Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
An increasing number of injuries are being seen in young, skeletally immature patients, which may be due to a decrease in free play combined with an increase in participation in competitive organized sports, sport specialization, and a general lack of physical preparedness. In this population, unique injuries are encountered related to the presence of an open growth plate, which is often the “weak link” between tendon and bone. An injury may be related to a single acute event or to overuse, with approximately 50% of all injuries seen in pediatric sports medicine practices being attributed to overuse.
Single acute traumatic events consist primarily of fractures through bone, dislocation with ligamentous injury, avulsion fractures, or a combination of these processes. Overuse injuries primarily relate to chronic stress of the growth plates, fatigue-type stress fractures of bone, and less commonly tendinosis.
An evaluation of sports injuries in young children versus adolescents found that children 5 to 12 years of age most often had acute traumatic bony injuries to the upper extremity, whereas overuse injuries to bone, such as apophysitis and osteochondritis dissecans, predominated in the lower extremities. Patients 13 to 17 years of age were more likely to have soft tissue than bony injuries, including anterior cruciate ligament injuries and meniscal tears.
This chapter emphasizes common conditions encountered in the course of imaging the skeletally immature athlete. A brief review of the pathophysiology common to many injuries seen in this group of patients is followed by a region-based review of specific conditions in this population.
The weakest part of the developing skeleton is the cartilage at the growth plates of the epiphyses and apophyses, with ligamentous structures shown to be two to five times stronger that open growth plates. Compared with adults, in whom acute tensile forces most commonly result in injury to the myotendinous junction, injury in skeletally immature patients most commonly occurs at or near osteochondral interfaces. It is because of the relatively weak cartilage present at the growth plates of apophyseal sites that avulsion fractures are more common in skeletally immature patients. When the tensile force overcomes the resistance of the cartilage at the growth plate, an acute avulsion fracture will occur.
Chronic repetitive stress, on the other hand, can lead to abnormal widening of the growth plates and may be seen clinically with pain or growth disturbance. Different mechanisms may exist depending on whether the applied stress is a repetitive compressive force or a traction force.
Pathophysiologically, the newly formed bone adjacent to the growth plates within the metaphyses is relatively fragile, with poor resistance to the compressive forces that can occur with repetitive weight-bearing stress in sporting activities. This repetitive microtrauma can disrupt the metaphyseal blood supply, thus limiting the delivery of necessary nutrients—such as calcium, vitamin D, and phosphates—that are needed for osteogenesis in endochondral ossification. Consequently, long columns of hypertrophic cartilage cells from the physis extend into the metaphysis. It is this extension of unmineralized cartilage that results in the characteristic widening of the growth plates in conditions such as gymnast's wrist. With traction forces, a chronic repetitive musculotendinous pull at the apophyseal site can outpace the ability of the body to repair the injury, resulting in the proliferation or hypertrophy of chondrocytes, microfractures, and inflammatory cells that has been termed apophysitis . This manifests as apparent physeal widening and a pattern of adjacent bone marrow and muscle edema on magnetic resonance imaging (MRI).
When repetitive stress is applied to bone, it responds by increasing the rate of cortical resorption and remodeling of the haversion system, ultimately leading to weakened cortical bone. When the rate of osteoclastic activity outpaces the rate of osteoblastic activity and persistent stress is applied through the weakened bone, fracture may occur.
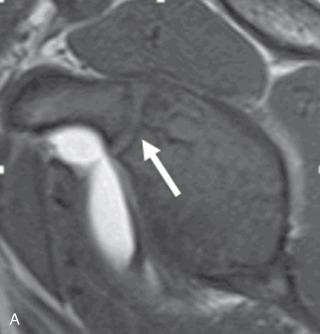
The proximal humeral growth plate begins to close at around 14 years of age, starting centrally, and concluding posterolaterally at around 17 years. Additional growth plates are present at the scapula, related to secondary ossification centers. These are important because they can be confused for fractures and can act as a point of weakness through which fractures may occur. The subcoracoid secondary ossification center forms within the superior glenoid with a bipolar growth plate present anteriorly at the base of the coracoid and posteriorly at the scapula. This ossification center contributes to growth of the superior third of the glenoid and starts to ossify between 8 and 10 years of age, completing typically by 16 to 17 years. The inferior glenoid secondary ossification center forms from multiple centers, resulting in a horseshoe-shaped epiphysis at the lower two-thirds of the glenoid that typically appears around 14 to 15 years of age and closes by 17 to 18 years ( Fig. 132.1A and B ).
At the clavicle, the medial cartilaginous epiphysis begins to ossify at 18 years of age, closing between 22 and 25 years. The lateral end of the clavicle can also have a secondary ossification center, but much less consistently. When present, it was thought to develop around 19 to 20 years of age and then to close quickly within a few months. However, more recent evidence based on a study using MRI identified this secondary ossification center in patients between 11 and 15 years of age. Owing to the rarity of this finding, its presence could result in an erroneous diagnosis of fracture.
The acromion forms from multiple ossification centers and is traditionally reported to reach complete closure between 18 and 25 years of age. However, the same MRI study also found that secondary ossification centers within the acromion can begin to ossify as early as 10 years of age and often close by 16 years. This is clinically relevant because it means that a symptomatic os acromiale may be seen in adolescent patients and is not only an adult problem.
Acute injuries are typically found in contact sports such as football, hockey, and wrestling, although other high-velocity sports such as snow and water skiing can result in fractures due to direct impact when falls occur.
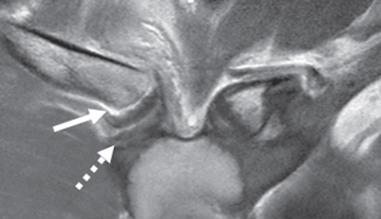
Midshaft clavicular fractures can occur in all age groups; however, a fracture unique to the immature skeleton that is typically seen in patients less than 13 years of age is the distal clavicular periosteal sleeve fracture. This fracture can mimic an acromioclavicular joint injury owing to displacement of the clavicle, although characteristically the acromioclavicular and coracoclavicular ligaments are intact. Fracture may occur either through the distal clavicular physis and be radiographically occult or may occur through the metaphysis and be visible on radiographs. Either way, subsequent stripping of the periosteal sleeve occurs, which often results in clavicular elevation and apparent disruption of the coracoclavicular ligaments, which are in fact uninjured and still attached to the periosteum ( Fig. 132.2 ). Unlike some grade 3 acromioclavicular joint injuries, these injuries are typically treated conservatively, with eventual ossification seen along the stripped periosteum. Similarly, injuries to the medial clavicle in the skeletally immature patient are more likely to represent a Salter 1 or 2 fracture than true dislocation, which may have an impact on treatment ( Fig. 132.3 ).

Another unique fracture to the skeletally immature athlete is a fracture through the base of the coracoid, which typically involves the growth plate at the base of the coracoid ( Fig. 132.4A and B ). Salter-Harris 2 fractures and greater tuberosity avulsion fractures are other fractures that also may occasionally be encountered ( Fig. 132.5 ).

Acute injuries can also affect the soft tissue constraints of the shoulder. The glenohumeral joint is particularly prone to soft tissue injury due to its large range of motion (ROM) and the glenohumeral articulation, which provides negligible osseous stability, relying almost entirely on static and dynamic soft tissue stabilizers. It is not a surprise then, that shoulder dislocations may be seen in young athletes participating in contact sports. In addition to labral and capsuloligamentous injuries, shoulder dislocations can result in osseous fractures to the glenoid and humerus, known as Bankart and Hill-Sachs lesions, respectively, although in younger patients, care should be taken not to call the normal inferior glenoid ossification centers a fracture (see Fig. 132.1 ). Rotator cuff tears can also uncommonly be seen in young athletes following a single traumatic event; when present, they are often also associated with labral injury. Although these injuries may be seen in skeletally immature patients, they are not typical for this population.
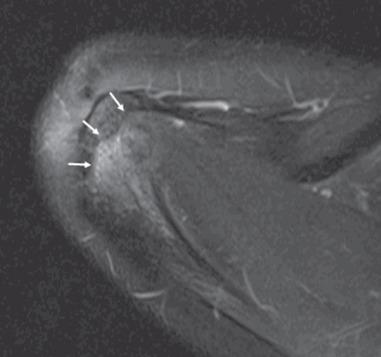
The quintessential overuse injury of the shoulder in the skeletally immature athlete is referred to as “Little Leaguer shoulder,” which is not a Salter 1 fracture but rather a chronic stress injury to the growth plate, which, as discussed previously, disrupts normal endochondral ossification and results in widening and irregularity of the growth plate on radiographs ( Fig. 132.6A–C ). The posterolateral growth plate in the proximal humerus is last to close and should not be confused with a chronic stress injury. If findings are equivocal, a contralateral view of the shoulder with the humerus in external rotation can be performed. Performance of a complete radiographic series for comparison purposes is unnecessary and exposes the patient to unnecessary radiation. On MRI, growth plate widening can be seen on the ubiquitous fat-suppressed fluid-sensitive sequences often performed when joints are being imaged, but they are particularly well visualized on non–fat-suppressed images.

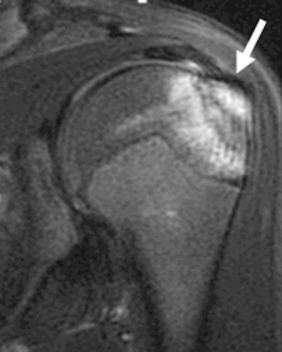
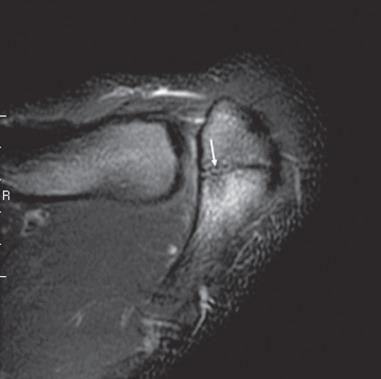
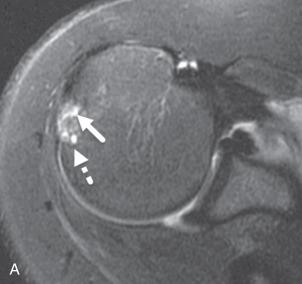
Another overuse injury that can be seen is the symptomatic os acromiale. Although an os acromiale has historically been considered to represent failure to incorporate the ossification centers of the acromion after 25 years of age, more recent literature has found that os acromiale can occur between 11 and 15 years, as discussed previously. Differentiation of normal acromial ossification centers from an os acromiale lies in evaluating the shape of the interface between the centers and the acromion; an arched shape is characteristic of a normal developmental ossification center, whereas a transverse interface perpendicular to the long axis of the acromion suggests os acromiale ( Fig. 132.7 ). When this finding is being evaluated on MRI, fluid at the interface and a surrounding marrow edema pattern present on fluid-sensitive sequences in the context of an os acromiale suggests instability and motion of the ossicle ( Fig. 132.8 ).
Glenohumeral instability—including anterior, posterior, or multidirectional instability—can occur related to the cumulative stress applied during sport activities such as baseball, football, tennis, swimming, or volleyball. Imaging findings related to overuse can be subtler than those related to a single traumatic event, and although labral pathology may be seen, MRI studies including MR arthrography can also be normal or show only a redundant capsule. Instability can also lead to pathologic internal impingement with subsequent labral or rotator cuff pathology, which is typically readily visible on MRI examinations, although these injuries are not unique to this population. However, it is important to remember that just the fact that a patient is young and has open growth plates does not mean that he or she cannot present with adult-type pathology. Indeed, a complete knowledge of adult pathology is also required when studies in skeletally immature patients are being interpreted ( Fig. 132.9 ).
A common mnemonic used to remember the normal pattern of development of the ossification centers of the distal elbow is CRITOE, which stands for Capitellum, Radial head, Internal (medial) epicondyle, Trochlea, Olecranon, and External (lateral) epicondyle. These ossification centers typically arise at 1, 5, 7, 10, and 11 years, respectively, with ossification centers in girls typically appearing 6 to 12 months earlier than those in boys. Absence of an ossification center at an age when it should already be seen should raise concern for a displaced avulsion fracture. If there is a question of whether the observed findings are pathologic or normal, imaging of the contralateral elbow may be useful.
Acute fractures about the elbow are commonly seen in young active children, two of the most common being supracondylar and lateral condylar fractures. Supracondylar fractures typically occur following a hyperextension mechanism after a fall on an outstretched hand, whereas lateral condylar fractures occur when a varus force is applied to an extended elbow with the forearm supinated. A common fracture seen in the older child athlete, typically 9 to 14 years of age, is an acute medial epicondyle avulsion fracture. This fracture accounts for approximately 20% of all pediatric elbow fractures and can be seen associated with overhead throwers due to the valgus stress applied with the throwing motion, but it can also be seen with falls on an outstretched hand ( Fig. 132.10 ). This fracture is also commonly associated with elbow dislocations, which may be seen in young athletes, particularly gymnasts. Careful assessment of the ossification centers is advised in the context of an elbow dislocation so as not to miss a displaced medial epicondyle into the humeroulnar joint.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here