Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The authors thank Dr. Hulya Sahin Ozkan for her contributions in the preparation of this chapter.
In the ensuing chapter, the cellular lineage markers and the application of immunohistochemistry (IHC) in the diagnosis and management of specific tumor types are reviewed.
We feel obliged to provide a cautionary statement. It is our strong bias that IHC is an extremely powerful tool, but only if it is used cautiously and in combination with morphology. It is our opinion (and experience) that there is not a magic IHC marker that makes the diagnosis by itself. There are always exceptions, and unfortunately, these exceptions tend to merge when IHC is needed the most. This should not come as a surprise though. After all, basic morphology and IHC are two different facets of the same phenotypic process in pathologic conditions. Where one is “unusual” or outside of the general realm, the other tends to be so as well. ,
The pancreas is one of the most versatile organs in the types of neoplasia it generates. This is partly because it is almost unique in harboring two functionally entirely distinct components, exocrine and neuroendocrine, in an otherwise intimate mixture, and tumors arising from these two components have vastly different pathologic and biological characteristics. Therefore, pancreatic neoplasms are classified based on their cellular lineage—that is, the component of the organ they recapitulate: acinar, ductal, neuroendocrine, or others; however, cross differentiation also does occur. For example, acinar cell carcinomas often contain numerous neuroendocrine cells or a separate neuroendocrine component. Additionally, the pancreas is one of a few organs, along with liver and kidney, that has an organ-specific “blastic” tumor of its own, pancreatoblastoma, which is characterized by differentiation along all components of this organ. Thus, IHC plays a crucial role in delineating the differentiation of neoplasms that arise in this organ and is an invaluable adjunct in the often-challenging differential diagnosis. It has been an important tool in unraveling the mechanisms of tumorigenesis as well.
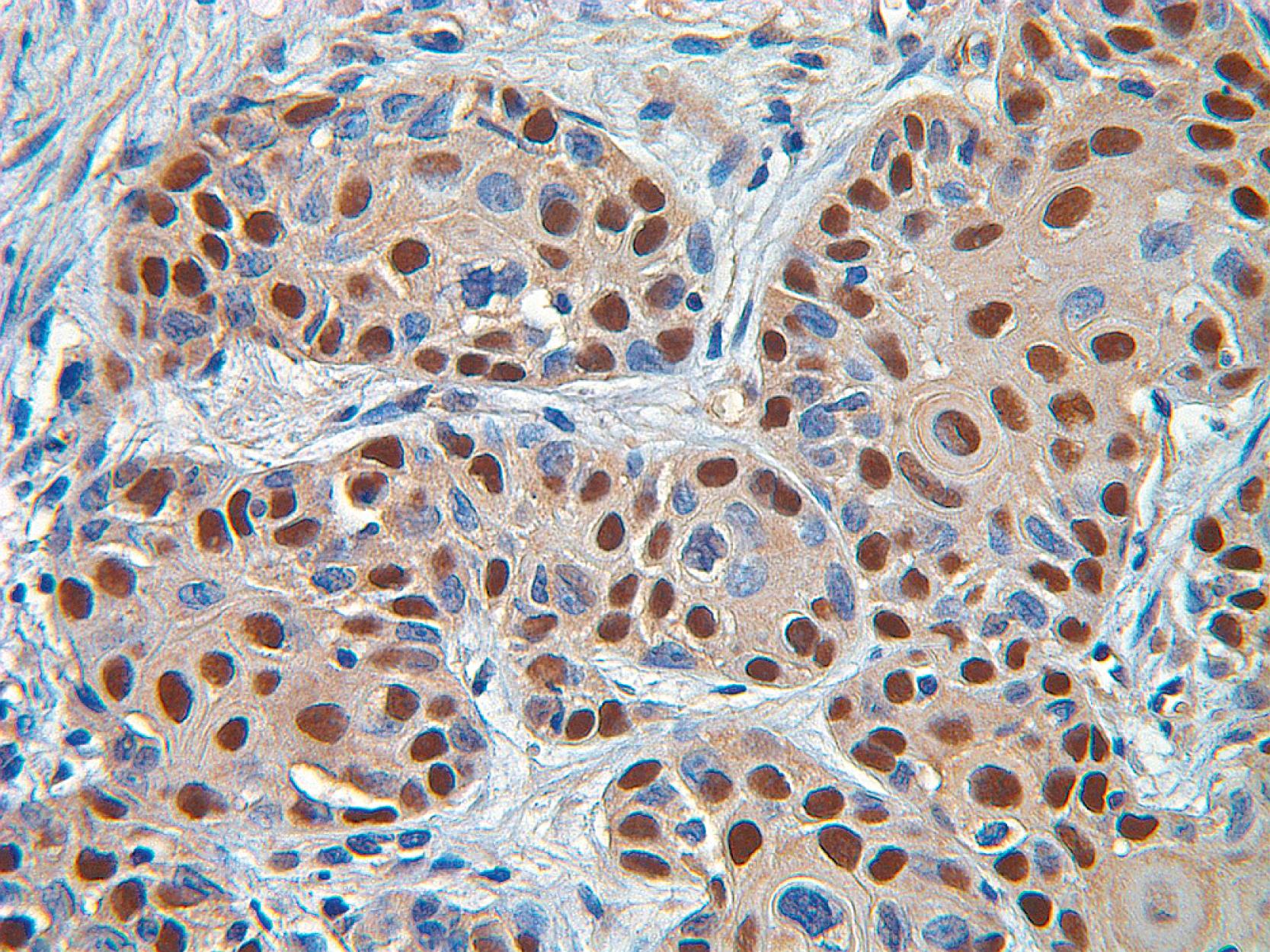
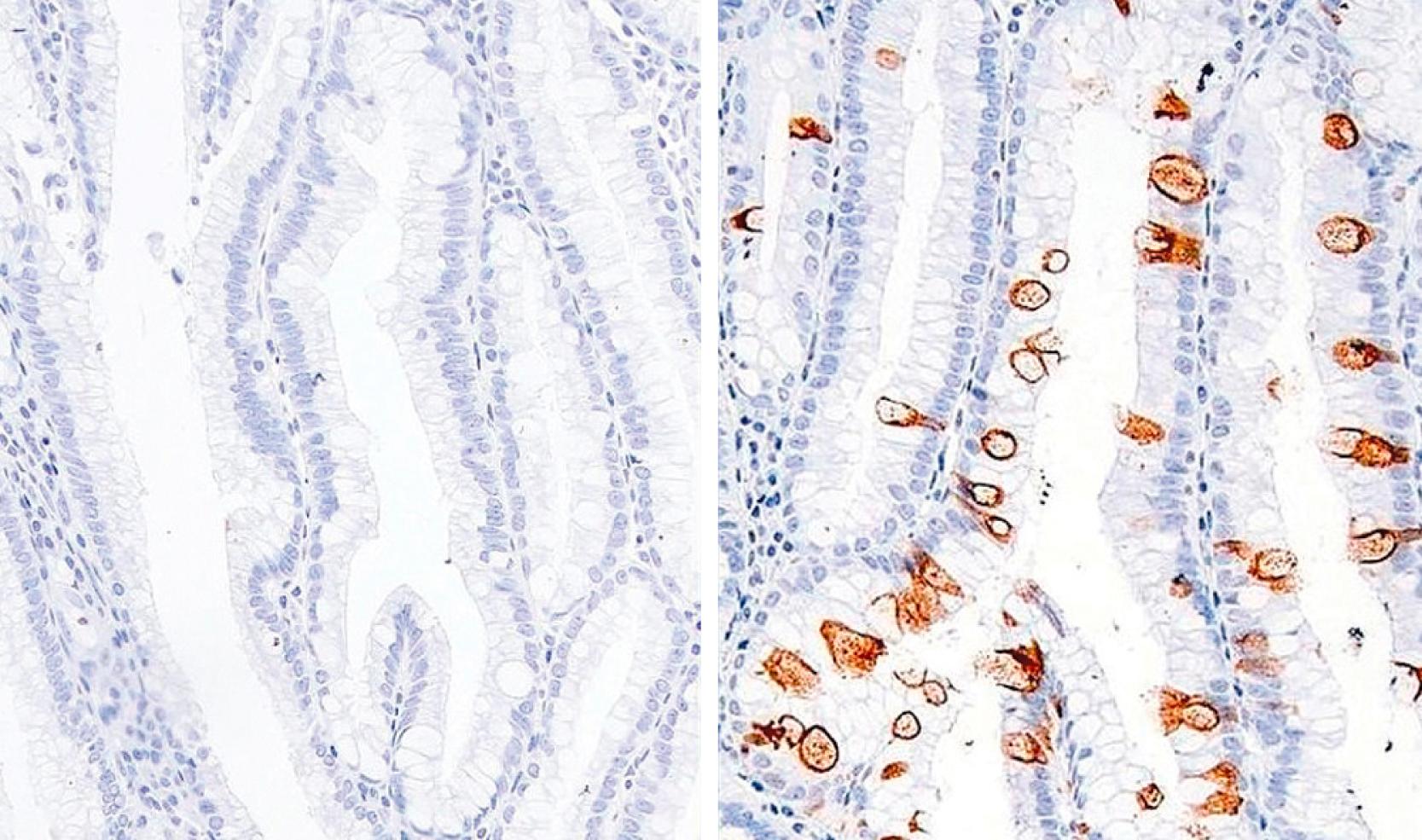
As expected, so-called pan-epithelial markers such as CAM 5.2, cytokeratin 8 (CK8), and CK18 are expressed in the pancreatic acini and ducts as well as in the extrahepatic and periampullary ducts ; however, certain subsets show differential expression patterns. Acinar cells generally do not label with AE1/AE3, CK7, and CK19 ( Fig. 15.1 ), whereas ductal cells are strongly positive for these markers. Both acini and ducts are typically negative for CK20, which is positive in the intestinal mucosa adjacent to the ampulla. In general, the expression of CKs, even the wide-spectrum CKs (CAM 5.2, AE1/AE3, CK8, and CK18), is typically less or absent in islet cells compared with other elements.
In the pancreas and ampulla, the glandular/ductal system is characterized and distinguished by mucin production. With the exception of centroacinar cells/intercalated ducts in the pancreas and the serous cystadenomas (SCAs) that presumably recapitulate this earliest component of the ductal system, virtually all glandular elements and their neoplasms exhibit some degree and some type of mucin formation. Among the mucin-related glycoproteins and oncoproteins that are commonly expressed in the glandular/ductal neoplasms of this region, the most widely used are MUCs, CA19-9, monoclonal carcinoembryonic antigen (mCEA), B72.3 (TAG-72), and ductal-of-pancreas-2 (DUPAN-2). Most of these are well described elsewhere in this book. Later, the ones more pertinent to pancreas are discussed.
MUCs are high-molecular-weight glycoproteins that are produced by various epithelial cells. They are categorized into membrane-associated mucins (MUC1, MUC3, MUC4, MUC12, MUC16, and MUC17), gel-forming mucins (MUC2, MUC5AC, MUC5B, and MUC6), and soluble mucin (MUC7). ,
MUC1, pan-epithelial membrane mucin or the “mammary-type” mucin, is constitutively expressed in the cell apices of the centroacinar cells, intercalated ducts, intralobular ducts, and focally in the interlobular ducts, but not in the main pancreatic ducts, acini, or islets. It is thought to have an inhibitory role in cell–cell and cell–stroma interactions and in cytotoxic immunity. MUC1 also appears to function as a signal transducer, closely interacting with the epidermal growth factor receptor (EGFR) family, and participating in the progression of carcinogenesis. It is expressed in almost all examples of pancreatobiliary type adenocarcinomas (invasive ductal adenocarcinomas [DAs] of the pancreas, cholangiocarcinomas of the bile duct, and a subset of ampullary adenocarcinomas that presumably arise from periampullary ductules). Whereas the expression is predominantly confined to the luminal membrane in the duct-forming areas, it is also intracytoplasmic in the poorly differentiated areas. Therefore, MUC1 is considered a marker of aggressiveness. ,
MUC2, intestinal type secretory mucin, goblet type mucin, or gel-forming mucin , is not constitutively expressed in the pancreas or ampullary ductules, with the exception of the scattered goblet cells, where it functions as a protective barrier. It is a product of the MUC2 gene, which is known to have tumor suppressor properties, and, as such, it is considered to be responsible for the more indolent behavior of the tumors. , Neoplasms with prominent intestinal differentiation, namely intestinal type pancreatic intraductal papillary mucinous neoplasms (IPMNs), colloid carcinomas that arise in association with IPMNs, and intestinal type adenocarcinomas arising from the ampulla/duodenum, all typically show diffuse expression of MUC2 as well as CDX2. CDX2 is a transcription factor responsible for intestinal programming and is also an important upstream regulator of MUC2. While diffuse expression of MUC2 is mostly confined to tumors with intestinal differentiation, CDX2 can be expressed to some degree in pancreatobiliary-type tumors as well.
Like MUC1, MUC4 is a membrane-associated mucin; however, it is not expressed in normal pancreatic tissue. It is less well studied, but preliminary evidence suggests that, like MUC1, MUC4 may be a marker of DA and a sign of aggressiveness. , Gastric type mucin s, especially those marking gastric surface-epithelial (foveolar) mucin, such as MUC5AC, are fairly ubiquitous in the gastrointestinal (GI) tract, including the ampulla, wherever there are gastric-like glands, as well as the tumors arising from these sites, presumably due to the close embryologic foregut association with pancreatobiliary tissue. However, normal pancreatic ducts do not express this marker. In recent studies, MUC5AC has been found to be marker of aggressive behavior both in the ampulla as well as in biliary tract. , Additionally, in the right context, it can be used to highlight subtle carcinoma cells such as in poorly cohesive cell carcinomas of the ampulla. The expression of MUC6, gastric pyloric glandular mucin or pyloric type mucin, is somewhat more restricted. In addition to decorating Brunner glands, the intercalated ducts of the pancreas, and the pyloric-like glands that occur in the walls of some preinvasive neoplasia such as IPMNs and mucinous cystic neoplasms (MCNs), MUC6 is also expressed extensively in some subsets of intraductal neoplasia that show oncocytic phenotype (intraductal oncocytic papillary neoplasms [IOPNs]), or those with nondescript morphology (“intraductal tubulopapillary neoplasms” [ITPN]). , It is also one of the defining characteristics of the intracholecystic tubular nonmucinous neoplasms of the gallbladder along with the mucinous pyloric gland adenoma type intracholecystic neoplasia.
It has long been known that trypsin, one of the best characterized serine proteinases, is produced as a zymogen (trypsinogen) in the acinar cells of the pancreas, is secreted into the duodenum, is activated into the mature form of trypsin by enterokinase, and functions as an essential food-digestive enzyme as well as catalyzes the cleavage of the other pancreatic proenzymes (chymotrypsinogen, prophospholipase, proelastase, and so on) to their active forms. , To date, four trypsin (or trypsinogen) genes—trypsin 1, 2, 3, and 4—have been characterized in humans, and three of them—trypsin 1, 2, and 3—have been demonstrated as the zymogens in human pancreatic juice. With the immunohistochemical methods, trypsin 1 can also be demonstrated in acinar cells as are the other pancreatic enzymes, such as chymotrypsin, lipase, amylase, and elastase. Ductal and neuroendocrine cells are typically negative for these enzymes. More important, although studies have shown that trypsins or trypsin-like enzymes are produced by other human cancer cells such as stomach, ovary, lung, colon, and others, immunohistochemical identification of pancreatic enzyme production is helpful in confirming the diagnosis of pancreatic acinar cell carcinoma (ACC) and other neoplasms with acinar differentiation including cystic acinar transformation, pancreatoblastoma, and mixed neoplasia. Although this requires confirmation, it has been reported that the tumor-derived trypsin is likely to contribute to tumor invasion and metastasis by degrading extracellular matrix (ECM) proteins and by activating the latent forms of matrix metalloproteinases (MMPs).
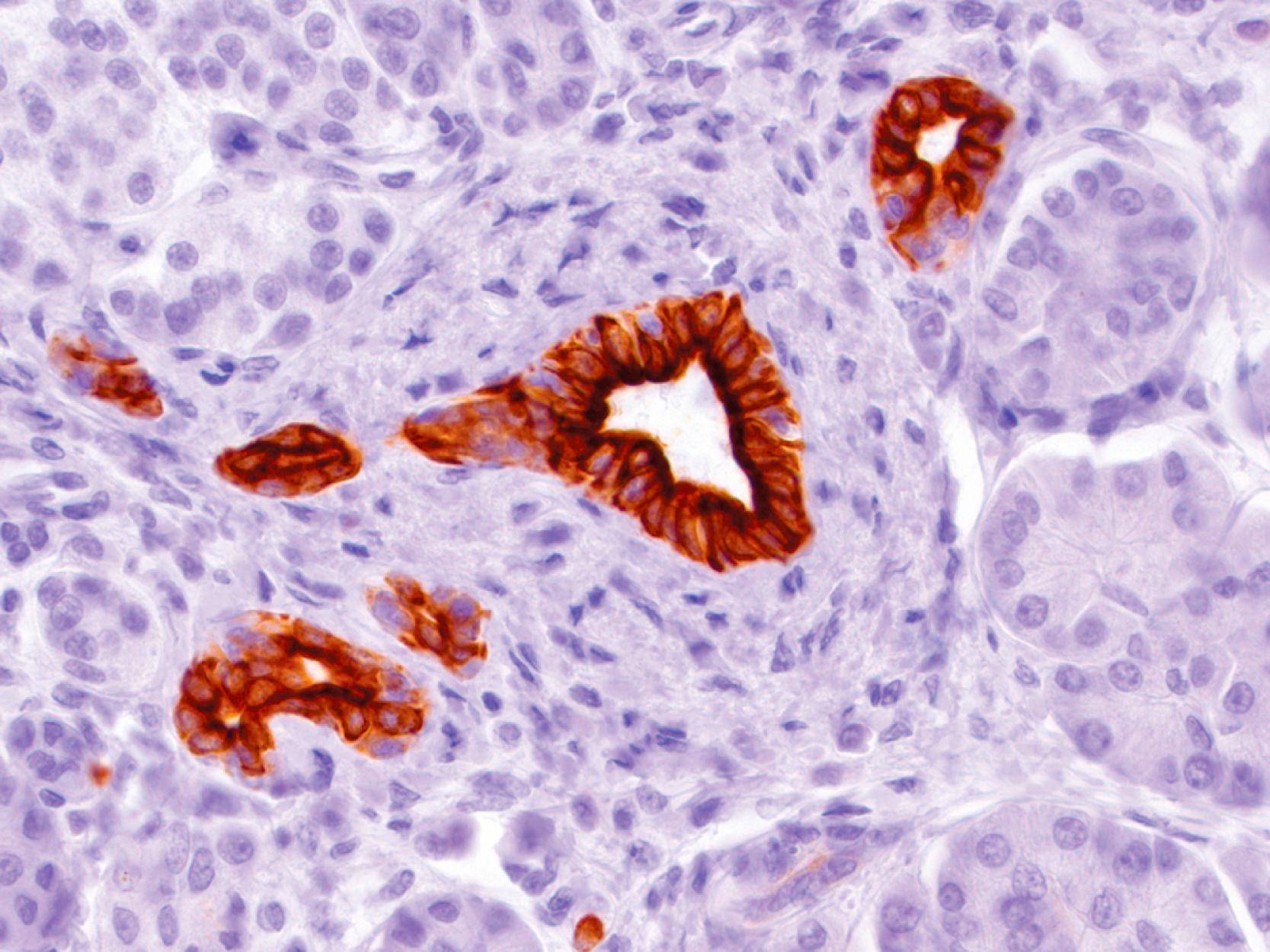
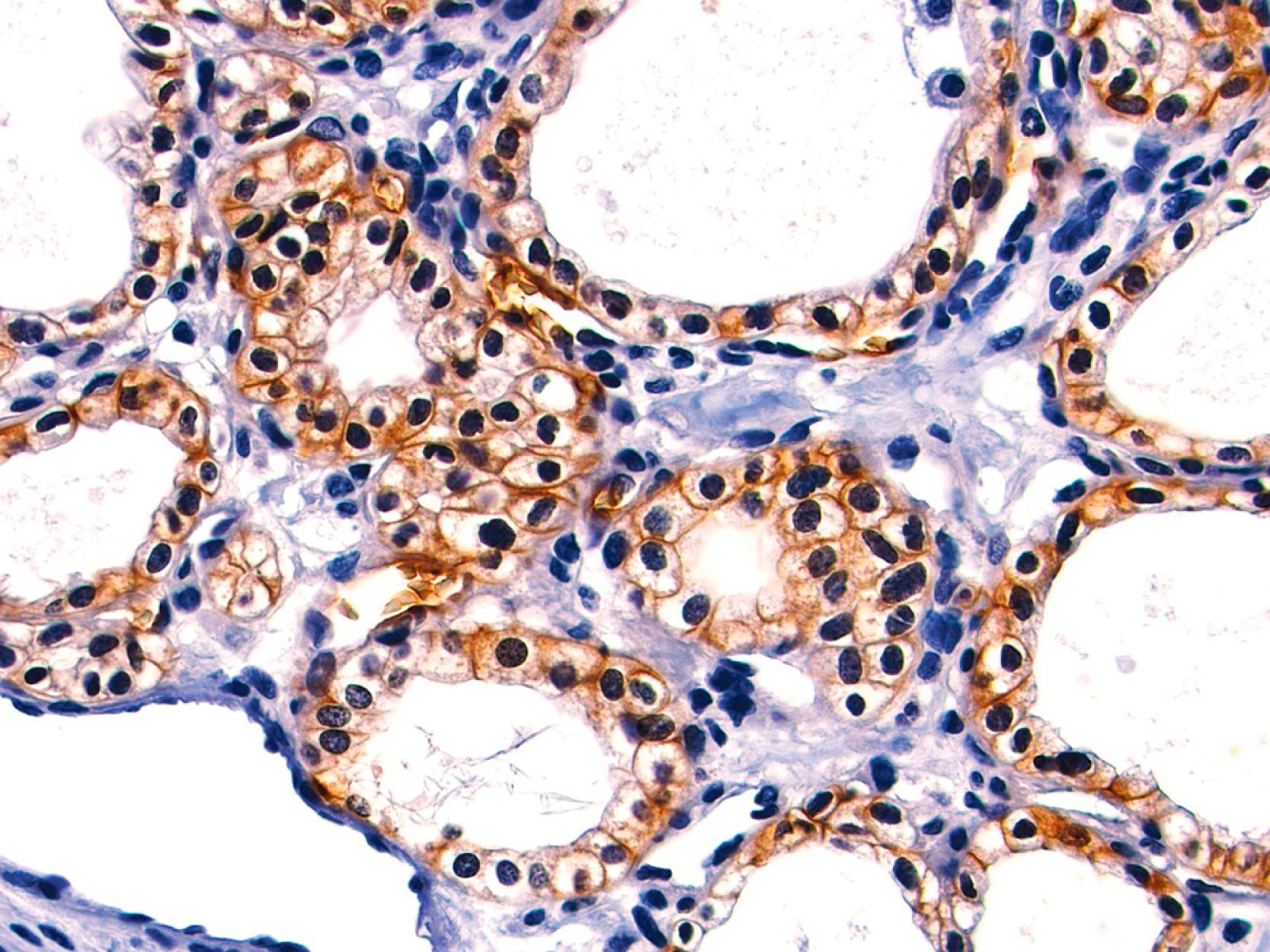
The immunohistochemical demonstration of the specific neuroendocrine cell peptides allows the classification of the pancreatic neuroendocrine neoplasms. However, it is not always possible to demonstrate these in pancreatic neuroendocrine neoplasms. Therefore, it is of diagnostic importance to use broad-spectrum neuroendocrine cell markers for the general identification of the neuroendocrine nature of islet cells and pancreatic neuroendocrine neoplasms. These protein markers, localized in the secretory granules in the cytosol or in the cellular membrane, present in most (rarely in all) normal and neoplastic neuroendocrine cells. The markers most commonly used in routine histopathology have been the secretory granule proteins chromogranin and synaptophysin, and the cytosolic enzyme neuron-specific enolase (NSE). As is well known, of these, chromogranin is the most specific, but unfortunately, its sensitivity is about 80% to 90% ( Fig. 15.2 ).
Chromogranins are a family of glycoproteins consisting of several members, chromogranin A, B, and C, and the proteins derived from them. Among these, particularly chromogranin A has attracted great interest. Different chromogranin A antibodies are commercially available, and the staining results with these antibodies may vary. Also, the intensity of chromogranin varies with the number of neurosecretory granules in the cytoplasm, which tend to be more abundant in the perivascular zones in normal islets.
Synaptophysin, also called protein p38, is a glycoprotein initially found in small vesicle membranes of neurons and of chromaffin cells in the adrenal medulla. It has been routinely used as a broad-spectrum marker in normal and neoplastic neuroendocrine cells including those of the pancreas; however, strong synaptophysin immunoreactivity has been well documented in tumors without any neuroendocrine differentiation, including solid-pseudopapillary neoplasm (SPN) of the pancreas, which is one of the most important differential diagnoses of neuroendocrine neoplasia in this organ.
NSE is a cytosolic isoenzyme of the glycolytic enzyme enolase, which catalyzes the conversion of 2-phosphoglycerate to phosphoenolpyruvate. It has been considered a marker for neuroendocrine cells and tumors, including pancreatic neuroendocrine neoplasms. Its staining intensity is unrelated to the content of secretory granules and their peptide storage. Therefore, NSE can immunostain even degranulated tumor cells. It may also be demonstrated in some nonneuroendocrine tumors. For this reason, it has also been dubbed as “nonspecific” enolase. Thus, it is important not to rely on NSE staining results alone, but always to use them in combination with other markers of neuroendocrine differentiation.
Cell membrane-associated proteins, such as neuronal cell adhesion molecule (NCAM or CD56) and leu-7 (CD57), have raised interest as neuroendocrine cell markers, but they lack specificity because they are also expressed in nonneuroendocrine cells and tumors.
Our own experience and analysis of the literature also indicate a high incidence of “unexpected” or “unexplained” positivity reported with various antibodies in the islets. For most of the antibodies, the staining pattern is faint and diffuse, without preferential staining pattern of the islet hormones, suggesting that it is a cross-reaction with a cytosolic component.
DNA mismatch repair proteins (MMR) are used as surrogate markers to test for microsatellite instability. Immunohistochemically, four markers (MLH1, MSH2, PMS2, and MSH6) are typically used in clinical practice. Loss of nuclear expression of any one of these markers warrant further analysis to determine whether the patient has microsatellite instability related cancer. MMR deficiency is exceedingly uncommon in pancreatic adenocarcinomas, and when seen it is typically in the very rare medullary phenotype. It is reported in a slightly higher percentage of gallbladder adenocarcinomas. In contrast, MMR deficiency is seen in about 15% of ampullary carcinomas. In the ampulla, medullary carcinomas, which are slightly more common than in the rest of pancreatobiliary tract, are commonly associated with MMR deficiency.
Cadherins are transmembrane glycoproteins that are prime mediators of cell-cell adhesion via calcium-dependent interactions. Different members of the family are found in different locations: for example, E-cadherin is found in epithelial tissue; N-cadherin is found in muscle and adult neural tissues; and P-cadherin is found in the placenta.
E-cadherin plays a key role in the maintenance of epithelial integrity and polarity function. , Normal E-cadherin immunoexpression is localized to the cell membrane with a crisp staining pattern. A decrease in membrane staining compared with normal or complete absence of staining (with the antibody raised against the extracellular domain of E-cadherin) and/or nuclear staining (with the antibody recognizing the cytoplasmic domain of E-cadherin), as seen in myriad invasive cancers, including SPNs of the pancreas, is regarded as abnormal. , Therefore, E-cadherin staining is of diagnostic use in the immunohistochemical workup of SPNs because all cases will show either absence of membrane staining or nuclear positivity depending on the antibody that is used. The exact mechanism by which E-cadherin enters the nucleus is not known, but it is considered that it is closely related to several partner molecules such as β-catenin. The cytoplasmic domain of E-cadherin interacts with the catenin molecules that mediate its binding to the actin cytoskeleton. Cytoplasmic dot-like staining has also been described with the antibody to full-length E-cadherin.
β-Catenin plays a key role in the Wnt signaling pathway as a transcriptional activator. Its normal immunoexpression shows distinct membrane decoration of the pancreatic acini and the ducts. Activating mutations in β-catenin (CTNNB1) result in (1) dysregulation and redistribution of β-catenin protein leading to characteristic strong cytoplasmic and nuclear immunoreactivity, which is seen in 100% of SPNs and in 50% to 80% of pancreatoblastomas, usually in the squamoid corpuscles (morules); and (2) over-expression of cyclin D1, which is variably reported in 74% to 100% of SPNs and in most pancreatoblastomas. Nuclear β-catenin expressing morules are also a defining characteristic of intracholecystic tubular nonmucinous neoplasms in the gallbladder.
Programmed death-ligand 1 (PD-L1), molecule involved in immune-avoidance, is over-expressed in some cancer cells, which allows them to escape the surveillance by T cells. Studies have suggested that immune checkpoint inhibitors that bind PD-L1 and block its binding to Programmed death 1 (PD-1) may render the cancer cells vulnerable to immune attack. Thus, immunohistochemical analysis for PD-L1 has been identified as a theranostic marker in select cancers. Unfortunately, this phenomenon appears to be rather limited in pancreatobiliary cancers, with the exception of perhaps ampullary cancers of especially medullary type.
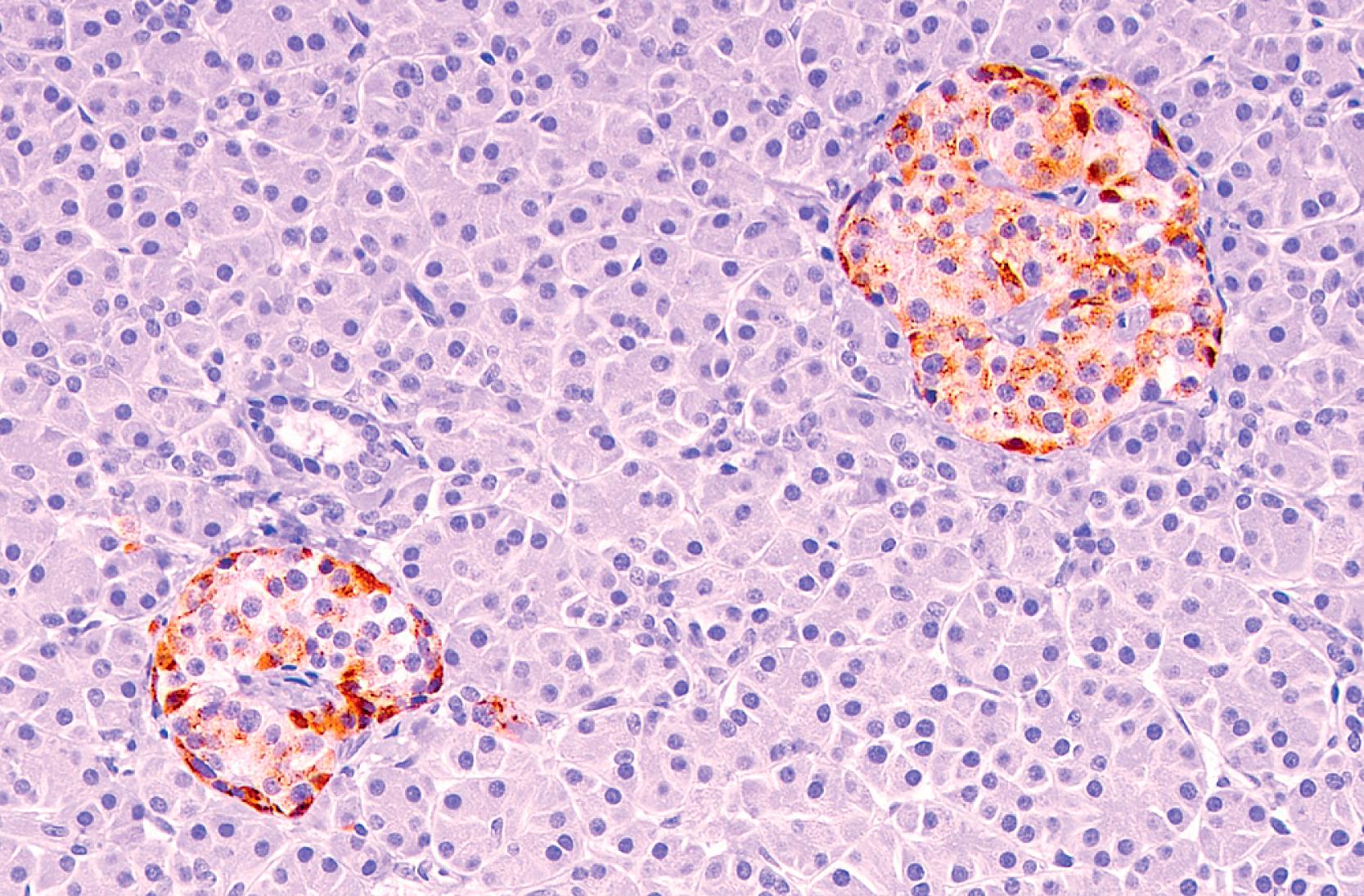
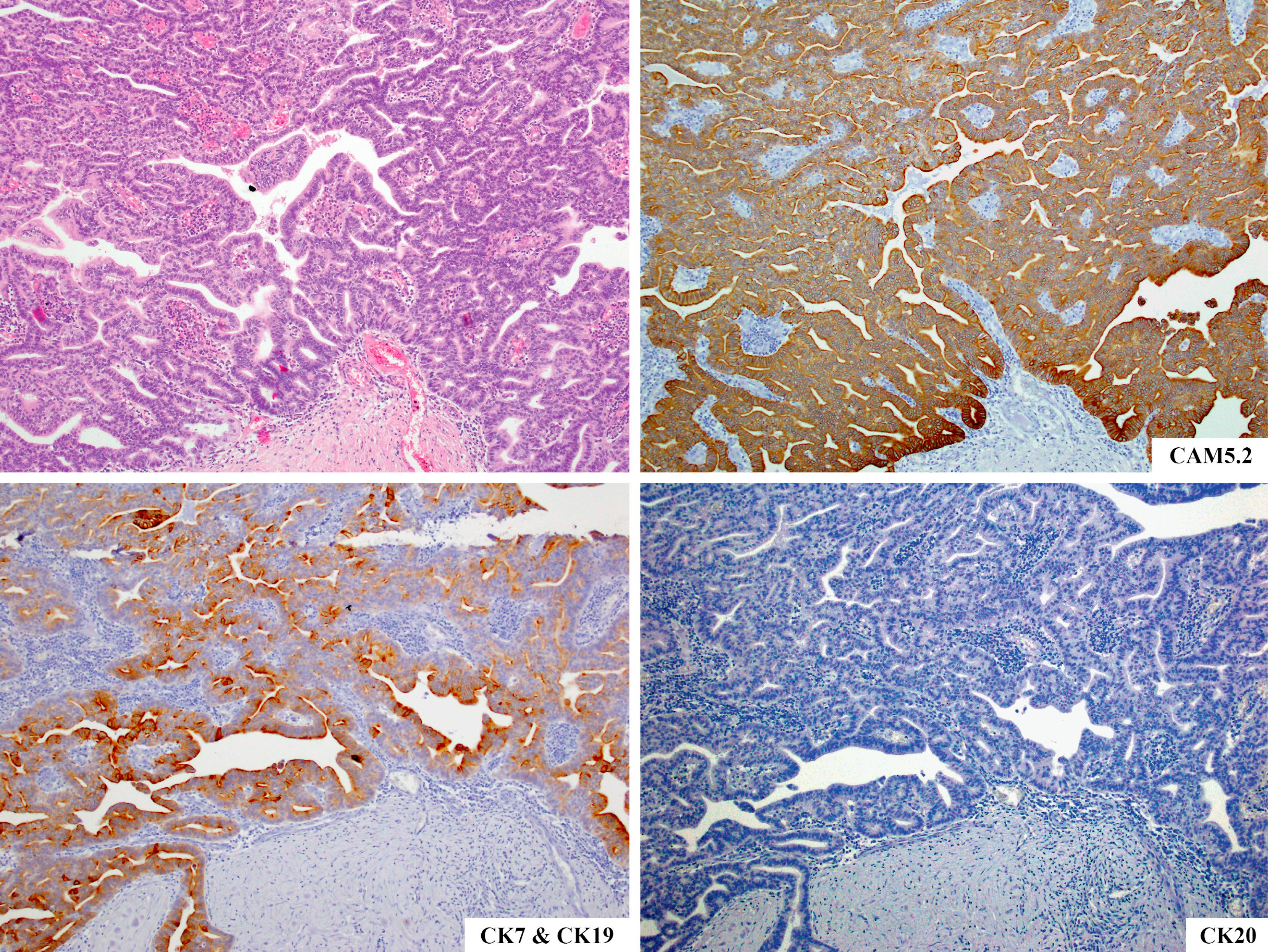
Ductal adenocarcinoma (DA) is the most common tumor of the pancreas (>85% of pancreatic tumors). It is now the third leading cause of cancer related deaths in the United States. It often forms a solid mass, which can be closely mimicked by pancreatitis, and therefore most of the cases require fine needle aspirate (FNA) or core biopsy for diagnosis. Unfortunately, the tumor is usually scirrhous, has an abundant stromal component, and has a very low tumor cell yield, which makes the diagnosis of DA one of the most challenging in surgical pathology. Moreover, DA also has very insidious growth pattern, and, in fact, along with ovarian cancer, it is the most common cause of “intraabdominal carcinomatosis” and is one of the most common sources of carcinomas of unknown primary. Therefore, it is important to know its immunolabeling pattern ( Fig. 15.3 ).
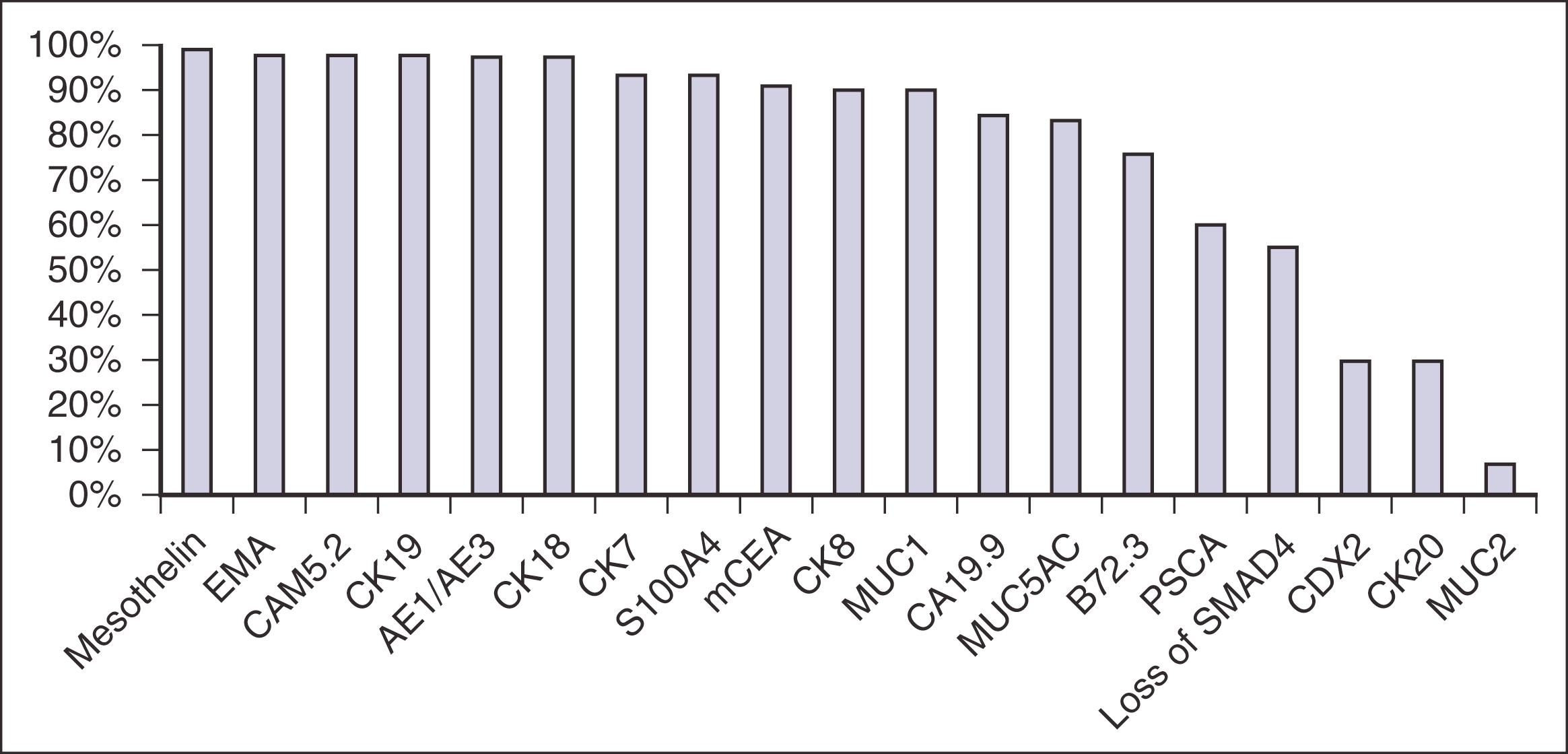
DAs express CKs and epithelial membrane antigen (EMA). The keratins expressed consistently are CK7, CK8, CK18, CK19 (as normal ductal cells), CK13, and (in a lesser percentage) CK4, CK10, CK17, and CK20. Although CK7 is expressed relatively diffusely and strongly in the vast majority of the cases ( Fig. 15.4A ), CK20 expression is less common, is detected in about one-third of the cases, and is usually focal (see Fig. 15.4B ). , , , , , , , This pattern of immunolabeling can be diagnostically useful, as most acinar and neuroendocrine neoplasms of the pancreas do not express CK7, and most colorectal cancers express CK20 but minimal CK7. Areas of squamous differentiation in DA are also appropriately CK5/6 and p63 positive ( Fig. 15.5 ). , , Molecular profiling studies have identified a “basal-like” subtype of DA, which seems to encompass the aggressive adenosquamous carcinomas. , GATA6 has been identified as a distinguishing marker of these subtypes but more studies are needed in this regard. ,
As mentioned previously, DAs express several mucin-related glycoproteins, including MUC1 ( Fig. 15.6 ), which is reported to be associated with a poorer prognosis, MUC3, MUC4, MUC5AC, and in a lesser percentage MUC6, , , , but not MUC2. MUC2 is virtually nonexistent in DAs unless there is focal mucinous differentiation or there are metaplastic goblet cells. The intestinal differentiation marker CDX2 is also positive in only about 30% of DAs, and its labeling is typically faint and variegated compared with colonic adenocarcinomas.
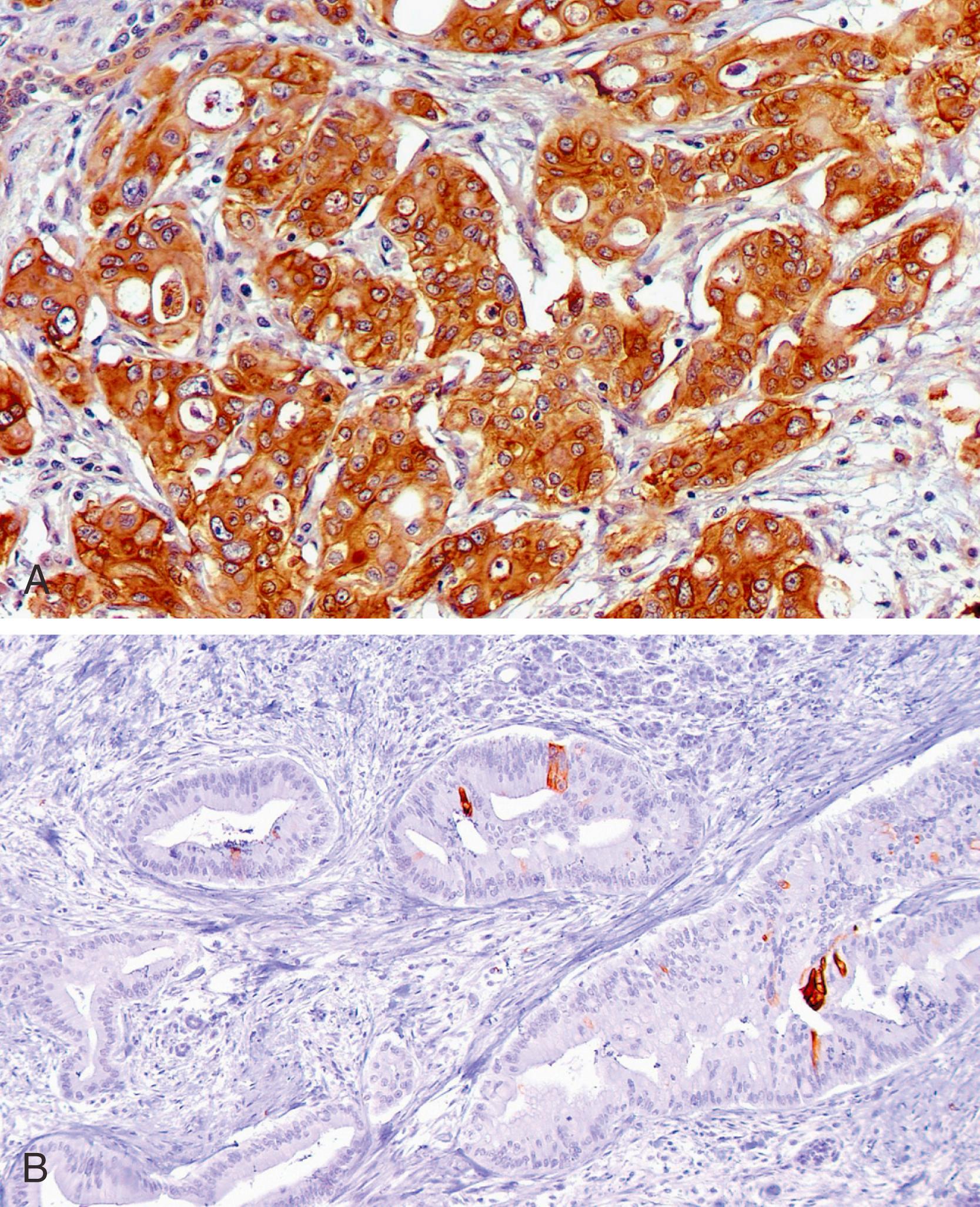
Oncoproteins that are widely expressed in DAs include CA19-9, mCEA, B72.3 (TAG-72), DUPAN-2, and CA125. The expression of mCEA ( Fig. 15.7 ), B72.3, and CA125 may be useful in distinguishing DA or high-grade PanIN from reactive glands, as nonneoplastic glands are often negative or only focally positive for these markers. However, caution needs to be exercised because overlap is common. Moreover, even the low-grade PanIN can express these markers. Recently, another glycoprotein, CEACAM1 (a member of the CEA family), has been reported to be positive in DA and not in a normal pancreas or in chronic pancreatitis, and that serum levels of CEACAM1 might serve as a useful indicator for the presence of pancreatic cancer.
DAs are typically negative for pancreatic enzymes, such as trypsin, chymotrypsin, and lipase, , unless there is a mixed acinar component, which is very uncommon. They also fail to label with neuroendocrine markers; however, in 30% of DAs, there are scattered, possibly nonneoplastic, neuroendocrine cells in close association with the neoplastic cells, which can be highlighted with immunohistochemical stains for chromogranin A, synaptophysin, and NSE. The latter two markers can occasionally show more diffuse expression, which should not be regarded as evidence of “neuroendocrine differentiation” unless the tumor also shows convincing neuroendocrine morphology.
The desmoplastic stroma associated with DAs expresses a variety of inflammatory and stromal markers. The inflammatory cells are mostly T cells (CD3 positive). Scattered B cells (CD20 positive) and macrophages (MAC387 and KP1 positive) are also usually present. The spindle cells express α-smooth muscle actin, smooth muscle myosin heavy chain, and collagen IV, markers of myofibroblastic differentiation. They are also reported to be positive for heat shock protein (HSP) 47 and fibronectin, as well as for proteins associated with tissue remolding, such as urokinase-type plasminogen activator, the MMPs, and the tissue inhibitors of metalloproteinases. These do not appear to have any clinical application as of yet.
It has been recognized that DA, like other malignant processes, is a genetic disease produced by progressive mutations in cancer-related genes although it is being recognized that local milieu changes may be the instigator of the molecular alterations. ,
Numerous studies have shown that inactivation of TP53 gene occurs in 50% to 80% of cases. However, it is well known that immunolabeling for the p53 protein is not entirely specific for a TP53 gene mutation.
DPC4 ( D eleted in P ancreatic C arcinoma locus 4 ) or SMAD4 ( M others A gainst D ecapentaplegic homolog 4 ) gene is inactivated in approximately 55% of the DAs but practically never in benign conditions. , Immunohistochemical labeling for the SMAD4/DPC4 gene product has been shown to mirror SMAD4/DPC4 gene status. Therefore the immunohistochemical absence of its protein product in the ductal epithelium of a biopsy specimen is strongly suggestive of carcinoma , as long as the in-built controls are labeling properly. Also, inactivation of the DPC4 gene is relatively uncommon in nonpancreatobiliary carcinomas; thus, the loss of DPC4 may also serve as a marker of a pancreatic DA in small FNA samples and in metastatic sites. ,
P16/CDKN2A is inactivated in approximately 95% of DAs (75% to 80% genetic inactivation plus 15% silencing by hypermethylation) , , ; however, a minority of benign ductal epithelial cells also labels for its protein product (p16); loss of p16 is not diagnostic of carcinoma. , , ,
The oncogene most frequently activated in pancreatic cancer is the KRAS oncogene, which is discussed later, but a number of other oncogenes can be activated in DA, including HER2/neu (over-expressed in approximately 70% of cases) and AKT2 (amplified in 10% to 20% of cases). ,
Gene expression analyses of DA have identified a large number of genes that are differentially over-expressed in DA compared with normal pancreatic tissue. Among them, mesothelin is expressed in close to 100% of Das, , sea urchin fascin in 95%, , a number of S100 protein subtypes in 93%, 14-3-3σ in 90%, and prostate stem cell antigen (PSCA) in 60%. The concurrent use of KOC and S100A4 protein has been found in some studies to improve the diagnostic sensitivity of biliary brushings cytology and demonstrates similar specificity as cytology alone in the diagnosis of pancreatobiliary malignancy. In addition, secreted or membranous proteins expressed in pancreatic cancer, such as mesothelin or PSCA that are shed into pancreatic secretions or blood, are under scrutiny as potential future markers for primary or recurrent disease.
DNA ploidy analyses have yielded aneuploid patterns in about half of the tumors, with the incidence being higher in the poorly differentiated forms. Also, cytogenetic analyses of large series have revealed recurrent patterns of alterations in specific chromosomes, such as the most frequent whole chromosomal gains being chromosomes 20 and 7 and the most frequent whole chromosomal loss being chromosomes 18. , MicroRNAs, small noncoding RNAs that negatively regulate gene expression, are also altered in DA.
A number of studies have identified that STK11/LKB1 Peutz-Jeghers gene, a tumor suppressor gene, is inactivated in a minority (5%) of DAs. This is clinically important, because patients with the Peutz-Jeghers syndrome have a greater than 130-fold increased risk of developing pancreatic cancer. STK11/LKB1 Peutz-Jeghers gene is also commonly altered in IPMNs (see later).
Among all human cancers, DAs have the highest frequency of KRAS alterations, the oncogene being constitutively activated in approximately 90% of DAs. , , , However, KRAS mutations are seen even in the earliest forms of neoplastic transformation (low-grade PanIN), a very common incidental finding in the pancreas, as well as in patients with chronic pancreatitis lacking invasive carcinoma, , and thus is by no means specific for “cancer.” Other oncogenes that are found to be activated in pancreatic cancer include AIB1 (amplified in 60%), BRAF (mutated in one-third of the small minority of cancers with wild-type KRAS ), c-MYC , and c-MYB. , ,
Unlike ampullary carcinomas, which have substantial association with microsatellite instability (MSI, about 15% ), MSI is an extremely rare event in DAs, and such cancers appear to have a distinct morphology called “medullary” , , , (see later), and an improved survival rate relative to those with conventional DAs. , , , The MLH1 gene is typically the one that is inactivated in MSI-high pancreatic medullary carcinomas (characterized with loss of expression of hMLH1 gene at the immunohistochemical level) either by mutation or hypermethylation. ,
Recently, BRCA has attracted much attention. BRCA alteration is detected in <5% of DAs, but this subset seems to benefit notably from certain targeted therapies, in particular poly (ADP-ribose) polymerase (PARP) inhibitors.
Undifferentiated examples of DA, which are now regarded separately from ordinary DA (see section below), include multiple distinct subsets including SMARC-deficient ones (characterized by loss of INI-1, BRM and BRG1, which are highly aggressive) and osteoclastic ones, which appear to be more indolent. ,
Genomic profiling studies have identified distinct clusters, similar to those in the breast, such as basal-like subtype, which appears to include adenosquamous cancers. , In some studies, GATA6 has been found to be a discriminator of this subtype. ,
DAs are consistently positive for CK7 diffusely and strongly, while CK20 is often either focal or absent.
Several mucin-related glycoproteins (MUC-1, MUC3, MUC4, and MUC5AC) and oncoproteins (CA19-9, mCEA, B72.3, and CA125) are also typically positive in DAs to variable degrees. None of these are entirely specific for this tumor type.
Scattered, possibly nonneoplastic, neuroendocrine cells in DAs can be demonstrated with immunostains for chromogranin A, synaptophysin, and NSE.
Loss of DPC4 staining in the pancreatic ductal epithelium is suggestive of carcinoma provided that this loss is confirmed by the presence of in-built controls. DPC4 may also prove to be a helpful marker for differentiating pancreatic adenocarcinoma from other carcinomas in small FNA samples and in metastatic sites.
Genomic profiling studies have identified “classical” and “basal-like,” but more studies are needed to establish their identity and significance.
Strong cytoplasmic expression of MUC1 and mCEA, which is often coupled with antigen leakage into stroma, is highly indicative of carcinoma (more common in high-grade areas).
p53 is significantly more abundant in carcinoma than in normal epithelium, although overlaps are common, and ought to be used cautiously.
Loss of DPC4 (SMAD4) is also a finding strongly in favor of adenocarcinoma, provided that in-built controls are working properly.
Colon versus DA: DA is consistently positive for CK7 diffusely and strongly. About one-third of DA express CK20, SATB2, and CDX2, but the expression is usually focal and weak. Colon carcinomas are negative for CK7, and they almost always express CK20, SATB2, and CDX2. Additionally, while DA is MUC1+/MUC5AC+/MUC2−/SMAD4-loss, colon carcinoma is more commonly MUC1−/MUC5AC−/MUC2+/SMAD-retained.
Lung versus DA: TTF-1 and surfactant apoprotein A (PE-10) are usually positive in lung adenocarcinomas and are negative in DAs. In contrast, antibodies that can be focally positive in DAs, such as CK20, CDX2, and CA125, are negative in lung carcinomas.
Müllerian (GYN-tract) versus DA: A panel composed of WT1, PAX8, MUC5AC, and CK20 is advisable in distinguishing ovarian serous carcinomas from DAs in omental or peritoneal biopsies, which often proves to be a challenging differential diagnosis. WT1−/MUC5AC+ phenotype would point toward DA, while WT1+ PAX8+/MUC5AC− is highly in favor of ovarian primary. If present, CK20 and, less reliably, CDX2 would also be more compatible with a diagnosis of DA. In one study, extensive CK17 reactivity has also been found to be supportive of a DA when the differential diagnosis includes ovarian serous and mucinous neoplasms.
Those rare DAs that lack hallmarks of ductal differentiation, including tubular configuration and intracytoplasmic mucin that may be focal, are classified as “undifferentiated carcinoma” if they constitute the majority of the tumor. , In some, epithelial-to-mesenchymal transition can be so complete that the tumor may resemble sarcomas (i.e., sarcomatoid carcinoma) and only after adjunct studies such as IHC that the ductal nature of the tumor can be elucidated.
Some are pleomorphic epithelioid carcinomas that often show bizarre tumor giant cells (not to be confused with the osteoclastic examples discussed separately below). Immunohistochemically, CKs are expressed in the well-formed epithelial component that these tumors often (but not always) contain in thorough sampling. Keratin expression may be diminished in the sarcomatoid component, might be negative or focal/weak positive, hindering the differential diagnosis with sarcomas. , , It should be kept in mind that sarcomas are exceedingly uncommon in the pancreas, and any sarcomatoid neoplasm ought to be regarded as suspect carcinoma rather than sarcoma. The keratin with the most diffuse and strongest staining has been reported to be the monoclonal so-called pan-cytokeratins (AE1/AE3 or OSCAR) ; however, these are also the keratins that are more prone to be expressed in true sarcomas. CAM 5.2, CK7, CK8, CK18, and CK19 are also positive in a variegated and less intense pattern. , , As is typical of most undifferentiated carcinomas, the neoplastic cells diffusely and strongly stain with vimentin. , , , They may also express MUC1, CA19-9, mCEA, and DUPAN-2. , EMA and B72.3 are negative in the majority of cases. Immunolabeling for chromogranin, synaptophysin, and NSE is also negative. , Recently, it has been demonstrated that noncohesive pancreatic cancers, including undifferentiated pancreatic carcinomas, are characterized by the loss of E-cadherin protein expression, which might explain the poor cohesion of many undifferentiated carcinomas.
Distinct types of undifferentiated carcinomas are being recognized in the pancreas and they appear to have different clinicopathologic characteristics, but more studies are needed to further establish their identity, associations, and biological behavior.
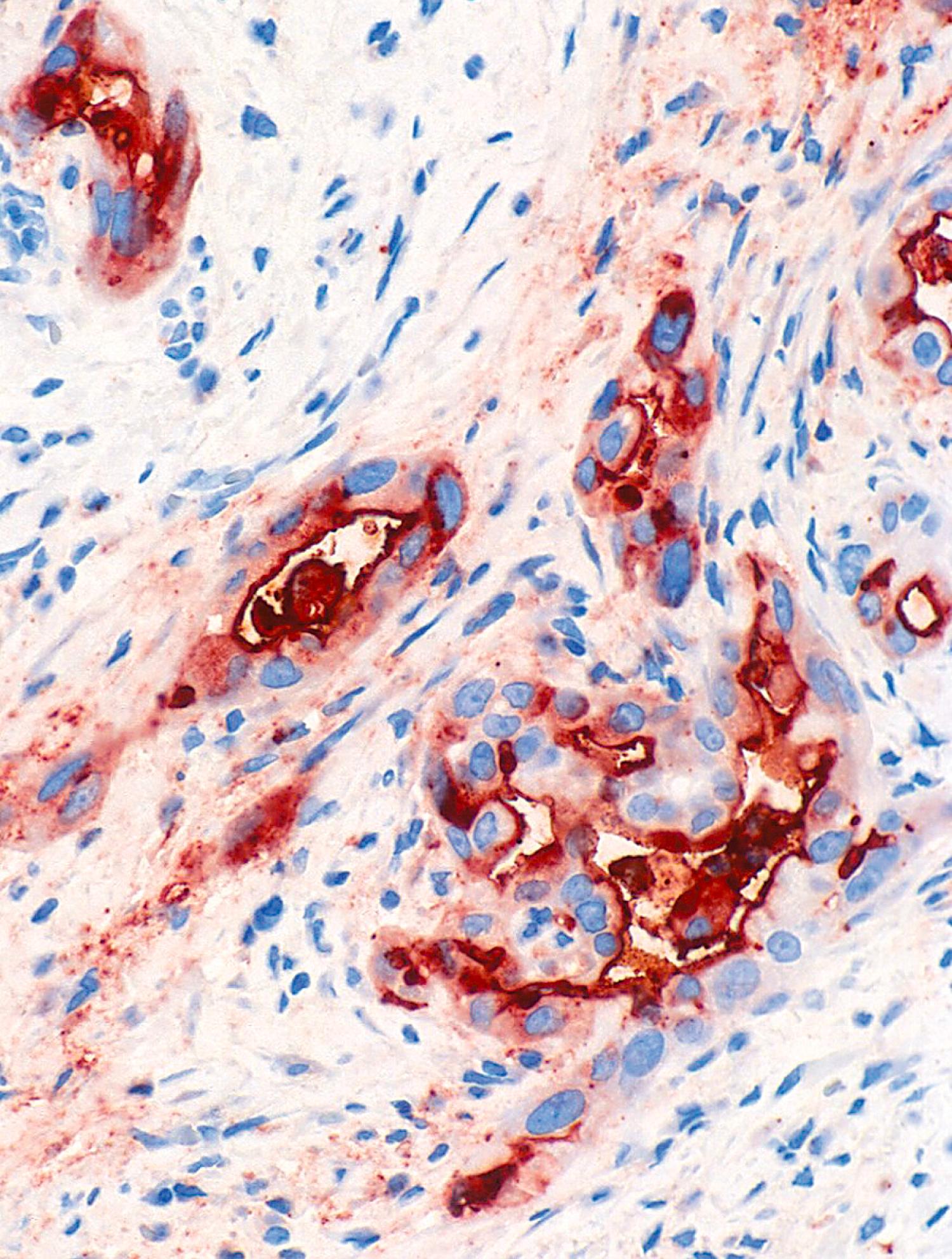
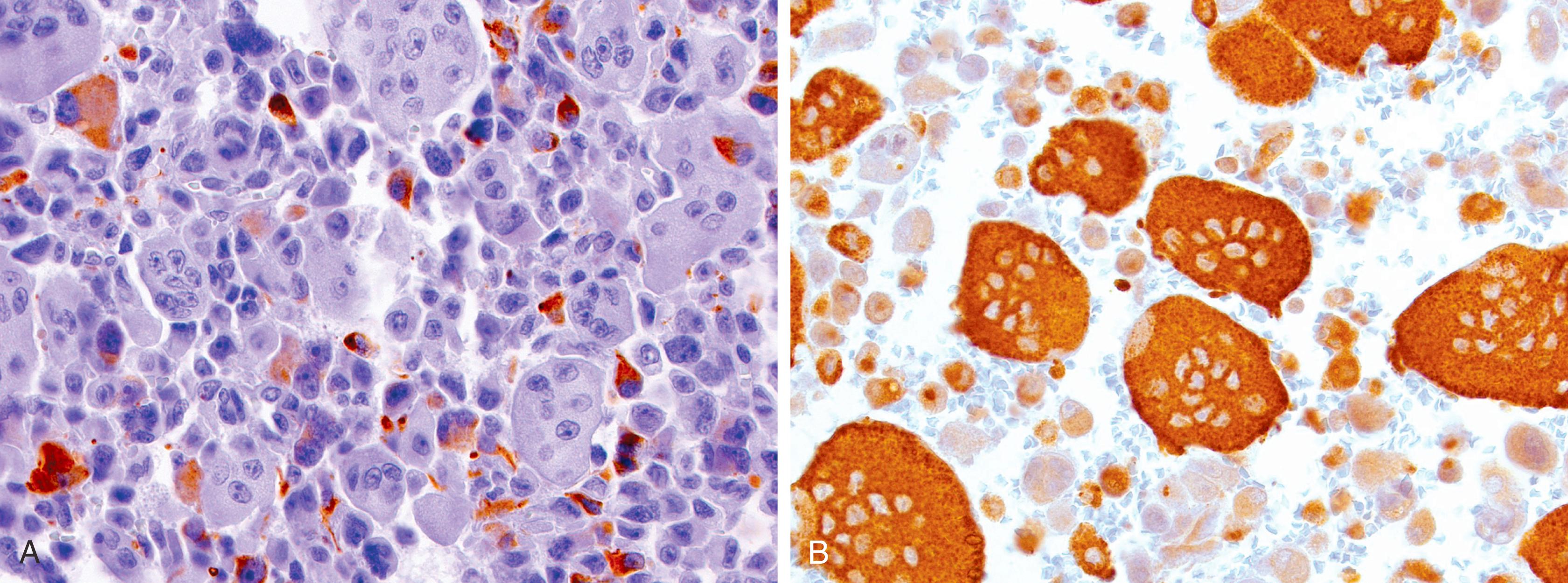
This is a distinct type of sarcomatoid carcinoma characterized by the presence, and often abundance, of osteoclasts, and it appears to have different properties including a more indolent behavior. , , OGCs are highly uncommon outside the pancreas. Osteoclastic giant cells are indeed osteoclastic, reactive in nature, and the malignant cells are actually the smaller, atypical mononuclear cells in the background. , It is not clear how these osteoclastic cells are recruited to these tumors in such abundance. Immunohistochemically, the atypical mononuclear cells in the background, which are the true malignant cells representing the sarcomatoid carcinoma cells, almost always express vimentin, while only a minority express CKs (CAM 5.2, AE1/AE3, or CK7; Fig. 15.8A ), EMA, and mCEA. , , , , , In some cases, all of the epithelial markers are negative. The osteoclastic giant cells are positive for vimentin, leukocyte common antigen (LCA, CD45), and histiocytic markers (CD68; see Fig. 15.8B ), while being nonreactive for CKs, EMA, or mCEA. , , , , However, “tumor cannibalism,” that is, the presence of malignant cells in the benign giant cells, is fairly common in this entity and ought to be considered in evaluating these markers. Heterologous stromal elements, there may be immunoreactivity consistent with the line of mesenchymal differentiation (e.g., myoglobin or myogenin in striated muscle, S100 protein in chondroid elements).
Rhabdoid (epithelioid) examples of undifferentiated carcinoma in the pancreas often represent a SMARC-deficient pathway, , which can be illustrated by immunohistochemical loss of INI-1, BRM, or BRG1 expression in the nuclei. These appear to be highly aggressive. ,
DAs develop through a multistep process that is initiated by an early activating KRAS mutation. Recent findings suggest that subsequent KRAS copy number changes and resulting KRAS mutant allele specific imbalance in a subset of cases may lead to the progression to undifferentiated carcinomas. It seems that KRAS mutant allele specific imbalance develops predominantly through KRAS amplification and/or chromosome 12 hyperploidy, monosomy, and correlates with worse survival.
These neoplasms often have TP53 gene mutations, and immunolabeling for the p53 protein has been shown to label the pleomorphic mononuclear cells but not the osteoclast-like giant cells. Additionally, genetic analyses have demonstrated that the atypical mononuclear cells harbor KRAS mutations in about 90% of these neoplasms. , , , , , By contrast, the osteoclast-like giant cells do not harbor KRAS mutations. ,
As in other organs (such as breast and tubular GI tract), medullary carcinoma in the pancreas is defined as syncytial growth of poorly differentiated epithelioid tumor cells, often accompanied by dense lymphoplasmacytic inflammatory infiltrate. , , , Desmoplastic reaction is minimal. , , , The tumors may arise sporadically or in patients with the hereditary nonpolyposis colorectal cancer (HNPCC) syndrome. Current experience is too limited to determine their biological behavior and prognosis; however, in one study, the patients were found to have an improved survival rate relative to those with DAs. Immunohistochemically, the epithelioid cells are labeled by antibodies to CK, , , , whereas trypsin, chymotrypsin, lipase, chromogranin, and synaptophysin are usually negative. CD3 antibody highlights the presence of numerous intratumoral T lymphocytes. Rare examples also contain Epstein-Barr virus (EBV) RNA.
Medullary carcinomas of the pancreas, like their colorectal counterparts, often show MSI, which is usually caused by somatic hypermethylation of the MLH1 promoter in sporadic cases and by an inherited mutation in one of the DNA mismatch repair genes ( MLH1 , MSH2 , and so on) in patients with HNPCC syndrome. Immunolabeling for MLH1 and MSH2 reveals a loss of expression of one of these DNA mismatch repair proteins in many cases.
The diagnosis of a medullary carcinoma has therapeutic implications. Although this is not studied thoroughly in the pancreas, patients with microsatellite-unstable medullary colorectal adenocarcinomas do not benefit from fluorouracil-based chemotherapy.
In the pancreas, squamous cells can be encountered in injured ductal epithelium as a result of a metaplastic process. The same metaplastic phenomenon also seems to take place focally in some examples of DA. When this finding is prominent (>30% of the tumor is the cutoff we use), the tumor is classified as adenosquamous carcinoma, and if it is exclusively squamous, then squamous cell carcinoma. Most of the tumors express CKs (CAM 5.2, AE1/AE3, CK5/6, CK7, CK8, CK13, CK18, CK19, and CK20), EMA, CA19-9, mCEA, and B72.3. , Typically, CK5/6, CK13, and p63 (see Fig. 15.5 ) are limited to the areas of squamous differentiation, whereas CK7, CK20, CA19-9, mCEA, and B72.3 often label to the glandular elements. , ,
The majority of the cases show nuclear p53 staining and loss of DPC4 protein similar to the molecular signature found in DA. KRAS mutations are seen in the majority of cases. ,
Genomic profiling studies have identified distinct clusters, similar to those in the breast, such as basal-like subtype, which appears to include adenosquamous cancers. , In some studies, GATA6 has been found to be a discriminator of this subtype. ,
Colloid carcinomas are characterized with well-delineated pools of stromal extracellular mucin containing scanty, floating carcinoma cells in clusters, strips, or as individual cells. By definition, mucin/epithelium ratio is typically very high. , They appear to have a distinctly better clinical course than other invasive carcinomas of ductal origin. , Five-year survival rates of resected cases is almost 75%, compared with 20% to 40% for those resected for DAs. The indolent behavior has been attributed to a combination of two factors: (1) there is an inverse polarization of cells, which show secretory activity toward the “stroma-facing” surface of the cells, instead of the luminal surface, and (2) the mucin produced is a specific gel-forming mucin (MUC2) that acts as a containing factor, preventing the spread of the cells. ,
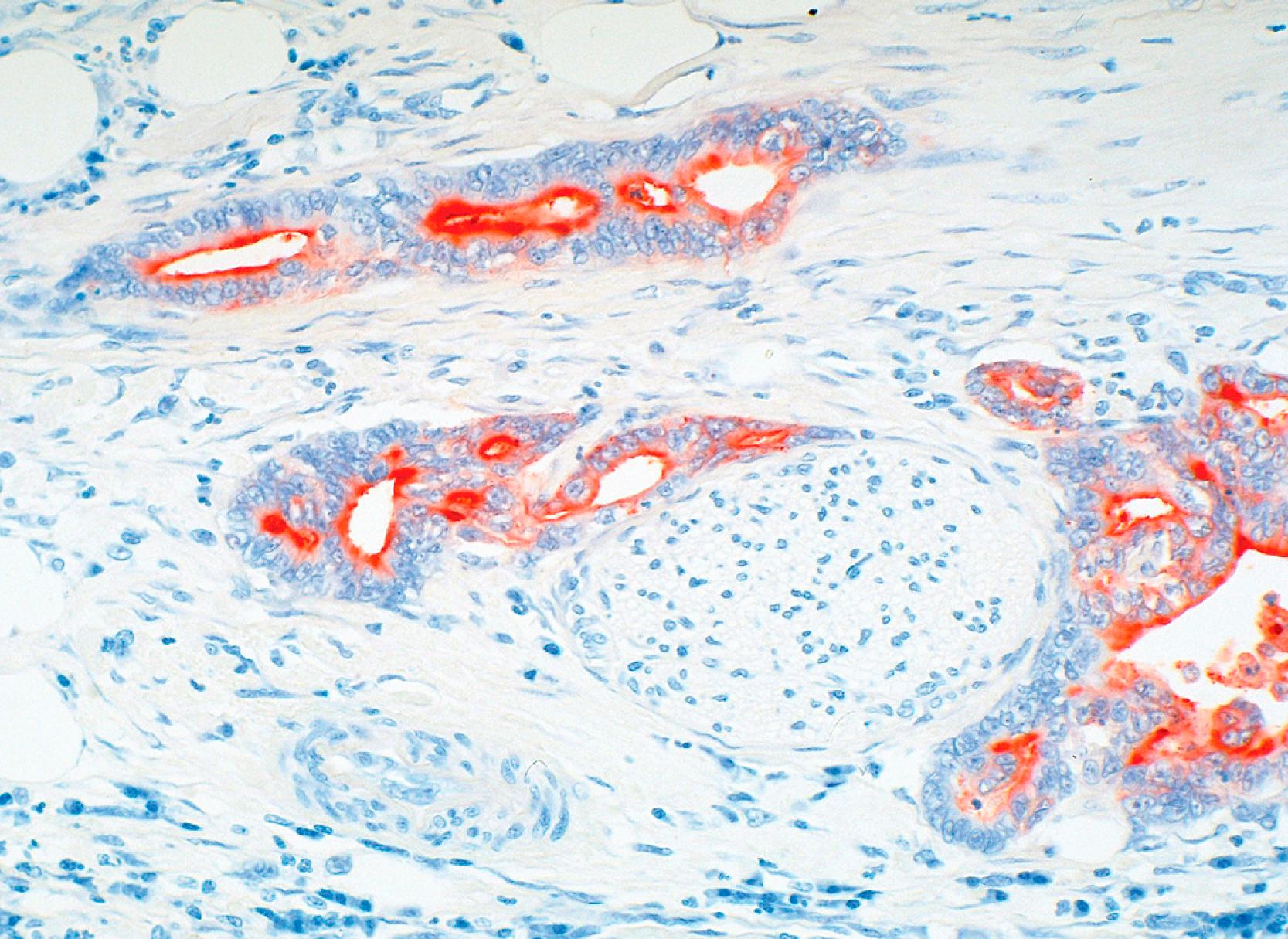
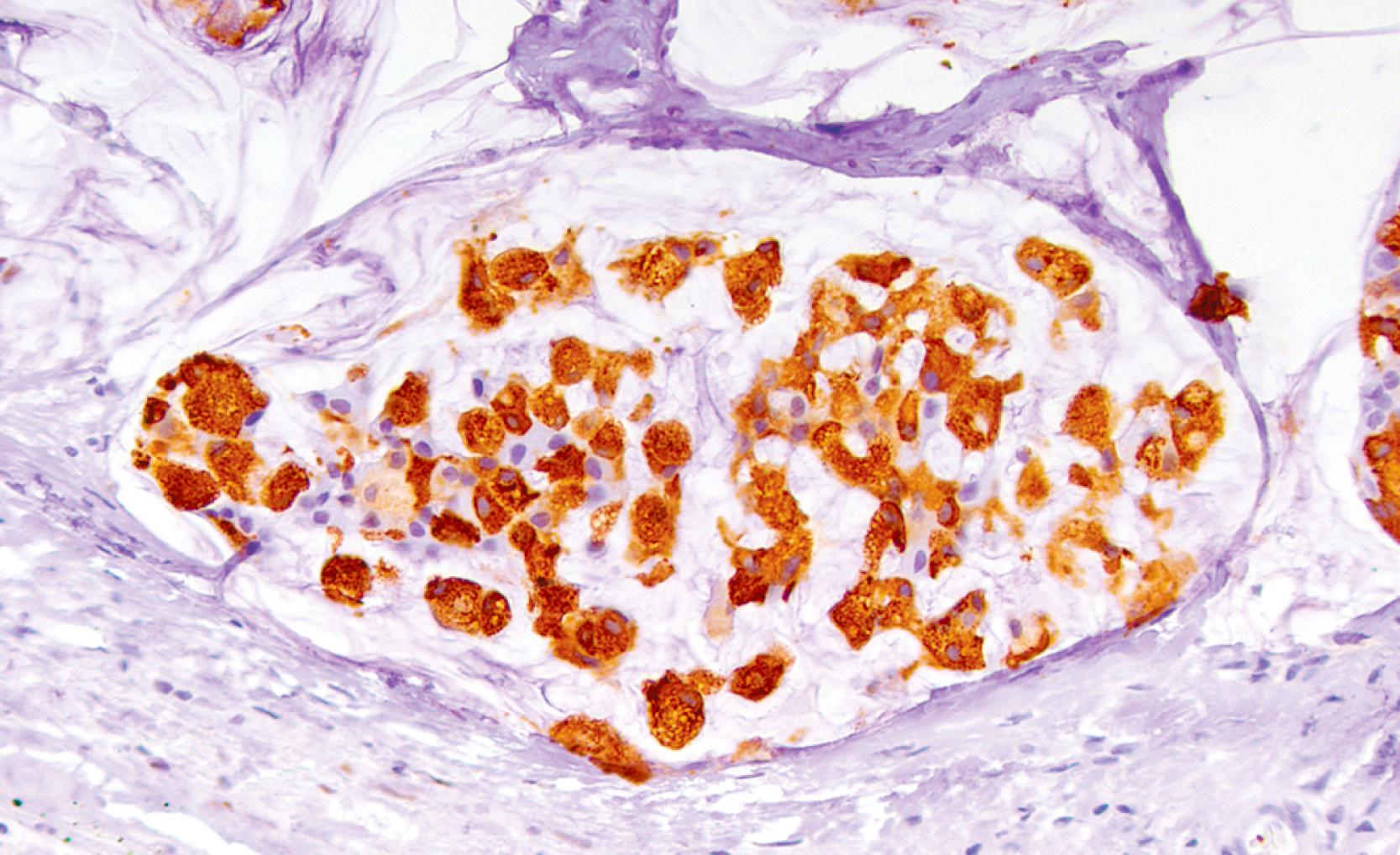
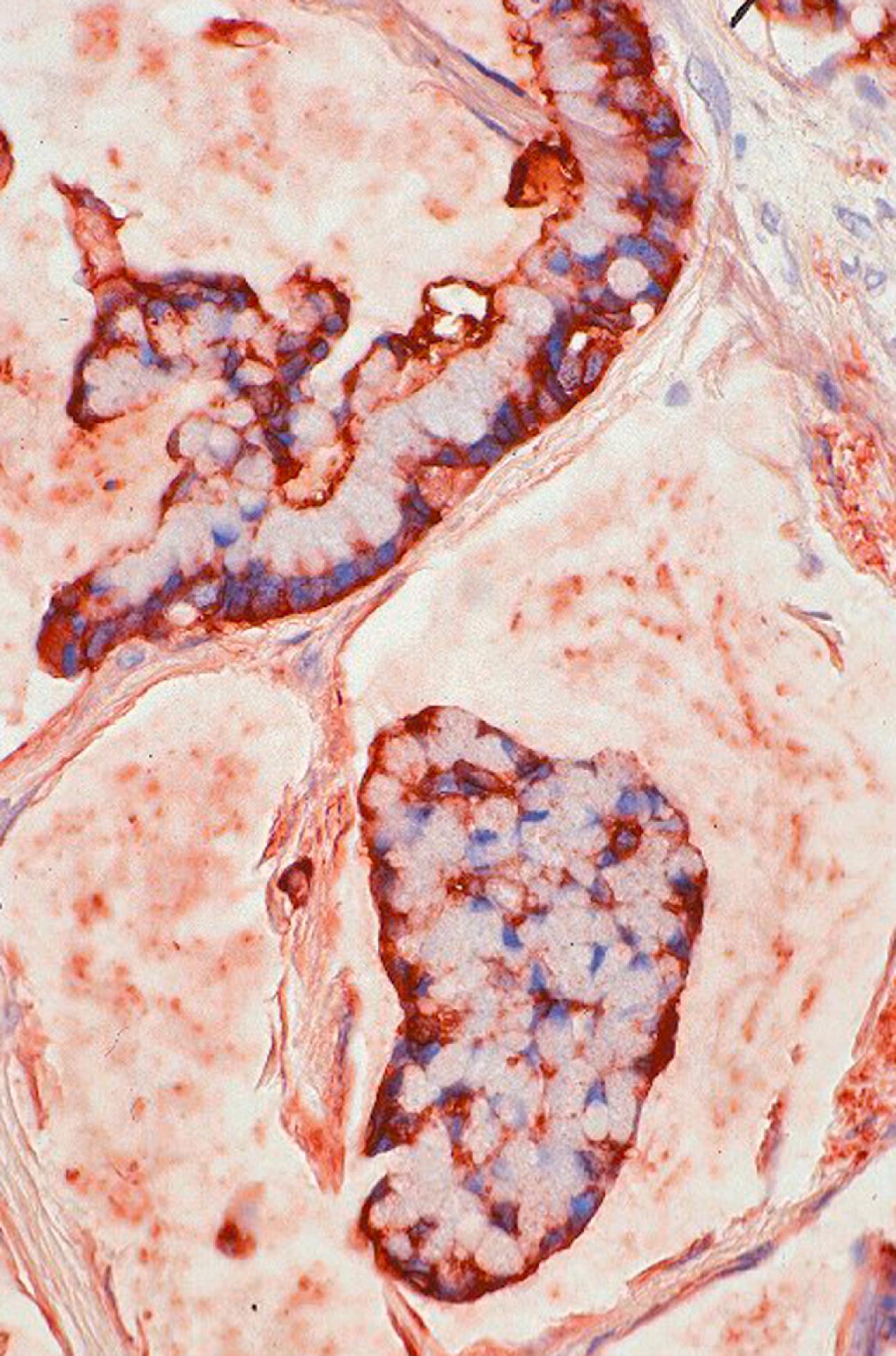
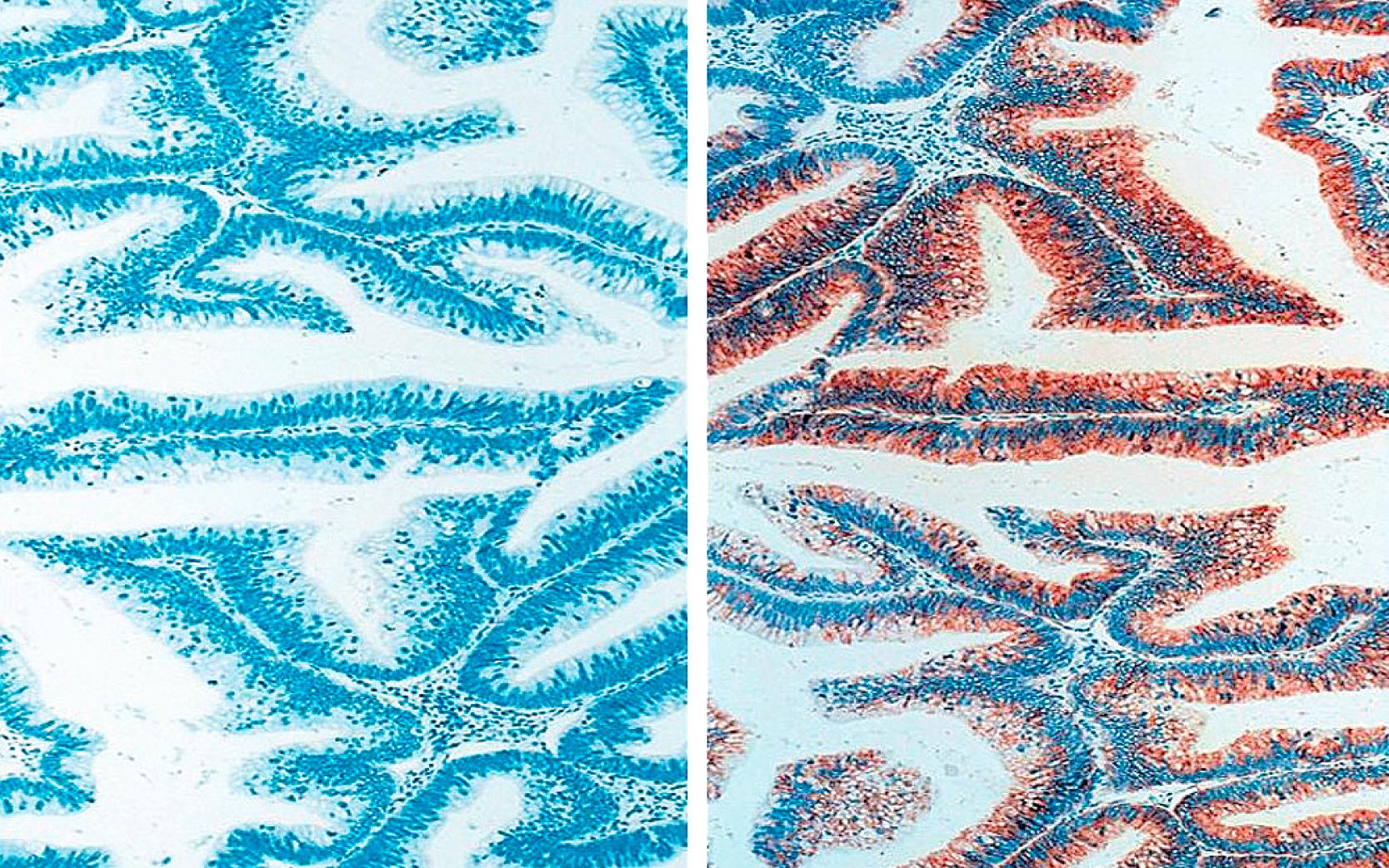
Immunohistochemically, in addition to the conventional epithelial and ductal markers, such as CKs, mCEA, CA19-9, and B72.3, colloid carcinoma is unique among invasive carcinomas of the pancreas by expression of intestinal differentiation markers, MUC2 and CDX2 ( Figs. 15.9 and 15.10 , respectively). Also, in contrast with DAs, they are negative for MUC1. Furthermore, the pattern of accentuated mCEA labeling in the stroma-facing surface of the cells ( Fig. 15.11 ) is specific to colloid carcinomas and is seldom seen in other invasive carcinomas of the pancreas. As opposed to DAs, the expression of DPC4 is intact in almost all cases.
Only one-third of the colloid carcinomas harbor KRAS oncogene mutations. Recent studies identifying mutations in GNAS in the vast majority of the colloid carcinomas also suggest that their carcinogenesis is distinct from that of DAs. , ,
There is a spectrum of intraductal proliferative lesions that are presumed to be precursors of invasive carcinomas, referred to as pancreatic intraepithelial neoplasia (PanIN). This spectrum used to be graded on a three-tiered scale as PanIN 1A (the earliest step), progressing to 1B and 2, and finally to PanIN3, which is considered carcinoma in situ. However, this is now revised into a two-tiered classification scheme, which was felt to be more in line with practical consequences: low-grade and intermediate-grade dysplasia likely has no immediate clinical consequences, whereas high-grade dysplasia usually requires clinical attention. According to this new two-tiered grading system, intermediate-grade is now categorized as low grade, and high grade is used only for the most advanced dysplastic lesions. Low-grade PanIN is a relatively frequent incidental finding. However high-grade PanIN is very seldom encountered in isolation, without a concomitant invasive adenocarcinoma.
The immunohistochemical labeling pattern of PanINs parallels that of DA. None of the lesions express MUC2, but most express MUC1, MUC4, MUC5AC, and MUC6. , In the multistep progression of DA, MUC1 expression within normal intra- and interlobular ducts appear to be decreased in the low-grade PanINs and are subsequently re-expressed in the high-grade PanINs. Unlike the case with MUC1, MUC5AC is expressed relatively uniformly throughout both grades of PanIN. Increasing Ki-67 labeling indices has been shown with increasing grades of “dysplasia” in PanINs.
Most of the molecular abnormalities identified within DAs have also been detected within PanIN. Among these, KRAS , p16/CDKN2A , GNAS , and BRAF seem to be “early” events. Their frequency increases with increasing grades of dysplasia and precedes both p53 mutation and DPC4 inactivation. , p53 mutation, as assessed by nuclear over-expression of p53 protein (>25% nuclei), is a “late” event in the progression model of DA, occurring only in high-grade PanIN (57% of the lesions). Similar to the case of the p53 gene, inactivation of the DPC4 gene appears to be a “late” event, seen only in high-grade PanIN (28% of the lesions).
IPMNs are characterized by intraductal proliferation of neoplastic mucinous cells, which usually form papillae and lead to cystic dilatation of the pancreatic ducts, forming clinically and macroscopically detectable masses. Microscopically, papillae with three distinct morphologic patterns can be seen: (1) a pattern reminiscent of gastric foveolar epithelium or resembling low-grade PanIN with scattered goblet cells (gastric) ; (2) a pattern closely resembling colonic villous adenomas (intestinal) ; (3) a pattern characterized with more complex papillae lined by cuboidal cells (pancreatobiliary) . Oncocytic intraductal neoplasms are now regarded as a distinct category. , , ,
There is a spectrum of cytoarchitectural atypia (IPMN with low-grade dysplasia to IPMN with high-grade dysplasia), , and approximately 30% of resected IPMNs have an associated invasive carcinoma. Intestinal type IPMNs are usually associated with colloid carcinoma; gastric and pancreatobiliary types are associated with tubular type invasion with all the morphologic features of DA. Ki-67 labeling demonstrates a progressive increase in cell proliferation from normal duct epithelium, to IPMN with low-grade dysplasia to IPMN with high-grade dysplasia. ,
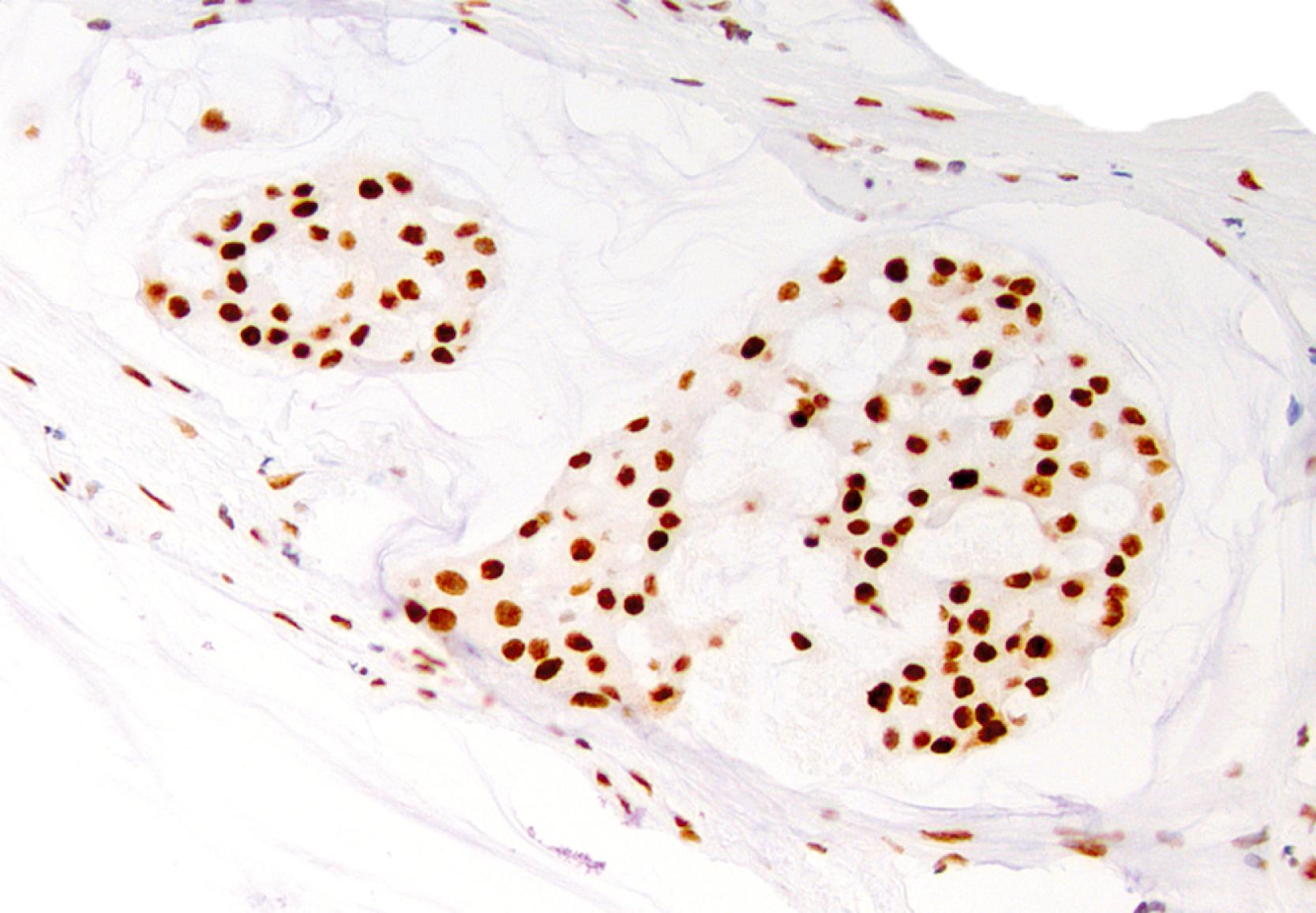
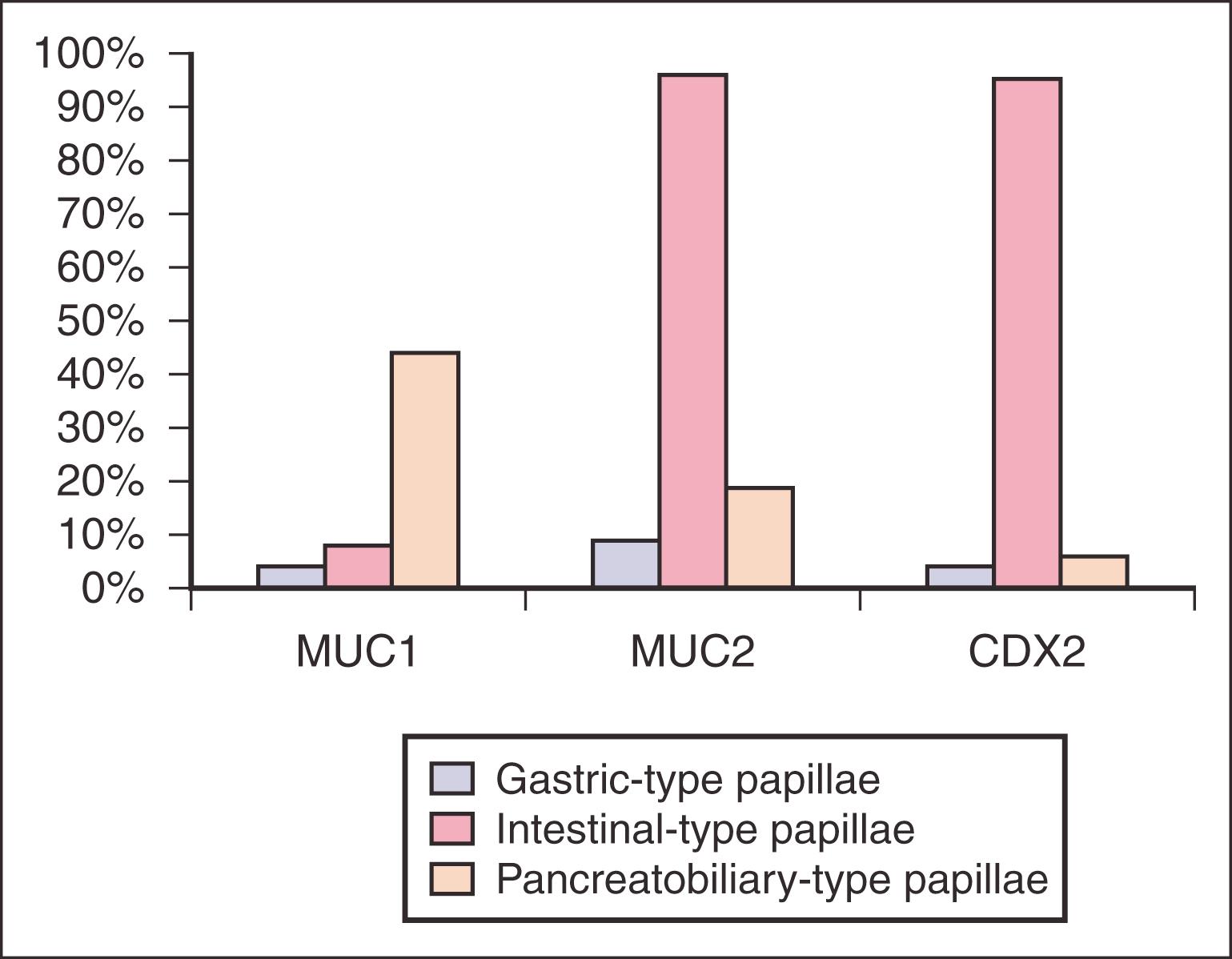
MUC expression profile of IPMNs ( Fig. 15.12 ) have been instrumental in delineating the differentiation and lineage of these neoplasia and in recognizing its subsets that are clinically significant. , , , , (1) Gastric type papillae appear to be a full recapitulation of gastric mucosa, with more papillary areas expressing MUC5AC and only small glandular elements at the base labeling with MUC6. They are usually negative or only focally positive for MUC1 and CDX2. Scattered goblet cells can be highlighted by MUC2 ( Fig. 15.13 ). , , , , (2) Intestinal type papillae do, in fact, show molecular characteristics of intestinal differentiation as evidenced by diffuse MUC2 and CDX2 expression but not MUC1 ( Fig. 15.14 ). , , , , Invasive carcinoma associated with the intestinal type, which is typically colloid carcinoma, also expresses MUC2 and CDX2 but not MUC1. In addition, intestinal type papillae are positive for MUC5AC and negative for MUC6. , , , , (3) Pancreatobiliary type papillae typically do not express MUC2 and CDX2, but may instead express MUC1 (a “marker” of aggressive phenotype in the pancreas), as well as MUC5AC, and to a lesser degree, MUC6. , The invasive component also expresses MUC1 but not MUC2. (In general, IPMNs are reported to show weaker labeling for MUC4 (70%), MUC3 (60%), and MUC5B (35%) and almost always negative for MUC7.
As expected, virtually all IPMNs express CKs. They are positive for CAM 5.2, AE1/AE3, CKs 7, 8, 18, 19, and variably for CK20. , , Some IPMNs, especially intestinal type ones, also express CA19-9 and mCEA. , , In the intestinal type, the degree of mCEA expression increases with the degree of dysplasia. Twenty percent of IPMNs label for DUPAN-2. , , Scattered neuroendocrine cells that are positive with chromogranin and synaptophysin are seen in most tumors but account for less than 5% of the tumor cells. , Cyclooxygenase-2 is also expressed in 60% to 80% of IPMNs.
KRAS oncogene mutations have been reported in 30% to 60% of IPMNs. , , , Recently, it has also been shown that recurrent mutations at codon 201 of GNAS are also present in approximately two-thirds of IPMNs, and that either KRAS or GNAS mutations could be identified in approximately 95%, , , illustrating that molecular analyses are a highly sensitive assay for the identification of IPMNs. However, it has been shown that oncocytic type IPMNs typically lack KRAS2 and GNAS mutations , , in stark contrast with any other tumor types in the pancreas characterized by ductal-mucinous differentiation, including greater than 90% of invasive ductal carcinomas. These findings elucidate that oncocytic type IPMN is not only morphologically distinct but also genetically distinct from other IPMN subtypes.
Of note, the frequency of TP53 , , , , and p16/CDKN2A tumor suppressor gene mutations in IPMNs vary greatly between reported series. , , , However, in contrast to DAs, the protein product of the SMAD4/DPC4 tumor suppressor gene is retained virtually in all cases, including the invasive carcinomas, suggesting a substantial difference in the pathogenesis of these two neoplasms. , , , , , , Recently, human cripto-1 protein, which is thought to have a role in tumor progression, was reported to be expressed more abundantly in the pancreatobiliary type than in the other types.
Although intraductal oncocytic papillary neoplasm (IOPN) of the pancreas was first described as a distinct entity, since both IOPN and IPMN present similarly as a cystic pancreatic lesion due to dilation of the native ducts by the intraductal neoplasm, the previous (2010) World Health Organization (WHO) guidelines put this neoplasm under the general category of IPMN as a variant thereof . However, more recent studies have illustrated differences between these entities, warranting revisions in the way these neoplasms are viewed and classified. , , , As such, in the current (2019) WHO, it is classified as a distinct entity.
On microscopy, the lesions exhibit papillary architecture with distinct oncocytic cytology and intraepithelial lumina. These intraepithelial lumina often contain mucin. Scattered goblet cells may be identified. Their papillae usually label for MUC1 , and MUC6, , whereas MUC2 and MUC5AC are largely restricted to goblet cells. , , CDX2 is rarely expressed. IOPNs also label strongly with antibodies against mitochondrial antigens. , , Interestingly, there is consistent immunolabeling with hepatocyte paraffin-1 (HepPar-1) antibodies; however, in situ hybridization (ISH) for albumin, a more specific test for hepatocellular differentiation, is consistently negative.
A detailed study we performed has shown that IOPN is not only morphologically distinct but also genetically distinct from other IPMN subtypes and pancreatic DA, as it does not harbor the vast majority of the previously reported IPMN- or pancreatic DA-related mutations. The most important genotypic difference from IPMN and pancreatic DA is the absence of KRAS and GNAS mutations in IOPNs. In contrast, ARHGAP26, ASXL1, EPHA8, and ERBB4 genes appear to be altered in some IOPNs.
Also, a subset of oncocytic pancreatic and biliary neoplasms reveal DNAJB1-PRKACA fusions, , which used to be regarded as diagnostic for fibrolamellar hepatocellular carcinoma. Considering DNAJB1-PRKACA fusions lead to upregulated protein kinase activity and that this upregulated protein kinase activity has a significant role in tumorigenesis, protein kinase inhibition could have therapeutic potential in the treatment of these pancreatobiliary neoplasms, once a suitable drug is developed.
Intraductal tubulopapillary neoplasm (ITPN) is a recently described entity. , It resembles IPMN by its intraductal nature and mimics ACC by its acinar pattern; however, it has several distinguishing characteristics: (1) no visible secreted mucin; (2) highly cellular complex intracellular tumor nodules showing predominantly tubular or cribriform patterns; (3) the absence of intracytoplasmic mucin; (4) atypical nuclei; (5) the absence of acinar and neuroendocrine differentiation; and (6) a relatively favorable overall outcome, despite an invasive carcinoma component in approximately two-thirds of the lesions. However, invasion is typically focal and difficult to distinguish from pagetoid spread to the smaller ductules. Nodular growth is characteristic both clinically and pathologically. Immunohistochemically, ITPNs are positive for AE1/AE3, CAM5.2 (100%), CK7 (100%), and CK19 (89%), but not for CK20 and CDX2 ( Fig. 15.15 ), , , and most express CA19.9 (93%) . Focal linear immunoreactivity for mCEA (50%) has been reported along the apical cytoplasm. The lesions also express MUC1 (88%) and MUC6 (68%), while MUC2 is negative, , , placing them closer to the pancreatobiliary type IPMNs. However, MUC5AC is almost always negative. The lesions show intact DPC4 labeling. Lack of acinar differentiation, as demonstrated by negative trypsin and other acinar markers, is essential in the differential diagnosis of intraductal tubular carcinomas from ACCs because the morphologic distinction of these two tumor types is often very challenging.
A detailed study we performed has shown that ITPN is genetically distinct from IPMN and pancreatic DA, as it does not harbor the vast majority of the previously reported IPMN- or pancreatic DA-related mutations. The most important genotypic difference from IPMN and pancreatic DA is the absence of KRAS and BRAF mutations in ITPNs. In contrast, certain chromatin remodeling genes ( MLL1 , MLL2 , MLL3 , and BAP1 ) and phosphatidylinositol 3-kinase (PI3K) pathway genes ( PIK3CA , PIK3CB , and PTEN ) appear to be mutated in at least a subset of ITPNs. Also, about 25% of ITPNs reveal either FGFR2 ( FGFR2-CEP55 , FGFR2-SASS6 , DISP1-FGFR2 , FGFR2-TXLNA , and FGFR2-VCL ) or ALK (STRN-ALK) fusions.
These findings provide support not only for the proposition that ITPN is a distinct pancreatic intraductal neoplasm with different morphologic features and biological behavior, but also for the hypothesis that distinct genetic pathways of tumor development. More important, some of these genetic alterations might be potentially targetable. For example, PIK3CA mutation is of special interest as it is a potential therapeutic target for inhibition of the PI3K pathway. , Similarly, BAP1 mutation may confer sensitivity to drugs targeting chromatin remodeling, such as histone deacetylase inhibitors. Also, several independent studies reported that cells harboring FGFR fusions show enhanced sensitivity to the FGFR inhibitors, suggesting that the presence of FGFR fusions may be a useful biomarker of tumor response to FGFR inhibitors. ,
Most other intraductal neoplasms have a fundamentally papillary architecture, allowing separation of IPMNs from ITPNs. Even if IPMNs have some limited tubular growth, especially at the periphery of the involved ducts, complete expansion and obliteration of the ductal profiles by a tubular proliferation is unusual. The presence of intracytoplasmic mucin and MUC5AC expression also favors IPMN.
Similarly, IOPNs can exhibit a solid or tubular growth pattern, but ITPNs lack the abundant granular eosinophilic cytoplasm of IOPNs.
ACCs may have an intraductal growth pattern either focally or extensively. Fortunately, IHC is very helpful. ACCs consistently express pancreatic enzymes, such as trypsin, chymotrypsin and generally lack expression of CK19. ITPNs consistently fail to express pancreatic enzymes.
Well-differentiated pancreatic neuroendocrine tumors (PanNETs) can also rarely show an intraductal growth pattern, but the characteristic diffuse staining for neuroendocrine markers can separate these from ITPNs.
In the last decade, MCNs began to be defined by the presence of ovarian type stroma. Studies applying this criteria more recently revealed that MCNs are seen almost invariably in perimenopausal women (95% of the patients are women; mean age, 50 year, there are only few men with ovarian stroma in record), and they present as a thick-walled cyst, often multilocular, in the tail of the pancreas. Microscopically the cysts are lined by mucin-producing epithelium, although nonmucinous pancreatobiliary epithelium is often seen and in some cases can predominate picture in paradox with the entity name mucinous. A distinctive ovarian-like stroma is present by definition, often forming a band around the cysts, and occurring in the septa of the cysts. , Just as in IPMNs, MCNs also exhibit characteristics of an adenoma-carcinoma sequence (MCNs with low-grade dysplasia and MCNs with high-grade dysplasia). , , Invasive carcinoma can be seen in association with MCN in less than one-fifth of MCNs. Invasive carcinoma is almost exclusively of tubular type, with all the morphologic features of DA. , , On occasion, sarcomatoid neoplasms arise in MCNs, but it is almost never of the colloid type.
The epithelial cells express immunoreactivity with CKs (CK7, 8, 18, and 19) , , , as well as with EMA, CA19-9, mCEA, DUPAN-2, and CA125. , , MUC1 is typically not expressed in non-invasive lesions of MCNs, but is a marker of invasion observed in greater than 90% of cases with invasion, detected both in the in situ and the invasive components. , MUC2 and CDX2 positivity can be seen as a very focal finding, especially in the interspersed goblet cells or sometimes at the base of the epithelium; however, in contrast with villous/intestinal type IPMNs, the papillary dysplastic nodules are typically negative or only focal for these markers. , The lesions invariably express MUC5AC, which is also commonly expressed in IPMNs and DAs. , Although the papillary components of MCN are mostly MUC6 negative, the foveolar-like epithelium in nonpapillary areas are typically positive for MUC6. Chromogranin or synaptophysin positive scattered neuroendocrine cells are frequently noted within the epithelium. , ,
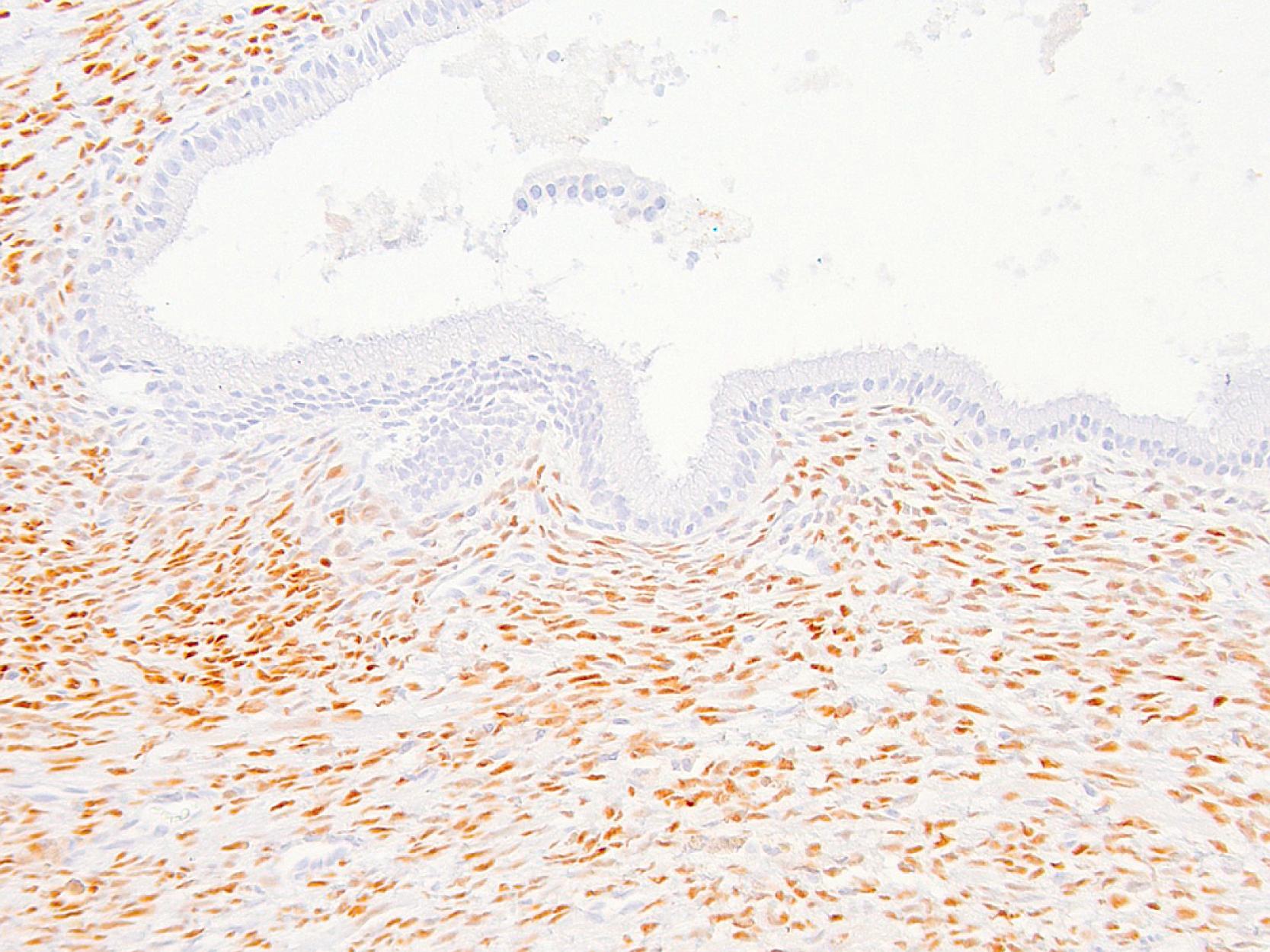
The ovarian-type stroma is immunoreactive for vimentin, smooth muscle actin, muscle-specific actin, desmin, h-caldesmon, bcl-2, and CD99 usually in a patchy distribution. , , Progesterone receptors are also expressed fairly consistently ( Fig. 15.16 ) and, in subtle cases, may help to establish the diagnosis by highlighting the presence of this pathognomonic finding. Estrogen receptors are often negative with the current antibodies available; however, it is suspected that this lack of detection is related to the receptor subunit specificities of these antibodies. If present, the luteinized cells label with antibodies to tyrosine hydroxylase, α-inhibin, and calretinin, which have been shown to recognize ovarian hilar cells and testicular Leydig cells. ,
By molecular/genetic analysis, KRAS mutations appear early and increase in frequency proportional to the degree of dysplasia. , p53 over-expression appears to occur relatively late in in situ and invasive mucinous cystadenocarcinomas. , Approximately half of the associated invasive carcinomas also show loss of DPC4 expression, which is not surprising because most of these carcinomas are conventional DAs. , , ,
MCNs are mucinous/ductal type neoplasia, and thus the epithelial cells are positive for CKs as well as for EMA, CA19-9, and mCEA. The epithelium may be nonmucinous.
All MCNs express MUC5AC, but MUC1 is seen predominantly in the in-situ papillary and invasive carcinoma areas.
The ovarian-type stroma cells label with antibodies to smooth muscle actin, muscle-specific actin, desmin, h-caldesmon, and also variably for α-inhibin and calretinin.
Progesterone receptors are expressed in the ovarian-type stroma cells and may be used to confirm the diagnosis in equivocal cases of MCNs.
Serous cystadenoma (SCA) is the only nonmucinous example of ductal neoplasia in the pancreas and, unlike other ductal tumors, has virtually no tendency for malignant transformation. It is also known to have well-established association with von Hippel-Lindau (vHL) syndrome. ,
The tumor cells have a clear cytoplasm because of the abundant intracytoplasmic glycogen and label with CAM 5.2, AE1/AE3, CK7, CK8, CK18, and CK19, but usually not with CK20. , One-third of the cases are also positive for EMA. , , , Even though CA19-9 and B72.3 expression , is reported, immunolabeling for mucin markers is generally lacking with the exception of MUC6. mCEA is uniformly negative, as are insulin, glucagon, somatostatin, vasoactive intestinal polypeptide, and vimentin. Chromogranin or synaptophysin positive scattered neuroendocrine cells are commonly detected. , , , , , , ,
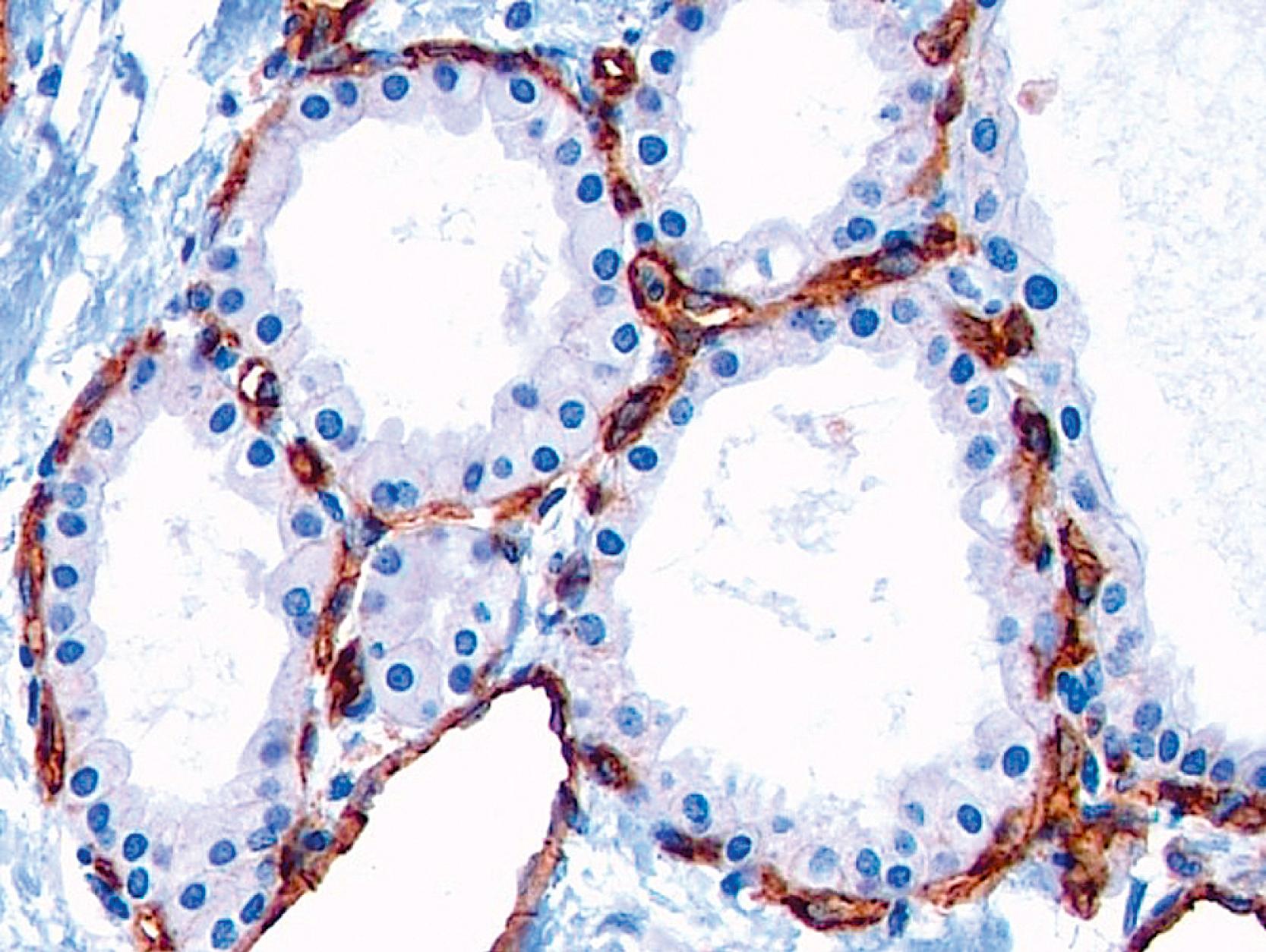
Not surprisingly, molecules implicated in clear-cell tumorigenesis (carbonic anhydrase IX, glucose uptake and transporter-1 [GLUT-1; Fig. 15.17 ], hypoxia-inducible factor-1α [HIF-1α] and vascular endothelial growth factor [VEGF]) are also consistently expressed. , One study had found that vascular endothelial growth factor-A (VEGF-A) was markedly elevated in SCAs compared to other cysts ; however, this impression has not been verified. Also, similar to other vHL-related clear-cell tumors, there is a prominent capillary network immediately adjacent to the epithelium, confirming that the clear cell-angiogenesis association is also valid for this tumor type. This rich capillary network, which can be highlighted by CD31 stain ( Fig. 15.18 ), may be helpful for surgical pathologists, especially as needle biopsies are becoming the norm for the initial workup of the patients. This finding may also be helpful in frozen sections where clear-cell cytology is typically not evident due to the preservation of glycogen.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here