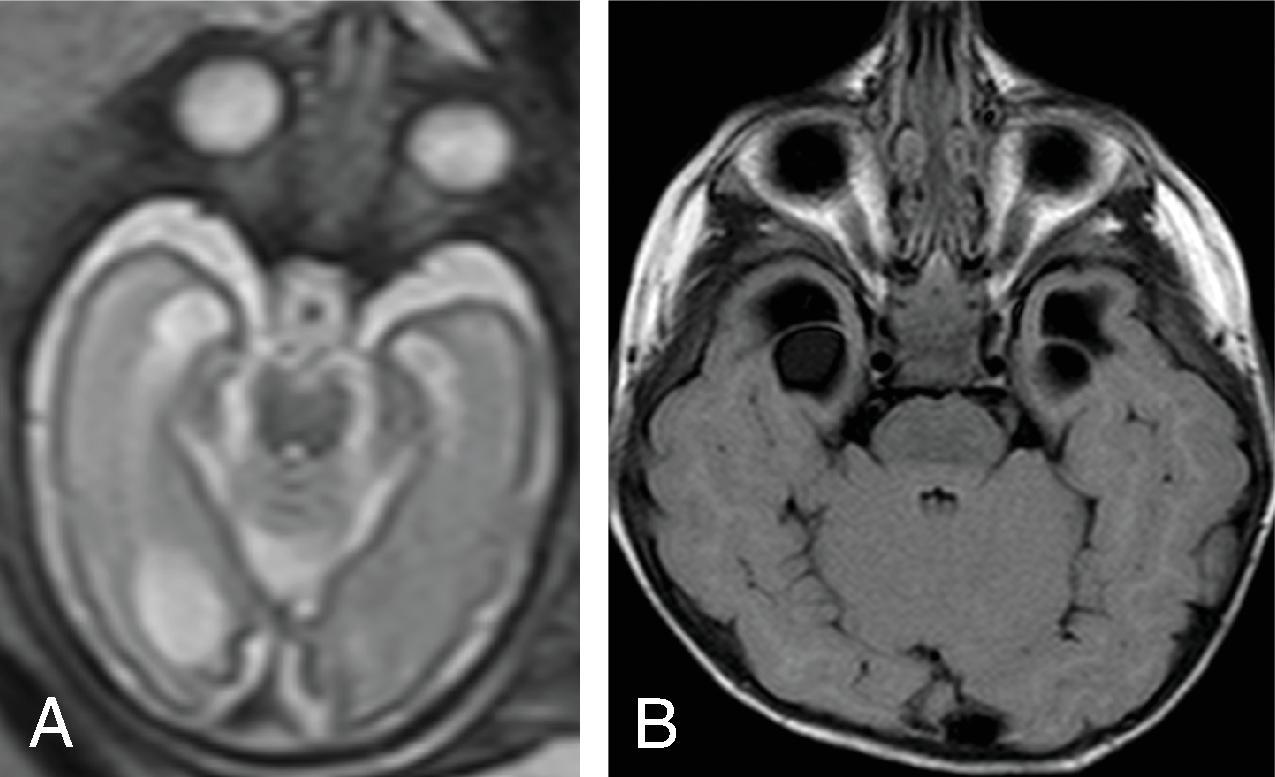
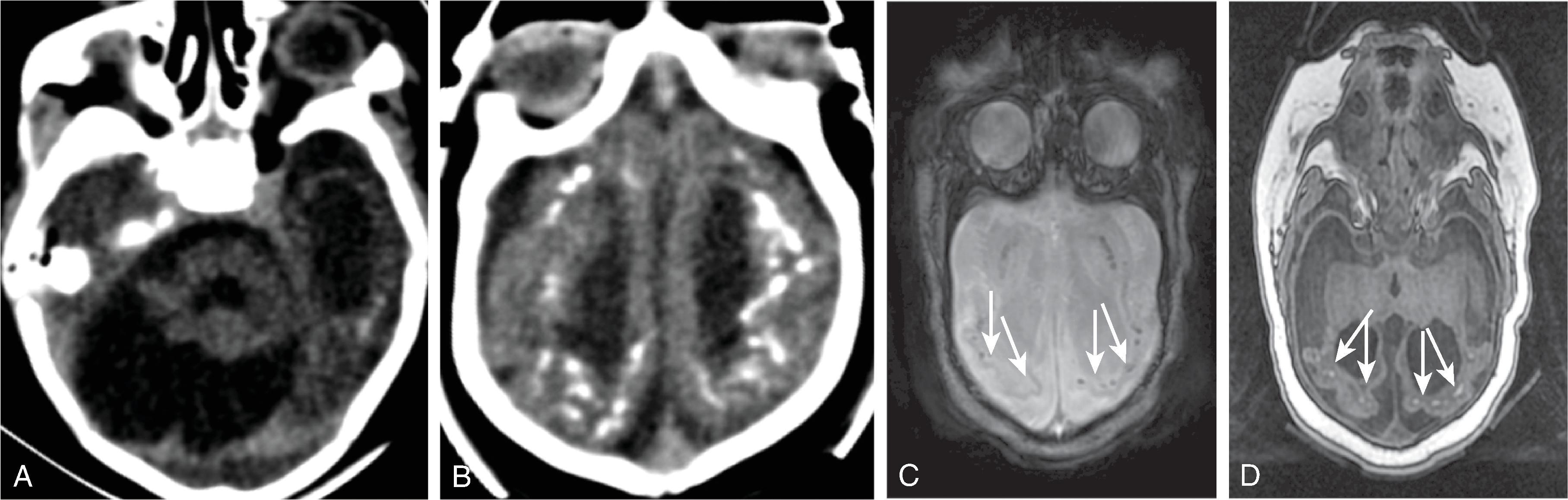
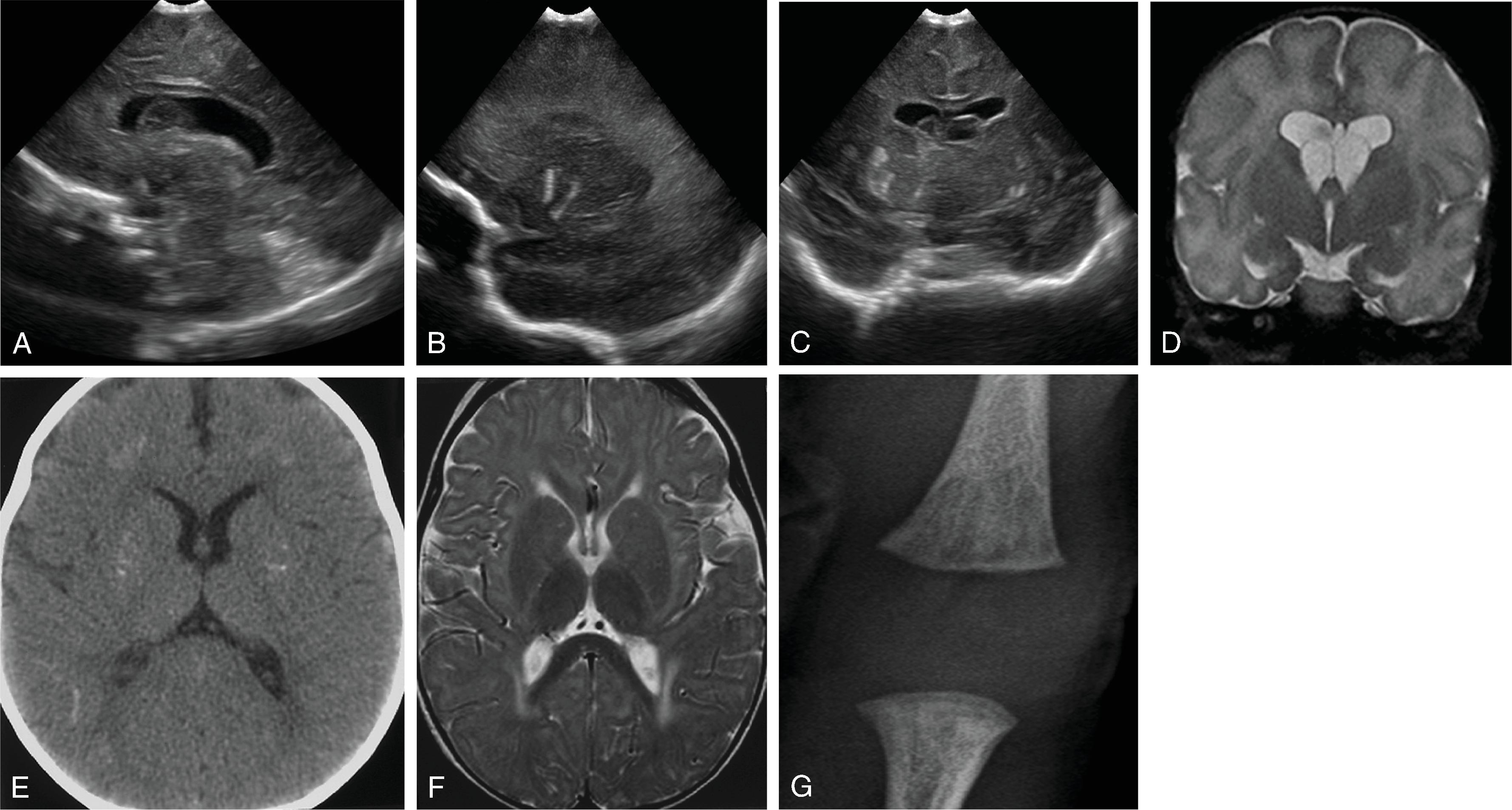
Single-strand RNA virus of the Picornaviridae family; HPeV-3 most commonly identified in CNS infections of young infants
Infection occurs via respiratory or gastrointestinal (fecal-oral) mechanisms with hematogenous spread to the CNS
Second most common cause of viral meningoencephalitis after enterovirus in infants younger than 2 months
Presentation
Gastroenteritis
Respiratory symptoms
Severe CNS infection: Fever, rash, irritability, seizures, sepsis-like features
Acute flaccid paralysis
Adverse neurodevelopmental outcome may occur
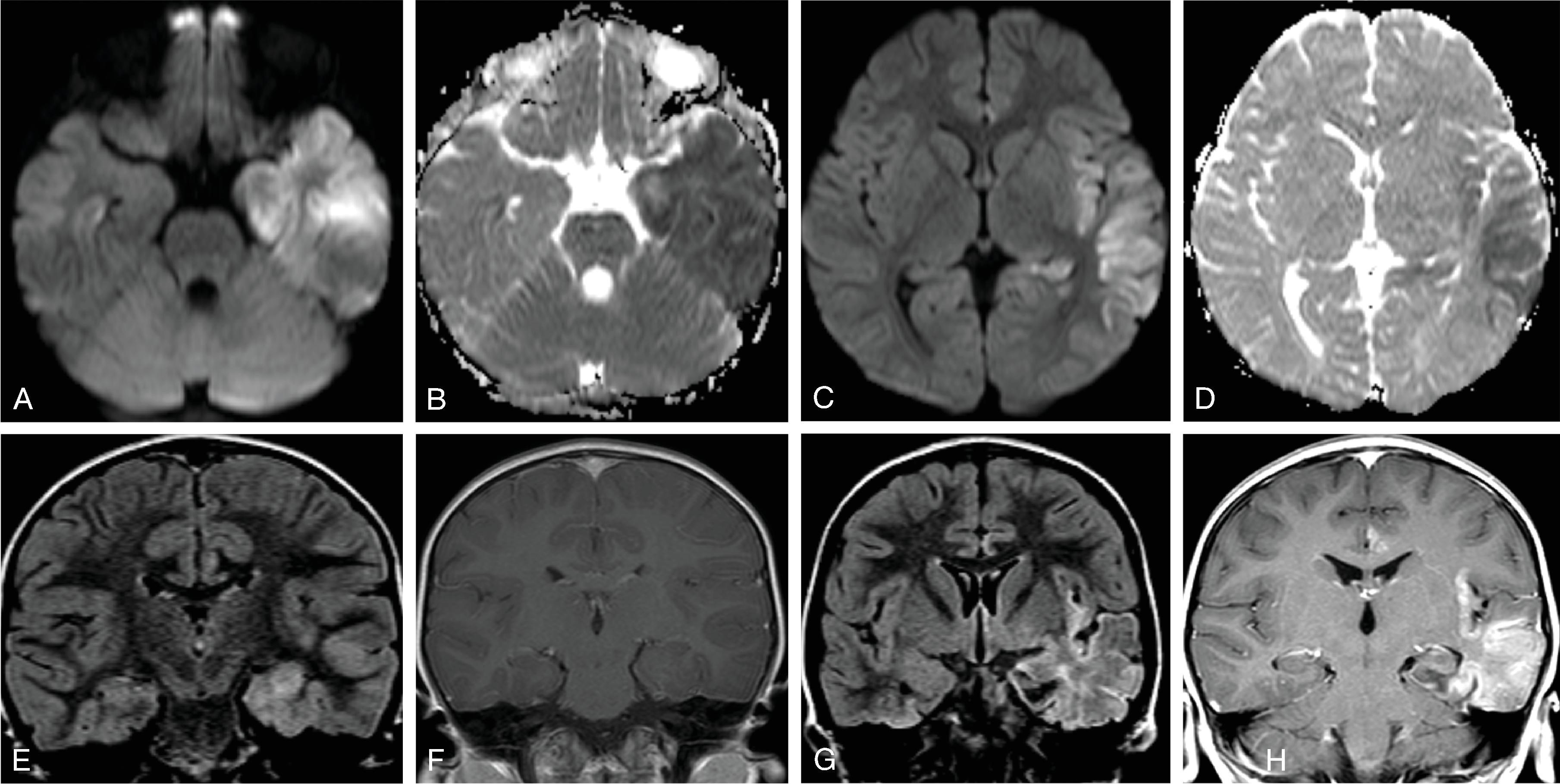
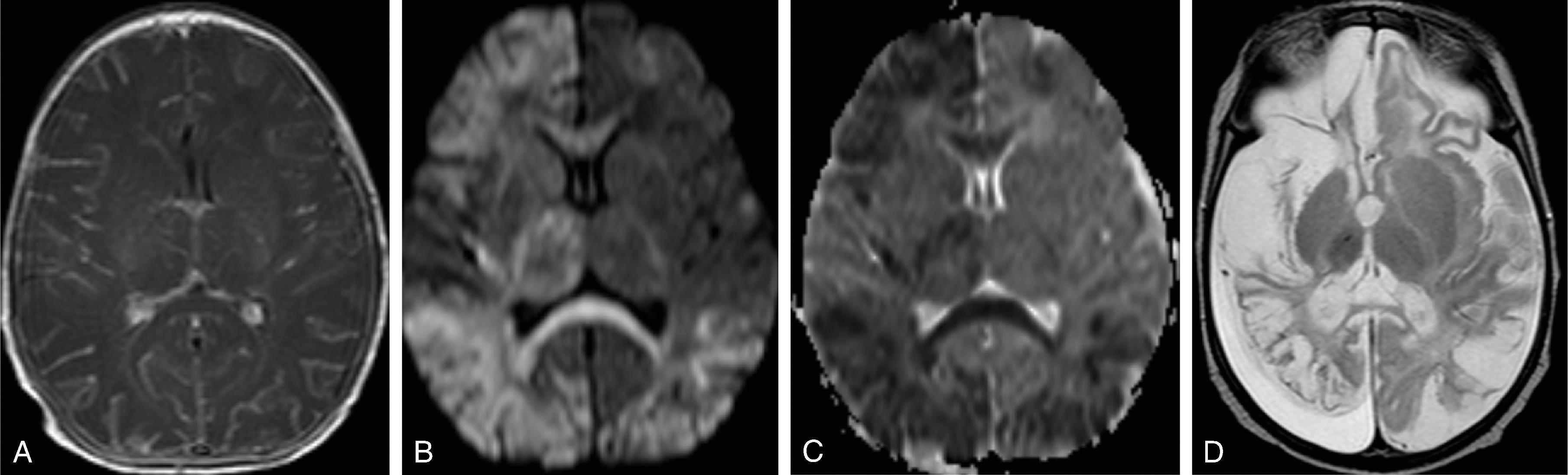
Mimics mild-moderate hypoxic ischemic encephalopathy (HIE): striated, nonenhancing T1W and T2W shortening in the periventricular white matter (frontal predominant) with intense restricted diffusion; corpus callosum is diffusely involved; variable involvement of the thalamus
May have foci of susceptibility within signal abnormality
Imaging is not pathognomonic; may be seen with other viruses such as rotavirus, and enterovirus. White matter injury from other causes such as congenital heart disease, prematurity may resemble this pattern
Permanent parenchymal injury may occur
Ubiquitous DNA virus belonging to Herpesviridae family with nearly 80% to 90% seroconversion in general population
Infection of mucosal surface or nonintact skin, usually orolabial route
Primary infection typically asymptomatic
Reactivation may be symptomatic or asymptomatic; cold sores most common but rarely may result in meningoencephalitis
Mechanism of meningoencephalitis
Reactivation at the level of the trigeminal ganglion with axonal spread to frontal and temporal lobes
Reactivation of latent virus within the brain parenchyma
Primary infection of the CNS
CNS entry may occur via olfactory or trigeminal nerves
Most common cause of sporadic fatal viral encephalitis
70% mortality in untreated patients
30% mortality in treated patients
High incidence of permanent neurologic deficits
Bimodal age distribution: Childhood and age >50 years with peak in late adulthood
Patients present with headache, fever, nausea, vomiting, seizures, encephalitis
Diagnosis made by CSF PCR; CSF is abnormal in more than 95% of patients and includes lymphocytic pleocytosis and increased protein
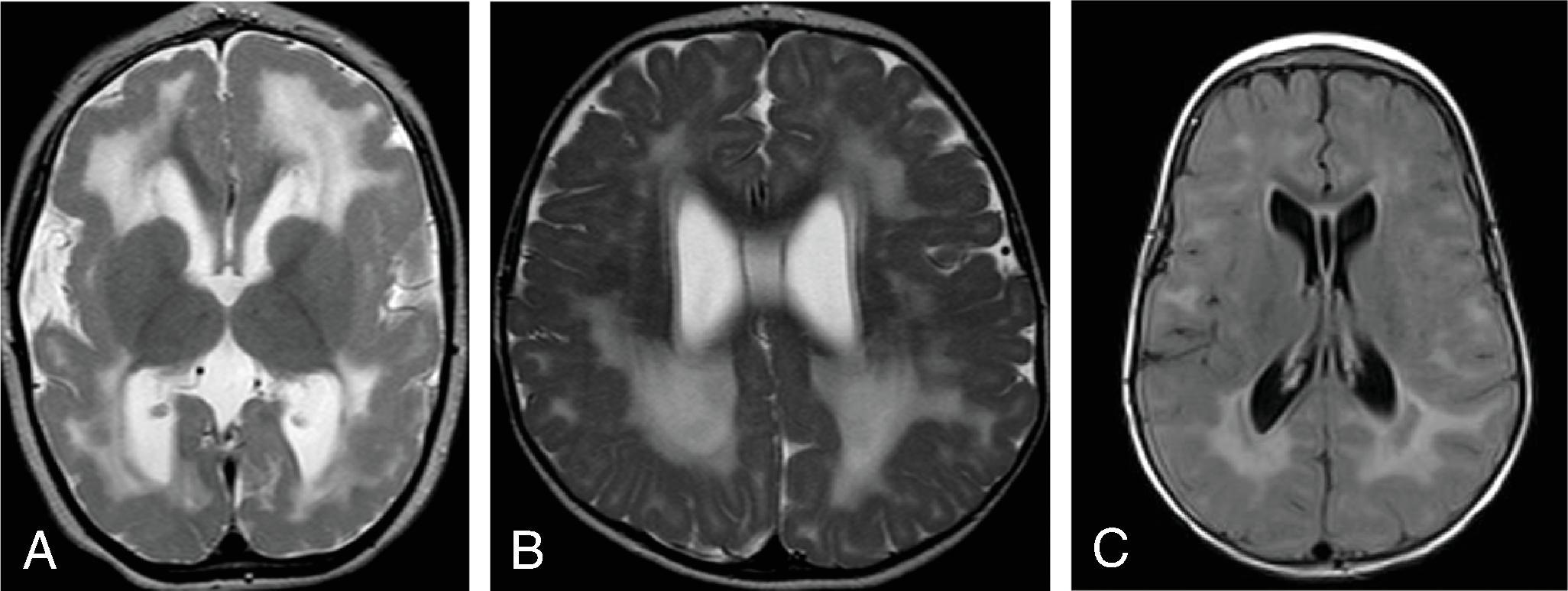
CT may be normal in the early phase of the disease.
MRI is the gold standard of imaging.
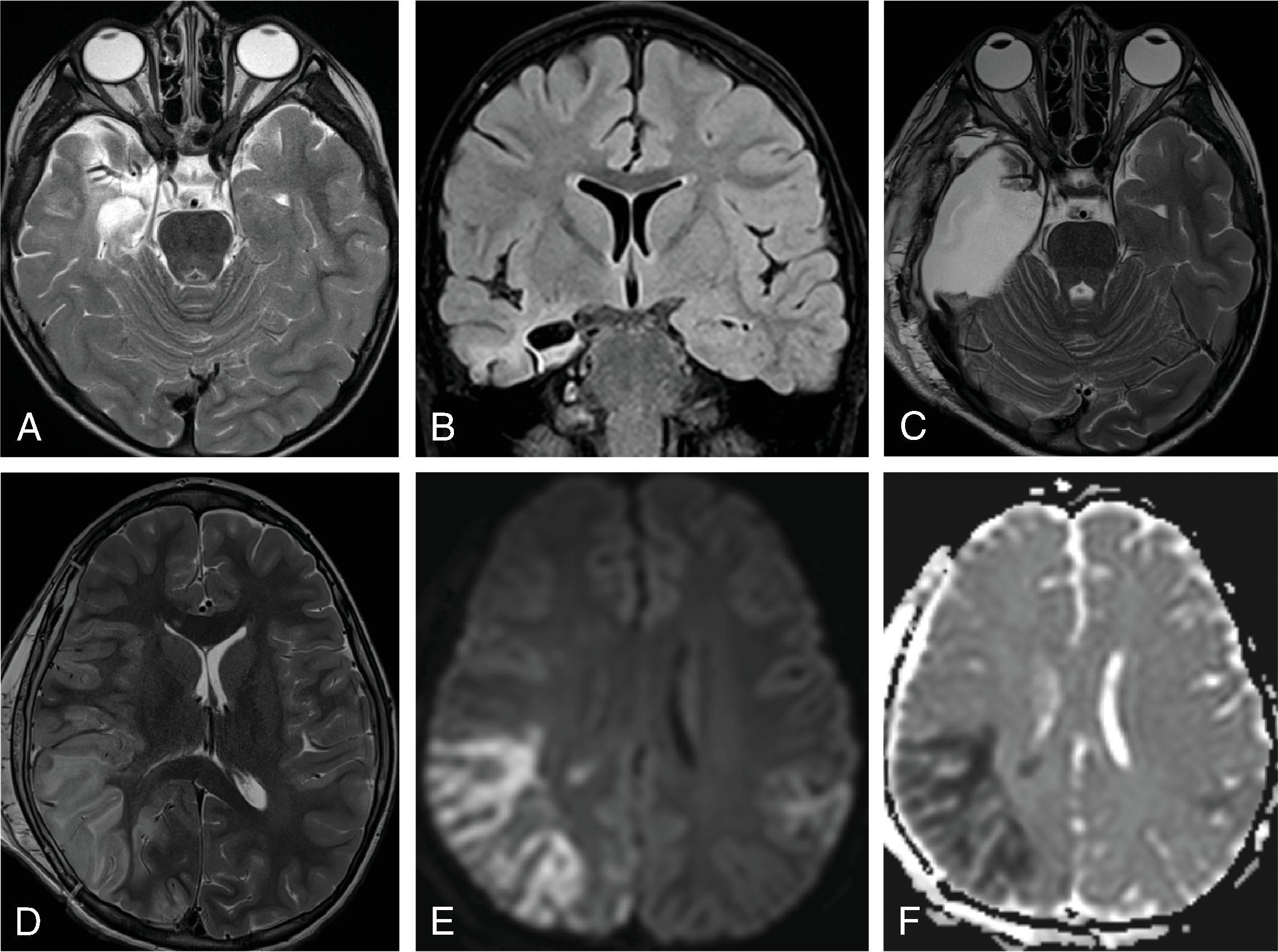
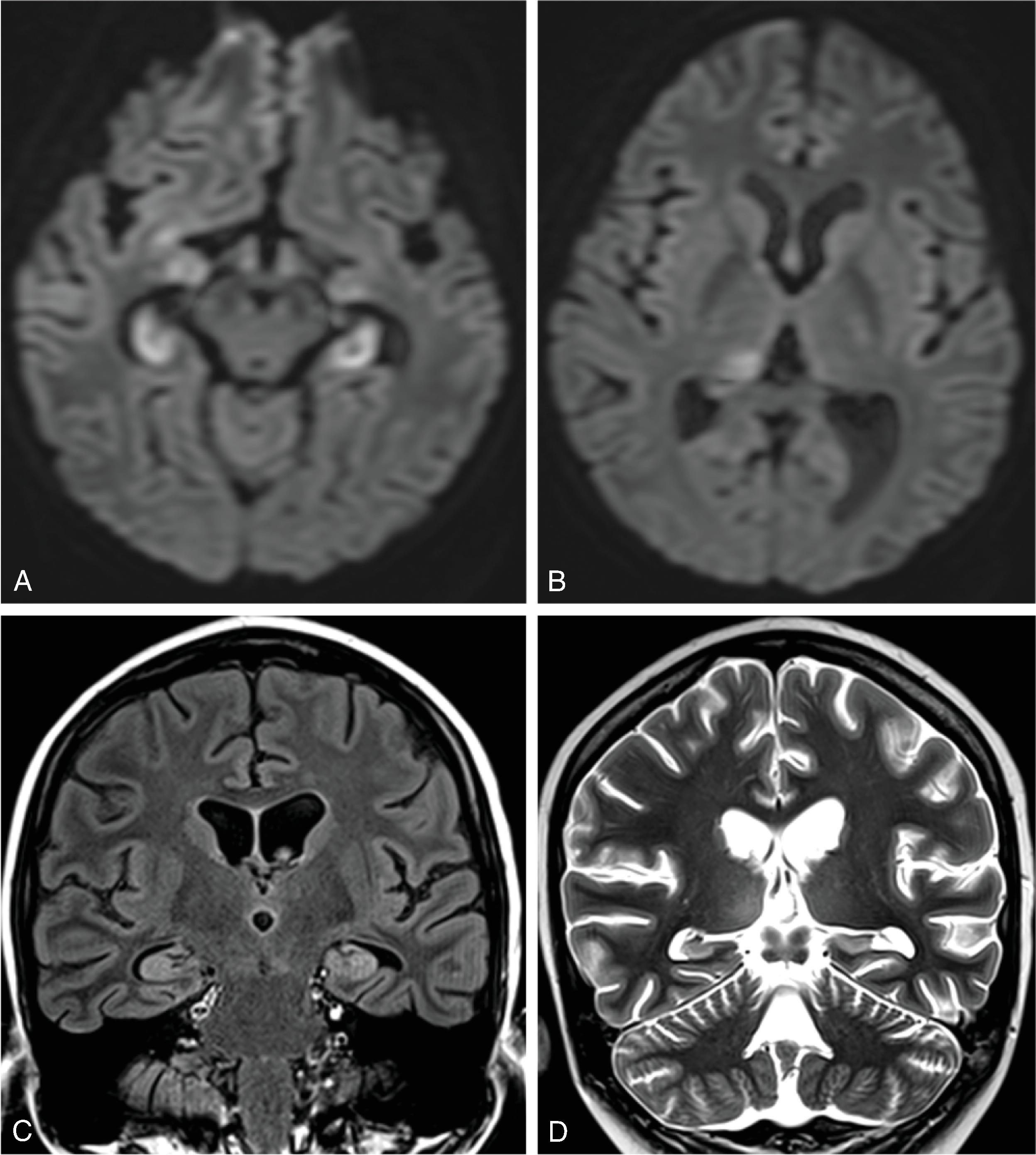
Bilateral asymmetric involvement of the cortical-subcortical inferior frontal lobes, temporal lobes (medial> lateral), insula, and cingulate gyri . Patchy bilateral hemispheric involvement may occur, mimicking thromboembolic infarct given the presence of restricted diffusion.
DWI imaging is very sensitive demonstrating restricted diffusion; may mimic multifocal thromboembolic infarcts.
T2W hyperintensity of involved parenchyma; multifocal susceptibility from hemorrhage.
Avid parenchymal and leptomeningeal enhancement well seen on T1W and T2W FLAIR postcontrast imaging.
Basal ganglia involvement is rare.
Encephalomalacia of affected areas is the end result.
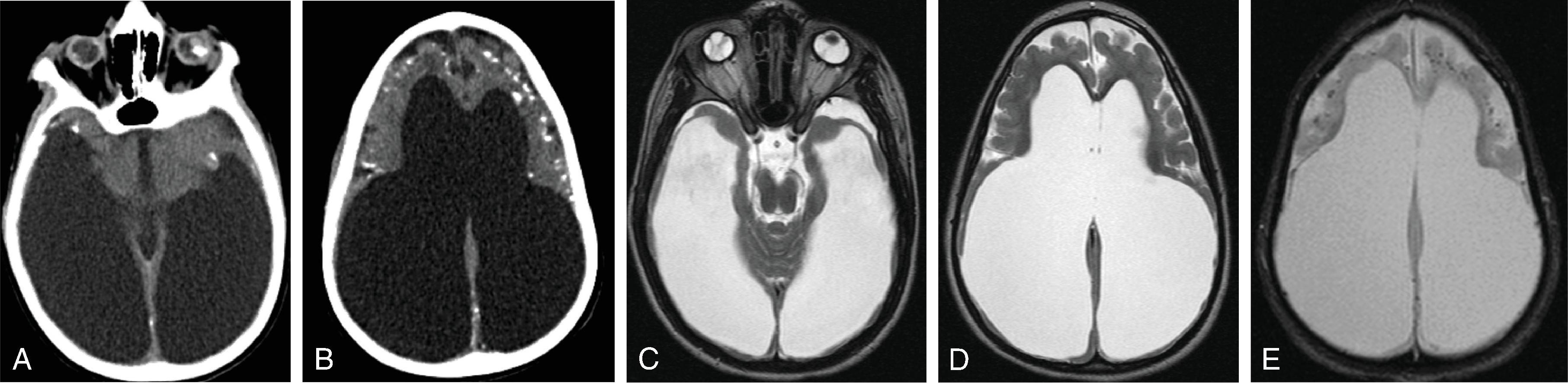
Accounts for 80% of encephalitis in infants.
HSV-2 infections in neonates occur in the perinatal/neonatal period and result from exposure to maternal HSV type 2 genital lesions at the time of vaginal birth.
Infants may present with systemic findings of seizure, lethargy, respiratory distress, vomiting, cyanosis, anorexia, and body temperature alteration.
CSF PCR gold standard. Up to 25% of neonatal HSV can have negative PCR in the early phase of infection requiring potential repeat CSF testing.
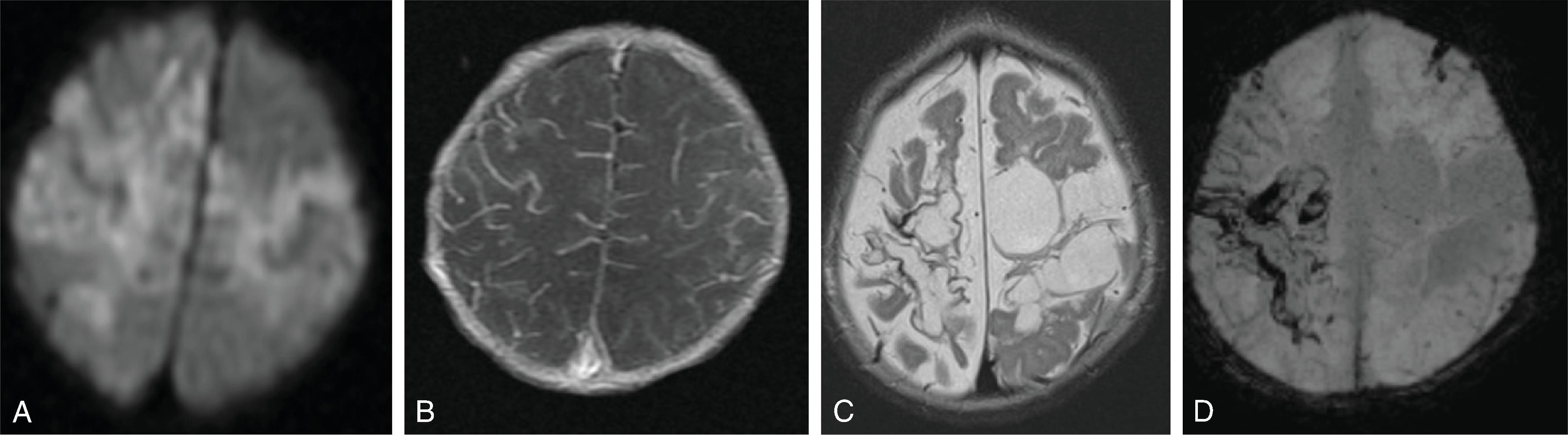
Variable, multifocal, watershed, or diffuse brain involvement without predilection for certain brain regions as seen in HSV-1
Cortex, white matter, central gray matter
Brainstem and cerebellum may be involved
Ultrasound and Computed Tomography
Nonspecific, includes the presence of both focal edema and diffuse edema
MRI
DWI imaging is very sensitive demonstrating restricted diffusion; may mimic multifocal thromboembolic infarcts or HIE
T2W hyperintensity of involved parenchyma; multifocal susceptibility may occur
Avid leptomeningeal enhancement well seen on T1W and T2 FLAIR postcontrast imaging
Encephalomalacia is present long term
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here