Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Endothelial keratoplasty (EK) is the procedure of choice for patients with endothelial dysfunction in both the adult and pediatric population.
EK allows for faster visual recovery and decreased intraoperative and postoperative risks compared to penetrating keratoplasty.
EK is not an appropriate keratoplasty option for patients with significant vision-limiting anterior corneal scarring.
There are several types of EK procedures: Descemet stripping (automated) endothelial keratoplasty (DSEK/DSAEK), ultra-thin DSAEK (UT-DSAEK), nanothin DSAEK (NT-DSAEK), and Descemet membrane (automated) endothelial keratoplasty (DMEK/DMAEK).
EK may be performed even in eyes with complex anterior segment and vitreous disease.
Since its introduction in the early 2000s, endothelial keratoplasty (EK) has quickly become the treatment of choice for patients with all types of corneal endothelial dysfunction. Using techniques that are readily adoptable by corneal surgeons, EK provides more rapid visual recovery with fewer intra- and postoperative complications than the alternative full-thickness penetrating keratoplasty (PK). The Eye Bank Association of America’s 2018 Statistical Report documents an exponential rise in the number of EK procedures performed within the United States over the past decade, from 1398 cases in 2005 up to 30,336 cases in 2018. Since 2012, the number of EK procedures performed in the United States has surpassed the number of PK procedures, with PK numbers on the decline. These trends reflect the many advantages of EK over PK.
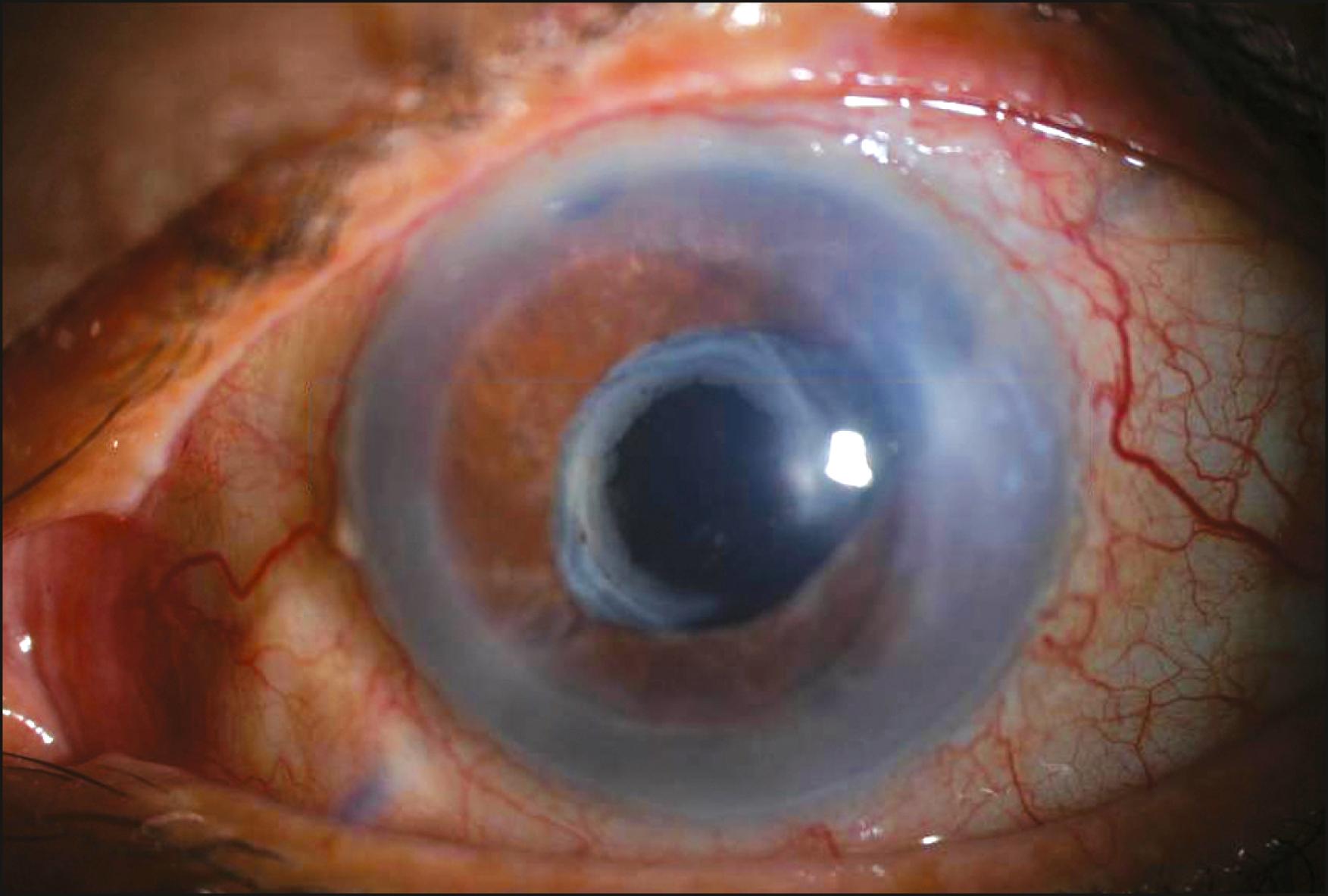
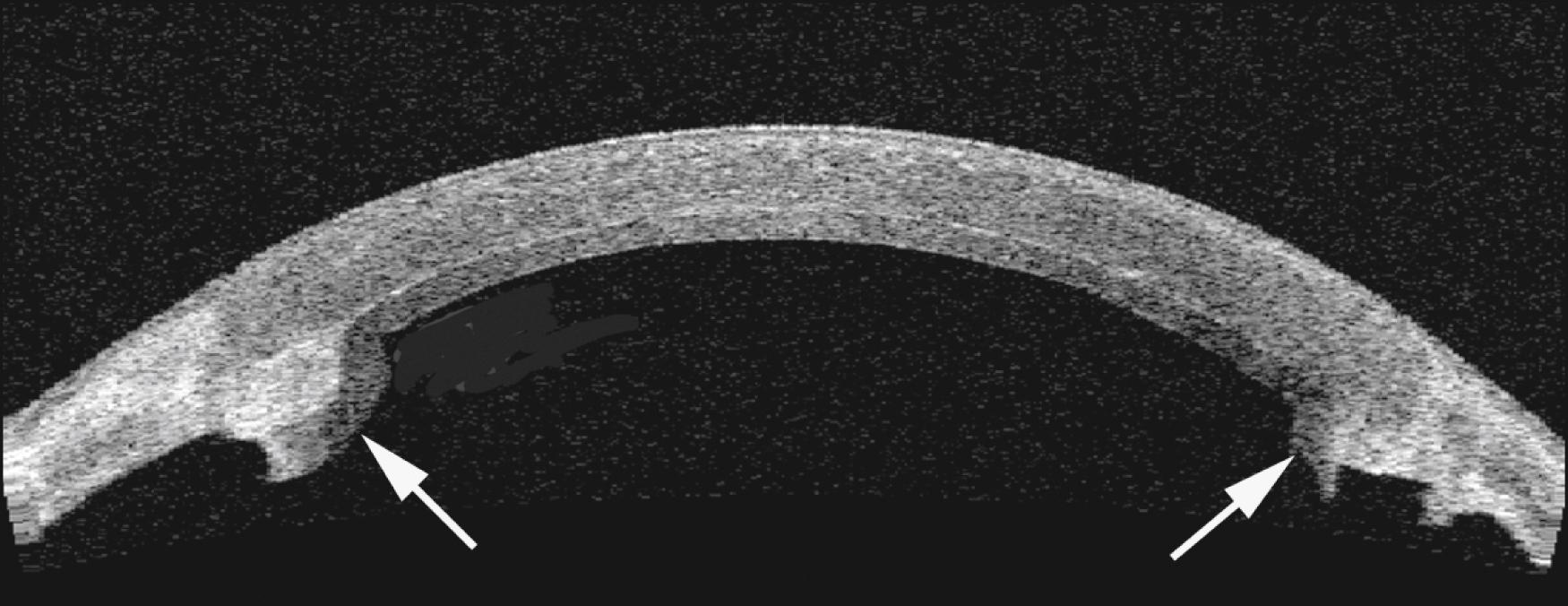
Candidates for EK procedures include patients with any type of endothelial dysfunction, including endothelial dystrophies such as Fuchs endothelial dystrophy, posterior polymorphous dystrophy (PPMD) or congenital hereditary endothelial dystrophy (CHED), pseudophakic or aphakic bullous keratopathy, iridocorneal endothelial (ICE) syndrome, endothelial decompensation from trauma or prior ocular surgery ( Fig. 128.1 ), or a late endothelial failure of a prior penetrating keratoplasty ( Fig. 128.2 and Table 128.1 ).
Indications
|
Contraindications
|
Assessment of anterior chamber space and specialized techniques advised in eyes with:
|
EK is not an appropriate option for patients with healthy endothelium, such as those with keratoconus or corneal ectasia (see Table 128.1 ). Similarly, EK may not be the optimal choice in patients with significant vision-limiting corneal subepithelial or stromal scarring. Depending on the patient’s visual needs and goals, a full-thickness penetrating keratoplasty or anterior lamellar keratoplasty may be a better choice in those cases.
The greatest advantage of EK procedures is the patients’ rapid visual recovery. , Vision after DSAEK typically stabilizes within the first 3 months of surgery, with minimal induced astigmatism from a small incision (approximately 3–5 mm in length) and a minimal shift in refractive error ranging from approximately 0.75 to 1.5 D of hyperopia. , Now with DMEK, vision recovery may occur even more rapidly, with average hyperopic shifts ranging between 0.03 and 0.5 D. This is in contrast to penetrating keratoplasty, where patients may developed significant regular and irregular astigmatism and there is a prolonged period between surgery and visual rehabilitation. Moreover, hard contact lenses or strong spectacle correction is required to achieve the best corrected visual acuity
Another advantage of the small incision in EK is that activity restrictions post-EK are fewer. Patients may frequently return back to regular activities within a few weeks after surgery. Patients can even engage in regular contact sports that carry some risk of minor trauma to the eye, such as basketball. This is a significant improvement over standard PK, after which minor trauma can readily rupture the transplant incision and cause loss of the eye.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here