Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The role of the immune system in controlling cancer was subject to debate for decades, reflecting the limited understanding of the immune system at the time and the complexity of tumor immunology. However, over time a wealth of evidence from murine and human studies has demonstrated that the immune system can control cancer. Numerous animal models have demonstrated the ability of T cells to reject tumors, revealed the importance of cytokines for antitumor immunity, and showed the susceptibility of immunodeficient mice to tumor formation. Compelling evidence of tumor immunosurveillance in humans is provided by reports of rare spontaneous tumor regressions in persons with melanoma and renal cell carcinoma, particularly after infection, paraneoplastic diseases (which are autoimmune neurologic manifestations of an antitumor response), and the higher incidence of melanoma in patients undergoing chronic pharmacologic immunosuppression after organ transplantation. Pediatric patients with immunodeficiencies are at risk for lymphoma, and posttransplant lymphoproliferative disease (PTLD) is a well-known entity in iatrogenically immunosuppressed patients. The immune system can prevent virus-induced malignancies, eliminate tumor cells via recognition of tumor antigens that distinguish them from “self,” and promptly terminate inflammation to avoid tumorigenesis. However, when the latter process is in disarray, such as in chronic inflammatory conditions and autoimmunity, the immune system is implicated in tumorigenesis. The control of tumor growth by the immune system also applies selection pressure, which may ultimately promote tumor progression. In this process, termed “cancer immunoediting,” cancer cells develop immune escape mechanisms and establish a tumor microenvironment that interferes with antigen presentation, T-cell activation, and differentiation, thereby leading to a gradual loss of control by T cells ( Fig. 47-1 ). An expanding body of preclinical and clinical experiences has established that the immune system can be manipulated in increasingly sophisticated ways to prevent, control, or aid in the control of established cancers. Careful selection of the appropriate target antigen(s) and consideration of preexisting immunologic memory are key features in the pursuit of successful immunotherapy. Antigens that are unique to the tumor and absent on healthy tissues often require priming of the immune system but possess the advantage that the induced antitumor response is unlikely to have autoimmune adverse effects. In the case of antigens that are present or overexpressed on tumor cells but are also detectable in some healthy tissues, depletion of T-cell clones with high avidity to the antigen may have polarized existing memory T cells toward tolerance. In this scenario, effective immunotherapy has to break tolerance and is more likely to induce undesired autoimmunity. The clinical use of immunotherapeutic modalities such as monoclonal antibodies (mABs), vaccines against oncogenic viruses, cytokines, and hematopoietic stem cell transplantation (HSCT) has been the standard of care in the prevention, treatment, and supportive care of cancer for many years. More recently, an exciting renaissance in cancer immunotherapy occurred as a result of the success of proof-of-concept clinical trials for a variety of novel immune-modulating strategies. As will be discussed further, these strategies include cellular therapies such as chimeric antigen receptor (CAR) T-cells (CARTs) and the first Food and Drug Administration (FDA)–approved cancer vaccine (sipuleucel-T); blockade of regulatory pathways with anti–cytotoxic T-lymphocyte antigen 4 (anti-CTLA-4) mABs; and antibody-targeted delivery of drugs via immunoconjugates such as brentuximab vedotin and trastuzumab emtansine. Many early-phase immunotherapy trials are being conducted for adult malignancies first and will be discussed when they are applicable. While promising results and toxicity data emerge from adult trials, the benefits of immunotherapy will also increasingly become available to pediatric patients with cancer.
The immune response can be divided into innate and adaptive immunity to differentiate between an early, generalized response against evolutionarily conserved molecular patterns and a highly specific response that forms fully as a result of exposure to specific antigens. One can also distinguishe a humoral from a cellular arm of the immune system. The humoral arm consists of soluble factors that are secreted by immune cells and includes antibodies and cytokines. The cellular arm encompasses antigen-presenting cells (APCs), phagocytes, lymphocytes, and innate immune cells.
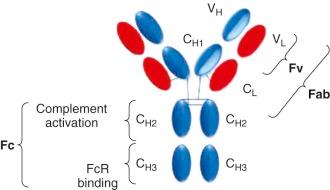
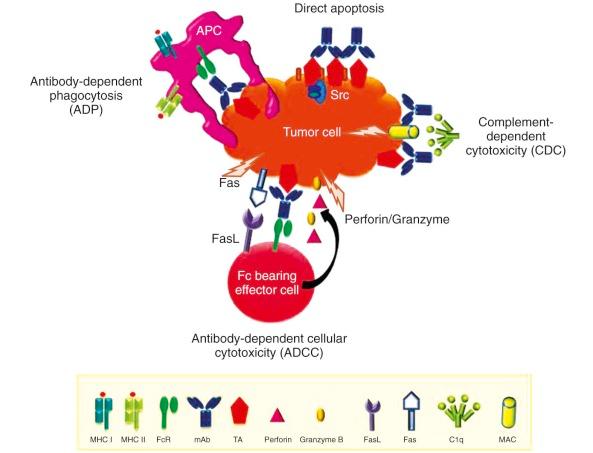
B cells have the ability to differentiate into plasma cells and secrete antibodies. B-cell receptors, which represent surface-expressed antibodies against a vast variety of potential antigens, are created by somatic V(D)J-recombination. Subsequent antigen exposure leads to clonal expansion of B cells with the cognate B-cell receptor and facilitates large-scale antibody production. Antibodies consist of two heavy chains (γ, δ, α, µ, or ε) and two light chains (λ or κ). The composition of the heavy chains determines the immunoglobulin (Ig) subclass, which can be IgM, IgG, IgA, IgE, or IgD. These immunoglobulin subclasses have different binding valencies and functions; for example, IgM is produced early in the immune response followed by a class switch to IgG, whereas IgA is predominantly involved in mucosal immunity. Antibodies function by binding to the antigen of their specificity via the antigen-binding fragment (Fab; consisting of one constant and one variable domain from each of the heavy and light chains), thereby marking their target for destruction in a process termed “opsonization.” Cellular destruction is mediated by the crystallizable fragment (Fc) component, which is composed of two heavy chains ( Fig. 47-2 ). Depending on the effector cell and type of Fc receptor (FcR), the immune response can be modulated in multiple ways. Activating FcRs contain a cytoplasmic immunoreceptor tyrosine activation motif, whereas inhibitory FcRs signal via an immunoreceptor tyrosine inhibition motif. FcR binding can lead to antibody-dependent phagocytosis (ADP) by macrophages or APCs or cell destruction by natural killer (NK) cells via antibody-dependent cellular cytotoxicity (ADCC). The Fc component can also fix complement, leading to complement-dependent cytotoxicity (CDC). Antibodies can further kill tumor cells by direct induction of apoptosis and blockade of growth factors or other stimulatory signals ( Fig. 47-3 ).
Cytokines are soluble proteins that are predominantly produced by leukocytes and carry out intercellular signaling function. Based on their varied functions, they can be classified into interleukins (ILs), interferons (IFNs), chemokines, and hematopoietic growth factors. Several cytokines have been used in cancer immunotherapy either as a single agent or to enhance the effect of other therapeutic agents. Growth factors such as granulocyte-colony stimulating factor (G-CSF) also play an important role in facilitating the neutrophil recovery necessary for compressed chemotherapy regimens, which have led to improved survival for children with multiple types of pediatric solid tumors. Lastly, analysis of the cytokine response triggered by immune therapies is informative in elucidating the mechanism of action and associated toxicities and can guide lifesaving therapeutic interventions, as demonstrated by the successful use of an IL-6 receptor (IL-6R) antagonist in the treatment of cytokine release syndrome associated with cluster of differentiation (CD)19-CAR therapy.
T cells are a major component of the adaptive immune system ( Fig. 47-4 ). They are derived from bone marrow, but in contrast to B cells, they travel to the thymus to undergo V(D)J-recombination of their T-cell receptors (TCRs), editing, and maturation. Somatic recombination of the α- and β-chains of the TCR results in the incredibly diverse T-cell repertoire from which clonal expansion can occur upon encounter of a specific antigen. To prevent autoimmunity, TCRs specific for “self” undergo negative selection in the thymus but also are subject to regulatory mechanisms in the periphery. Generation of an adaptive antitumor response begins with capture of tumor antigens by dendritic cells (DCs) in the peripheral tissues. DCs then travel to the draining lymph nodes, where they interact with T cells. Successful activation of a T-cell response (T-cell priming) requires presentation of the antigen on major histocompatibility complex class I (MHC-I) or class II (MHC-II) molecules for TCR-mediated recognition (signal 1), as well as a costimulatory signal (signal 2). Classically, the costimulatory signal is delivered to CD28 on T cells via the B7 family (CD80 and CD86) on APCs, but many other costimulatory molecules have been identified. The absence of costimulation leads to anergy. T cells may also receive inhibitory signals via CTLA-4, programmed death 1 (PD-1), and various other receptors, which play a physiologic role in terminating an immune response. The tumor microenvironment exploits some of these mechanisms to escape immune surveillance by MHC downregulation, as well as expression of inhibitory ligands such as PD-1 ligand (PD-L1). The discovery and characterization of other modulatory signaling pathways is ongoing and will continue to be a platform for therapeutic intervention.
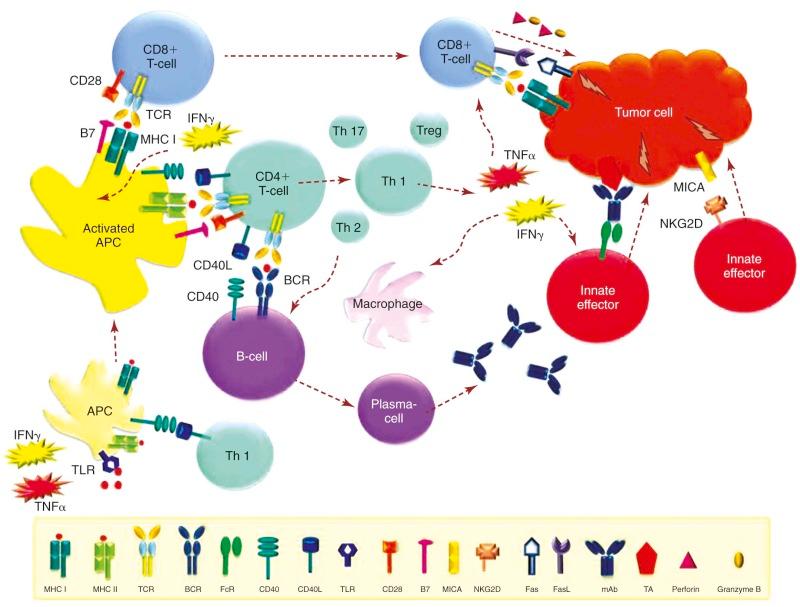
T cells express CD3 and are divided in CD8+ cytotoxic T lymphocytes (CTLs) and CD4+ helper T cells. DCs can process and present antigens via MHC-I and MHC-II pathways. CD8+ CTLs are generally activated via MHC-I. This pathway predominantly processes antigens derived from the cell itself (such as viral antigens), but it can also present antigens taken up by the cell through a mechanism referred to as cross-presentation. MHC-I is present on all nucleated cells, and upon recognition of the MHC-restricted cognate antigen on a tumor cell, primed CD8+ CTLs mediate tumor cell death by virtue of releasing perforin/granzyme B or by inducing apoptosis through interactions of death receptors such as Fas/Fas ligand. MHC-II expression is limited to APCs such as DCs, macrophages, and B cells, which process phagocytosed antigens and activate CD4+ T cells via the MHC-II pathway. CD4+ T cells do not generally directly mediate tumor cell lysis, but they critically support and influence the immune response by producing cytokines and providing “help” to CD8+ T cells and B cells via CD40 signaling. Depending on the polarization of their cytokine profile and function, CD4+ helper T cells are divided into Th1, Th2, Th17, and follicular helper T-cell subtypes and regulatory T cells (Tregs). Th1 responses are characterized by proinflammatory cytokines such as IFN-γ and tumor necrosis factor (TNF)-α, which enhance macrophage and CTL function and promote secretion of immunostimulatory cytokines, such as IL-12 by APCs. Th2 responses are essential for antibody production and class switching of B cells, are involved in allergic responses, and produce an array of cytokines such as IL-4, IL-9, IL-10, and IL-13 that contribute to eosinophil and mast cell activation. The Th17 subset was only described relatively recently. Although it is involved in the pathogenesis of autoimmune and inflammatory diseases, it may also play an important role in tumor immunity. Lastly, Tregs express CD25 and the forkhead box (FOX)P3 transcription factor in addition to CD4+. They serve to inhibit immune activation, induce self-tolerance under physiologic conditions, and notably expand in response to IL-2. Treg blockade or elimination is an important factor in facilitating an effective antitumor immune response, and therapeutic expansion of Tregs may play a role in controlling graft-versus-host disease (GVHD).
γδ T cells represent a small subgroup of circulating T cells that function at the interface of innate and adaptive immunity. Their TCR also undergoes somatic recombination and editing but consists of a γδ heterodimer. This subset may recognize specific antigenic determinants via the TCR or by a TCR independent pathway similar to that of NK cells.
Natural killer T cells (NKTs) are a unique subset of T cells with a highly restricted TCR repertoire, allowing recognition of certain glycolipid antigens, such as GD2, in conjunction with the nonclassical MHC-I molecule CD1d. They contribute to antitumor immunity as an early source of cytokine production, resulting in activation of other effector cells. Higher numbers of tumor-infiltrating NKTs have been associated with improved long-term disease-free survival (DFS) in children with stage IV neuroblastoma. NKTs are thought to inhibit tumor growth by targeting tumor-associated macrophages (TAMs) that have been shown to have clinical significance in neuroblastoma, Hodgkin lymphoma (HL), and other malignancies. NKTs are attracted by the chemokine (C-C motif) ligand 2 (CCL2). MYCN , the hallmark of aggressive neuroblastoma, mediates CCL2 repression and therefore reduces NKT infiltration. Via another escape mechanism, TAMs in the neuroblastoma microenvironment produce a different chemokine, CCL20, in response to hypoxia, thereby attracting NKTs into hypoxic traps. IL-15 was shown to protect NKTs from the inhibitory effects of hypoxia and enhances antimetastatic activity of NKTs.
NK cells play a key role in the innate immune response, in an early defense against infection or malignant transformation. NK cells can be phenotypically distinguished from other peripheral blood mononuclear cells because they are CD56+ and lack B-cell (CD19), T-cell (CD3), and monocytic (CD14) markers. Subsets of NK cells also express the FcRs CD16 and CD11b that mediate ADCC and participate in CDC. Contrary to T and B cells, NK-cell receptors do not undergo somatic recombination and do not require recognition of a cognate antigen to mediate cytotoxicity. Traditionally it has been thought that they do not develop immunologic memory, although this paradigm may be changing. Their function is tightly regulated by a complex system of activating and inhibitory receptors, which often recognize MHC-I or MHC-I–related molecules. These interactions provide the basis for the therapeutic exploitation of NK-cell alloreactivity. The key regulators of NK cells are activating and inhibitory killer cell immunoglobulin-like receptors (KIRs), which activate natural cytotoxicity receptors including NKp30, NKp46, and NKp44 and the activation receptor NKG2D. NK cells are capable of rapid killing via degranulation and release of toxic granules, primarily through a perforin and granzyme B–dependent pathway. They can also mediate apoptosis by utilizing Fas ligand or TNF-related apoptosis-inducing ligand (TRAIL) and execute ADCC via their FcRIII (CD16) receptor. NK cells further secrete chemokines such as CCL2 through CCL5, XCL1, and CXCL8. Their clinical significance in pediatrics is underscored by the susceptibility of infants born with NK-cell deficiencies to fulminant viral infections and the NK-cell defects underlying primary hemophagocytic lymphohistiocytosis. NK cells facilitate stem cell engraftment, fight infection, and control cancer, yet they do not cause GVHD. These characteristics make them attractive therapeutic candidates for adoptive NK-cell therapies.
Dendritic cells (DCs) represent a small subset of peripheral blood mononuclear cells (1% to 2%). They are mobile sentinels that collect antigen from peripheral tissues and carry it to the secondary lymphoid organs to activate T cells. DCs are termed “professional APCs” based on their ability to process and present antigenic peptides on MHC-I or MHC-II molecules. In steady state, they reside in the periphery in an immature state and play an important role in maintaining tolerance by taking up self-antigens. Successful T-cell activation requires DC activation. Upon activation, DCs upregulate MHC molecules, costimulatory molecules (which provide the second signal for T-cell activation), and chemokine receptors (which enhance homing to lymphoid organs) and secrete inflammatory cytokines such as IL-12. DC activation can occur in response to a variety of signals, such as the receipt of exogenous and endogenous danger signals via Toll-like receptors (TLRs), which recognize evolutionarily conserved molecular patterns from products of damaged or dying cells and from pathogens. DCs are also matured by proinflammatory cytokines secreted by other cells (e.g., innate effectors) or by CD40 ligation. In addition, DCs are important in launching humoral immunity, partly because of their capacity to directly activate B cells.
Myeloid DCs and plasmacytoid DCs are the two main subsets among various other DCs. They express high levels of human leukocyte antigen (HLA)-DR (MHC-II), but they differ in their expression of CD11c (myeloid DCs), CD123 (plasmacytoid DCs), and TLRs, among other markers. DCs are critical regulators of adaptive T- and B-cell responses and are central to the development of successful tumor vaccines. Because of their low abundance in the peripheral blood, sufficient numbers of DCs can be generated in vitro either by expansion of isolated DCs or by generation from monocytes using cytokine cocktails. DCs further play a role in the pathogenesis of GVHD and are required for full graft-versus-leukemia (GVL) effects, and thus their therapeutic manipulation is of relevance in HSCT.
Neutrophils are crucial to the rapid destruction of pathogens, particularly bacterial, fungal, and certain parasitic organisms, as evidenced by the high risk of sepsis during periods of neutropenia in the oncology population. However, neutrophils also contribute to antitumor activities of the immune system. Through their FcRs, they can be involved in ADCC-mediated tumor destruction. In addition, neutrophil activation at sites of the tumor via administration of cytokines such as GM-CSF can play a role in tumor cell degradation and enhance antigen presentation.
Monocytes are myeloid-derived phagocytic cells that differentiate into resident macrophages upon recruitment into tissues. Macrophages are able to ingest apoptotic cells and opsonized cells via their FcRs. Aside from their role in clearing cellular debris, they are able to present antigenic peptides of the digested cells in an immunogenic way. Activated macrophages prominently secrete cytokines such as IL-12, which may be critical in activating local immune responses by NK cells and T cells. Macrophages were originally classified into M1 (proinflammatory) and M2 (antiinflammatory) macrophages according to their polarization status. Although this classification remains conceptually helpful, it is now clear that tissue macrophages display a high degree of functional and phenotypic plasticity in response to changing microenvironmental stimuli and that M1 and M2 polarization represent extremes of a continuum of activation states. Increasing evidence indicates that TAMs are implicated in protumor effects and can play a role in tumor initiation, progression, and distant metastasis. Limited evidence suggests that myeloid-derived suppressor cells develop from a common myeloid progenitor without a monocytic intermediate and have predefined immunosuppressive properties, whereas monocytes lack suppressive activity in steady state and acquire this function in response to certain stimuli. In persons with cancer, the majority of studies support an association between high TAM density and poor clinical outcome, as has been demonstrated in several malignancies, including neuroblastoma. However, TAM function in tumor immunity appears to be dynamic and heterogeneous depending on the tumor type, tumor progression, location within the tumor, and perhaps most importantly, polarization of the TAM. In this regard, increased density of M2-like TAMs is a marker of poor prognosis, whereas the presence of M1-like subsets is advantageous. Based on these findings, subpopulations of TAMs are now being explored as new therapeutic targets.
Tumor antigens (TAs) are molecules that enable the recognition of tumors by components of the immune system. A wide array of target antigens have been identified and may be classified into various subgroups according to their origins. Tumor-specific antigens are epitopes that are found exclusively on malignant cells. This group includes proteins arising from mutated oncogenes, clonally rearranged immunoglobulin genes, and oncoviral gene products. Tumor-associated antigens are expressed on some healthy and malignant tissues alike. Tumor-associated antigens may arise from overexpressed normal proteins, oncofetal proteins, lineage-restricted markers, histocompatibility molecules, and proteins that are normally expressed in immune-privileged sites.
A number of malignancies are associated with specific genetic mutations or translocations, resulting in the synthesis of novel proteins that are foreign to the host's immune system, thereby offering the potential of immune recognition while sparing healthy tissues. Commonly they are drivers of or contribute to tumorigenesis, as is the case for oncogenes or mutated tumor suppressor genes, but they may also arise from mutations not directly involved in the neoplastic process. A variety of malignancies express gene products derived from mutated tumor suppressor genes, such as p53 or ras . Examples of antigens derived from mutated oncogenes include the EWS-FLI fusion protein resulting from the t(11 : 22) translocation characteristic of Ewing sarcoma and the p210 and p190 products of the bcr/abl translocation in chronic myelogenous leukemia (CML) and Philadelphia chromosome–positive acute lymphoblastic leukemia (ALL), respectively.
Viral infections play a causal role in several malignancies and give rise to immunogenic viral proteins that can be recognized and eliminated by the immune system. This process is underscored by the fact that immunosuppressed persons, particularly those with impairment of T-cell immunity, have a higher propensity to develop Epstein-Barr virus (EBV)–associated lymphomas and human papillomavirus (HPV)–associated skin and cervical cancers. Examples of oncoviral proteins are the expression of the EBV antigens EBNA-1, EBNA-3, LMP-1, and LMP-2 in PTLD and some lymphomas and the papillomavirus E6 and E7 proteins in cervical carcinomas.
Surface immunoglobulin is a marker of B-cell maturity and is present in mature B-cell non-Hodgkin lymphomas (NHLs) and multiple myeloma. Because surface immunoglobulin expression results from separate somatic recombination events in each B cell, all malignant cells in a monoclonal B-cell malignancy express the clonally unique immunoglobulin variable region, or idiotype. Immunoglobulins are proteins and can therefore be immunogenic and lead to the development of idiotype vaccines. Another approach to targeting this group of TAs includes the generation of anti-idiotype mABs in mice, which in turn are immunogenic and amplify the immune response upon administration to the patient as a type of vaccine.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here