Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Disclosure : The authors have no financial interest to declare in relation to the drugs, devices, and products mentioned in this article.
There continues to be a steady annual growth in breast reconstruction within the United States, with over 100 000 procedures performed in 2016 and a 39% increase in reconstructive breast procedures since the year 2000.
Immediate two-stage prosthetic breast reconstruction is well accepted in breast cancer reconstruction due to its impact on post-mastectomy body image and quality of life, as well as its safety and high patient satisfaction. Furthermore, in 2010, a national survey found half of all US-based plastic surgeons who perform implant-based breast reconstruction use acellular dermal matrix (ADM). As prosthetic breast reconstructions continue to increase, all plastic surgeons should be well versed in delivering a safe, consistent, and aesthetically pleasing result in this kind of reconstruction.
In the following chapter, the authors will focus on tissue expander–based immediate breast reconstruction with acellular dermal matrix as a first-stage implant-based breast reconstruction. Emphasis will be placed on surgical technique, as well as highlighting key concepts and pearls in tissue expander/ADM-based reconstruction.
Treatment planning for post-mastectomy breast reconstruction depends on several issues. Key indications for immediate breast reconstruction include the patient's oncologic disease burden as well as the need for adjuvant therapy. Immediate two-stage implant-based reconstruction is optimal in cases where adjuvant radiation therapy is not required. Ideal candidates include relatively thin patients and patients requiring bilateral reconstruction ( Fig. 10.1 ). However, the success and outcome of immediate implant-based reconstruction depends heavily on a reliable native soft tissue envelope. This can be achieved through a collaborative effort between the surgical oncologist and reconstructive surgeon. The two-stage approach also allows for precise recreation of the breast mound in terms of Infra-mammary fold (IMF) positioning, natural shape and final symmetry and is more flexible than one-stage implant-based reconstruction with fewer complications.

One absolute contraindication is ischemic or damaged mastectomy skin flaps. In this case a delayed reconstruction may be in the patient's best interest. Other contraindications include poor quality of the pectoralis major muscle, obesity, and tobacco use.
Acellular dermal matrices have become ubiquitous in breast reconstruction. The benefits of ADM include improved inframammary fold control, better support and control of the pocket, greater intraoperative expansion with fewer subsequent clinic visits, and decreased risk of capsular contracture. There is also evidence to suggest a clinical benefit for patients who undergo subsequent radiation therapy, but the literature remains inconclusive and will benefit from further studies.
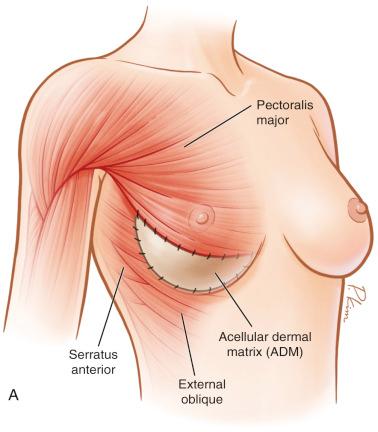
Additionally, by utilizing ADM as a tissue supplement over the inferior pole, further muscle dissection is spared, which leads to less postoperative pain, and a more anatomically precise pocket can be defined ( Fig. 10.2 ). The higherintra operative fill volume also addresses the retained skin in skin-sparing mastectomies. These benefits ultimately result in increased control by the surgeon over the reconstruction as well as final aesthetic outcome for the patient.
During the preoperative visit, the overall quality of breast skin in each patient should be evaluated carefully. In addition, the presence of breast ptosis should also be evaluated. One important discussion to highlight in the preoperative setting with the surgical oncologist is mastectomy flap thickness. It is imperative to adhere to good oncologic principles during the ablation. However, it must be emphasized that immediate prosthesis-based reconstruction relies on healthy and viable tissue flaps, which are to be respected in order to optimize the reconstructive outcome.
Skin-sparing or nipple-sparing mastectomy can usually be decided by the breast surgeon. The patient should be informed of the possibility of delayed reconstruction if the plastic surgeon deems the flaps are compromised. Additional considerations involve the impact of possible adjuvant chemotherapy and radiation therapy.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here