Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Spinal cord tumors are uncommon causes of back pain, radicular pain, and sensorimotor deficits in adults and pediatric patients. Primary spinal tumors are less common than intracranial tumors and represent approximately 2–4% of primary central nervous system (CNS) tumors.
Spinal cord tumors are classified as either (1) intradural intramedullary, (2) intradural extramedullary, or (3) extradural depending on the relationship to the spinal cord and dura.
Extradural tumors . The majority of spinal tumors are extradural, accounting for 60% of spinal cord tumors and are frequently compressive osseous metastatic lesions. Intradural spine tumors can originate adjacent to the spinal cord (e.g., extramedullary) or within the cord (e.g., intramedullary). The differential diagnosis can be narrowed by recognizing where the tumor is located relative to the thecal sac and spinal cord.
Intramedullary tumors . Intradural intramedullary spinal cord tumors (IMSCTs) comprise 8–10% of primary spinal cord tumors, of which 60–70% are ependymomas and 30–40% are astrocytomas. The third most common IMSCT is hemangioblastoma, which represents 3–8% of all IMSCT. Hemangioblastomas are associated with von Hippel-Lindau (VHL) syndrome in 15–25% of cases. The clinical presentation of primary spinal cord tumors depends on the location of the lesion. In a recent series of IMSCTs, pain was the most common presenting symptom (72%) and can manifest as back pain (27%), radicular pain (25%), or central pain (20%). Motor disturbance was next most common (55%), followed by sensory problems (39%).
Intradural extramedullary tumors . Intradural extramedullary spinal tumors are usually benign lesions with a few exceptions and can be cured with preserved neurologic function with surgery alone in the majority of cases. Intradural extramedullary tumors comprise more than 70% of intradural spinal cord tumors in adults and are only slightly less common in pediatric patients. The most common intradural extramedullary tumors are derived from nerve sheath cells (schwannomas and neurofibromas) or meningeal cells (meningiomas). Myxopapillary ependymoma is an extramedullary lesion arising from the conus medullaris and filum terminalis. Other rare extramedullary tumors include hemangiopericytomas, paragangliomas, malignant peripheral nerve sheath tumors, epidermoid cysts, and dermoid cysts.
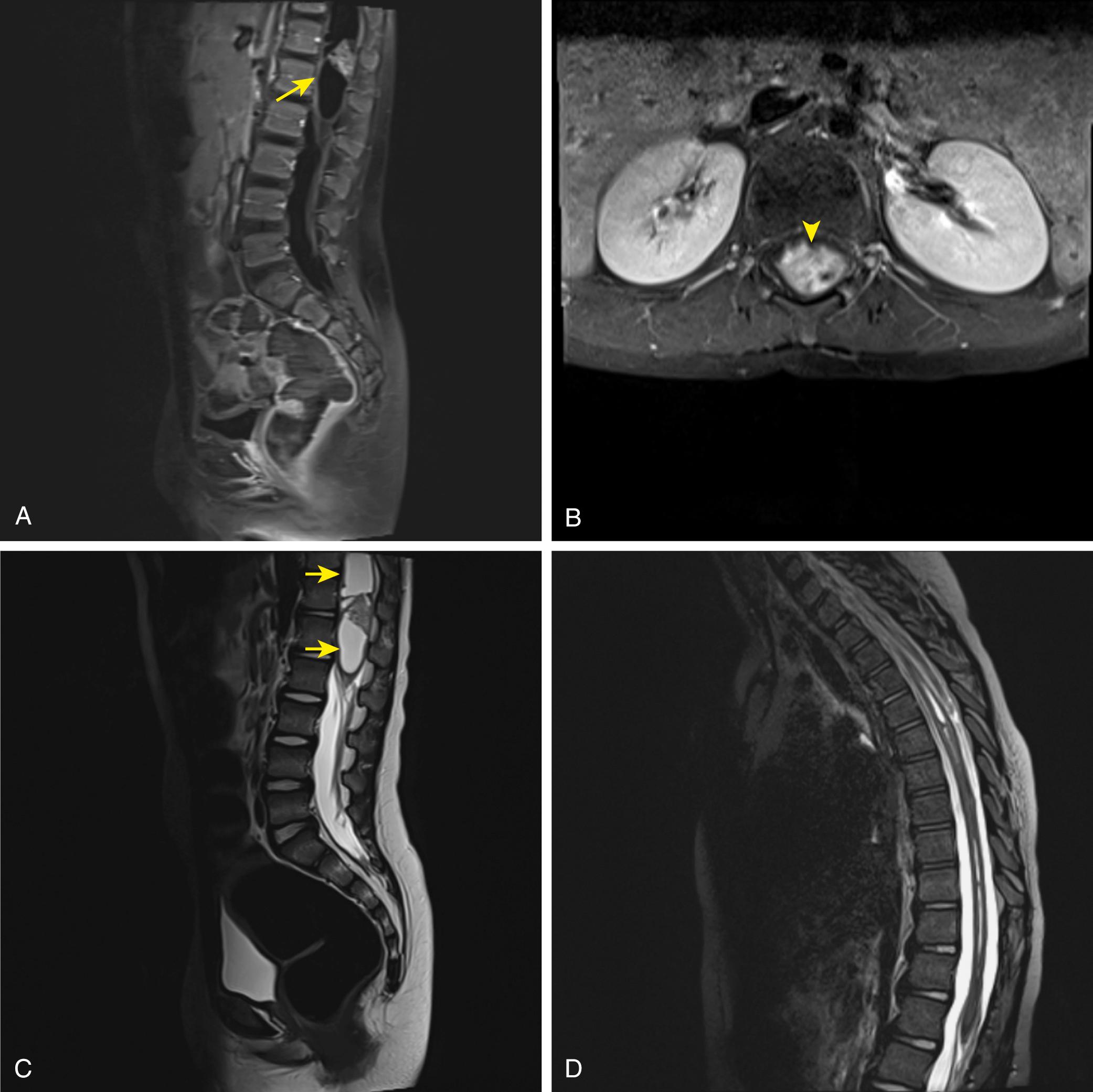
Case . A 5-year-old boy presented to the pediatric orthopedic clinic with complaints of worsening back pain and scoliosis. He had been previously evaluated for his scoliosis with a plan to conservatively manage and observe clinical symptoms. Due to the progressive nature of his complaints, an MRI of the thoracic and lumbar spine were obtained, which demonstrated a 21-mm enhancing intramedullary lesion with a distal cystic component at the thoracolumbar region of the spinal cord with an associated syrinx proximally ( Fig. 8.1 ). On examination, he maintained a kyphotic posture due to pain and had dysesthesias throughout his bilateral lower extremities but no appreciable strength deficits. Reflexes in the lower extremities were symmetrically absent. Surgical resection was recommended, and the patient underwent laminectomy and gross total resection of the tumor. The surgery and his postoperative course were uneventful, and he was discharged to a rehabilitation facility 1 week later. Final pathology was consistent with a pilocytic astrocytoma. His follow-up imaging demonstrated complete tumor removal without residual enhancement and improvement in his syrinx. He continues to do well without functional imitations on serial follow-up.
Teaching Points: Imaging of Spinal Cord Astrocytoma. Astrocytomas account for 80–90% of IMSCT in childhood and approximately 60% in adolescence. The peak incidence of astrocytomas is in the third decade of life, but they are not as common as intramedullary ependymomas in this age group. In adults, astrocytomas make up almost 25% of IMSCT with equal incidence in men and women. Intramedullary astrocytomas are predominantly located in the cervicothoracic or thoracic region in pediatric patients, but cervical involvement is more common in the adult population. , Astrocytomas can span multiple vertebral levels and can have associated cyst formation. , Low-grade astrocytomas and fibrillary astrocytomas account for almost two-thirds of intramedullary astrocytomas in adults and almost 90% of intramedullary astrocytomas in children. High-grade lesions are rarer and account for about 10% of intramedullary astrocytomas.
Imaging and histology. MRI of low-grade spinal astrocytomas reveals an enlarged homogeneous mass with hypointense to isointense signal on T1-weighted images and hyperintense signal on T2-weighted images. There is very little edema and no hemorrhage in low-grade astrocytomas. Most intramedullary astrocytomas enhance, and calcifications are rare. While pilocytic astrocytomas can have well-defined borders, fibrillary astrocytomas are poorly defined with irregular tumor margins. High-grade anaplastic astrocytoma or glioblastoma account for only about 10% of intramedullary astrocytomas. These higher grade lesions display heterogeneous enhancement associated with necrosis, edema, and cyst formation. Microscopically, low-grade astrocytomas show a low degree of cellularity, low mitotic activity, and absence of necrosis and microvascular proliferation. Anaplastic astrocytoma and glioblastoma show moderate to high cellularity and an increased mitotic index. Glioblastoma specifically exhibits a high degree of necrosis and microvascular proliferation.
Clinical features. Presentation of intramedullary spinal cord astrocytoma is variable and typically progresses over months to years. Pain is the earliest and most frequent presenting complaint and can be local or radicular. Sensory disturbance is also common and may consist of dysesthesias or loss of sensation unilaterally or bilaterally. Spasticity and weakness follow with loss of bowel and bladder function occurring late with the exception of tumors involving the conus medullaris. , Due to the centrally located nature of the tumor, motor deficits present with weakness in the upper extremities preceding the lower extremity. In children, pain is the most common first symptom, but gait deterioration, motor regression, torticollis, and kyphoscoliosis are also significant presenting findings. In malignant tumors, pain is followed by rapid neurological deterioration resulting in significant disability in 3 to 5 months. ,
Patient management . Treatment is directed at total surgical resection, particularly for low-grade gliomas. There is no evidence that the degree of resection affects outcome in high-grade gliomas, and the goal of surgery for these patients should be a less extensive resection in order to reduce postsurgical morbidity.
Electrophysiologic monitoring is frequently used intraoperatively during the resection of IMSCT with motor-evoked and somatosensory-evoked potentials being the most common modalities. Gross total resection is achievable with pilocytic astrocytomas due to its well-circumscribed nature. However, the infiltrative nature of even low-grade astrocytomas make gross total resection difficult without risking postoperative morbidity. The rate of gross total resection is reported to be between 30% and 70%. , ,
Subtotal resection of fibrillary astrocytomas is appropriate in many cases, and there does not seem to be any significant difference in survival between total and subtotal resection techniques in long-term survival when controlled for tumor grades. Intramedullary fibrillary astrocytomas have a high recurrence rate that ranges from 25% in low-grade tumors to almost 100% in high-grade tumors. , Adjuvant radiotherapy at diagnosis of high-grade astrocytoma or with tumor recurrence is frequently utilized. The utility of concomitant chemotherapy is uncertain due to systemic toxicity and inability of large molecules to bypass the blood-spinal cord barrier. In low-grade astrocytomas, 5-year survival ranges from 80–100%. Patients with intramedullary anaplastic astrocytomas or glioblastoma have an average life expectancy of 15 months. ,
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here