Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The editors wish to thank authors Adda Grimberg and Jessica Katz Kutikov for their excellent contribution to this text in the fifth edition. This chapter has been reproduced here in the sixth edition essentially unchanged.
Enabled by its strategic anatomy, the hypothalamus uniquely serves the interface between the neural and endocrine systems. It is at the same time a part of the brain, an intrinsic component of neural pathways, and an endocrine gland, specially connected to the pituitary gland to form the “master gland” unit of the body. The multiple functions of the hypothalamus ultimately involve regulation of the body’s energy status and the maintenance of homeostasis, or bodily equilibrium. It has been long understood that, to refine this regulation, the hypothalamus responds both to information from the brain and to the levels of the peripheral hormones and body fluids it regulates. Appreciation has grown that the hypothalamus also receives input from the gut and fat stores, in essence closing the loop of metabolic regulation. All these incoming factors are compared with intrinsic setpoints, and outgoing messages are then released to enact modifications that will match the body to the appropriate setpoint. We have reviewed pediatric disorders of the neuroendocrine system, both congenital and acquired, elsewhere ; this chapter focuses on normal anatomy, embryology, and physiology of the hypothalamus.
Despite the importance of the hypothalamus for multiple homeostatic functions, the structure is less than 1% of human brain volume; its various parts total approximately 4 g of the 1200 to 1400 g of an adult human brain and measure less than 4 cm. Many of the borders of the hypothalamus are difficult to distinguish and are semiarbitrary, although magnetic resonance imaging techniques for study of the hypothalamus are improving. The hypothalamus lies at the base of the third ventricle, immediately posterior to the optic chiasm.
Because of its many eminences, the hypothalamus is an irregular structure that roughly forms a diamond. It is composed of four main structures: the tuber cinereum, the median eminence, the infundibulum, and the mammillary bodies. The tuber cinereum lies centrally on the inferior aspect of the hypothalamus. The median eminence, a central swelling located on the tuber cinereum, forms the floor of the third ventricle. The infundibulum is a stalk that connects the median eminence to the posterior lobe of the pituitary, and the mammillary bodies are two round protuberances at the posterior end of the inferior surface of the hypothalamus.
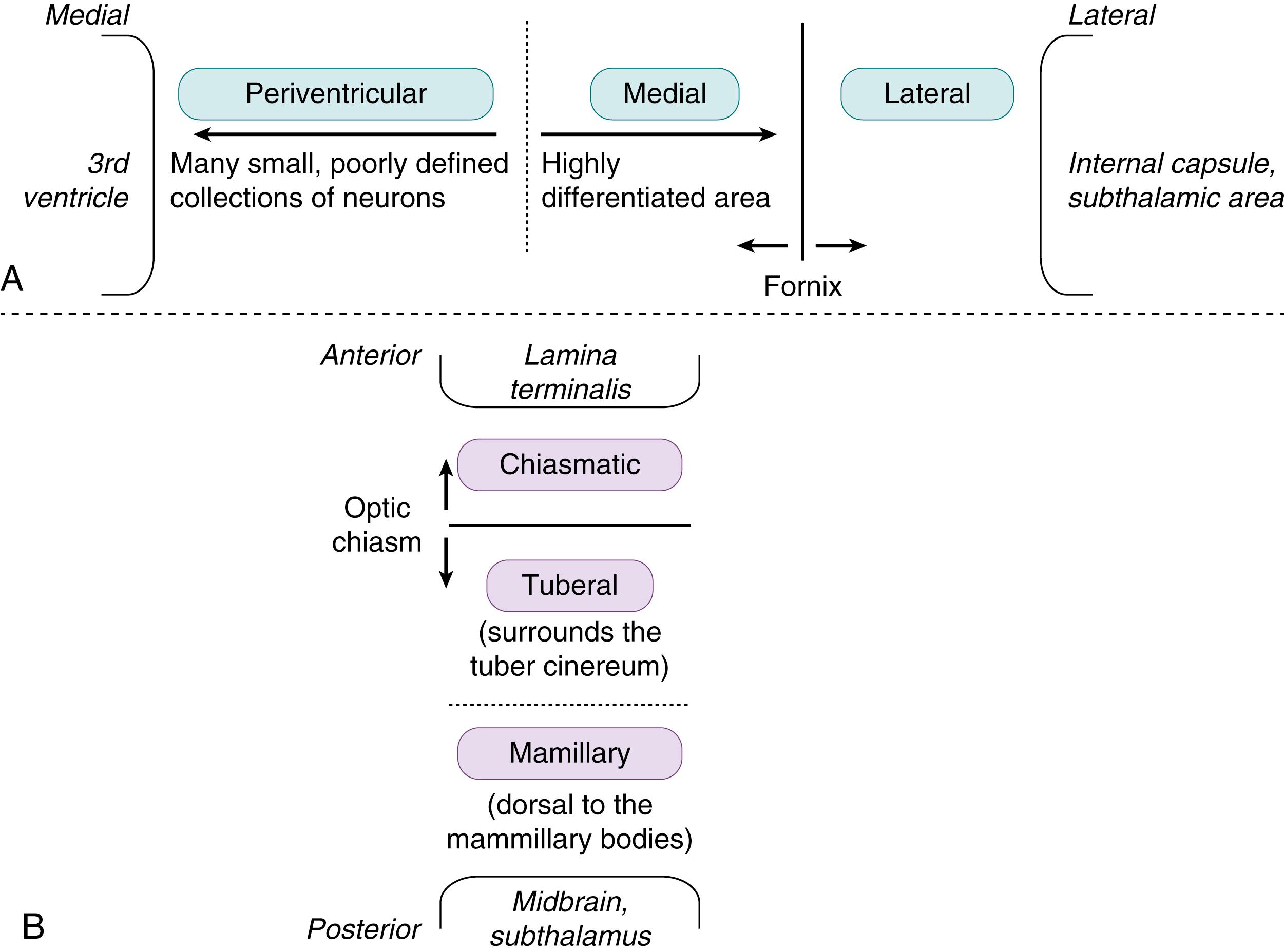
The hypothalamus can be difficult to describe because of its lack of landmarks. Of the many systems devised to divide the hypothalamus into discrete areas, two are particularly helpful. One describes nine zones, determined by their mediolateral and anteroposterior locations , ; it is shown in Fig. 139.1 . The second system defines discrete clusters of cell bodies (nuclei) that have characteristic anatomic positions and functions ( Table 139.1 ). Hypothalamic nuclei are not well circumscribed in adult brains. Examination of developing brains, in which cell groups are more discrete, has led to a greater understanding of hypothalamic architecture. Nonetheless, this schema is also semiarbitrary and is divided in many ways, depending on the source.
| Anteroposterior Region | Nuclei | Anatomy | Function |
|---|---|---|---|
| Chiasmatic | Preoptic area | Small nuclear groups, anterior to optic chiasm | Controls blood pressure, body temperature, hormonal release, reproductive activity |
| Suprachiasmatic nucleus | Midline nucleus above optic chiasm | Sets circadian rhythm and sleep-wake cycles, regulates body temperature, hormonal control | |
| Paraventricular nucleus | Medial half = parvocellular neurons; lateral half = magnocellular neurons | Produces oxytocin and antidiuretic hormone (magnocellular neurons); regulates anterior pituitary function (parvocellular neurons); regulates autonomic responses | |
| Supraoptic nucleus | Superior to optic chiasm; also contains magnocellular neurons | Produces oxytocin and antidiuretic hormone | |
| Anterior nucleus | Between the paraventricular and supraoptic nuclei | Less differentiated; role ill-defined | |
| Tuberal | Dorsomedial nucleus | Dorsal part of medial zone; projects locally and to periaqueductal gray matter | Feeding, growth, maturation, reproduction; parvocellular neurons regulate anterior pituitary function |
| Ventromedial nucleus | Ventral part of medial zone; projects locally and to periaqueductal gray matter | Feeding, growth, maturation, reproduction; parvocellular neurons regulate anterior pituitary function | |
| Arcuate nucleus | Basal portion of tuber cinereum | Parvocellular neurons regulate anterior pituitary function; dopaminergic neurons | |
| Lateral hypothalamic nucleus | Large neurons lateral to ventromedial nucleus | Signals hunger | |
| Mammillary | Posterior nucleus Mammillary nuclei |
Prominent nucleus, medial Complex of three or four nuclei |
Controls autonomic function Hippocampus → mammillary nuclei → thalamus; Papez circuit possibly involved in emotion and memory |
An area of particular controversy involves reports of sexual structural differences in several hypothalamic nuclei. In both rats and human adults, the sexually dimorphic nucleus of the preoptic area is larger in males than in females. , Another preoptic cell group was found to be larger in men. The bed nucleus of the stria terminalis is male predominant, , whereas the massa intermedia (interthalamic adhesion) is female predominant. Age-related changes in neuronal health and sex hormone activity can affect these differences. For example, because the cell loss of human senescence in the sexually dimorphic nucleus of the preoptic area follows different time courses in men and women, the magnitude of the structural difference is age dependent. , Sexual functional differences have also been shown in the hypothalamus by immunocytochemical staining for various neuronal products (e.g., somatostatin and vasopressin, also known as antidiuretic hormone [ ADH ]) and hormone receptors (e.g., androgen and estrogen receptors) and may also be age dependent. For example, the female dominance of neurokinin B immunoreactivity in the infundibular nucleus does not appear until puberty and progresses into adulthood. Speculation and controversy surround the implications for sexually dimorphic behaviors and psychological phenomena. Most relevant to neonatologists is the debate about imprinting of the brain by androgens in utero and its consequences for therapeutic outcomes in patients with various disorders of sex development, including ambiguous genitalia.
A final anatomic feature that is integral to hypothalamic functioning is blood supply. The hypothalamus communicates with the anterior pituitary gland through a special portal circulation that not only is fenestrated (the exception to the blood-brain barrier) but also transmits information bidirectionally. This feature enhances the ability of the hypothalamus to receive both signals from the general circulation and feedback from the pituitary. Furthermore, the hypothalamohypophysial portal system ensures that high concentrations of hypothalamic factors reach the pituitary, often at concentrations that far surpass those in the general circulation.
Early in nervous system development, three primary brain vesicles form from the neural tube: the prosencephalon or forebrain, the mesencephalon or midbrain, and the rhombencephalon or hindbrain. Secondary vesicles then form from the prosencephalon during the fourth to fifth weeks of gestation. The secondary vesicles are termed the telencephalon, or endbrain, and the diencephalon. The telencephalon grows to cover all other brain structures and eventually becomes the cerebral hemispheres. The diencephalon also grows, forming a roof plate and two alar plates. During the sixth embryonic week, neuroblasts in the inferior portion of the alar plates of the diencephalon proliferate, forming the human hypothalamus. , Hypothalamic development occurs in two main stages: forebrain induction by early signals before or during gastrulation and then cell type differentiation by ventralizing and rostralizing signals from the axial mesendoderm. Axial mesendoderm induction of hypothalamic development is necessary for eye separation, and its failure causes holoprosencephaly.
Distinct cell groups are easier to distinguish in the fetal hypothalamus than in the adult hypothalamus. The fetal hypothalamic nuclei become recognizable between 6 and 12 weeks of gestation. At this same time, the hypothalamic fiber tracts develop, and many hypothalamic factors become detectable. For example, somatostatin, dopamine, and thyrotropin-releasing hormone are detectable as early as the 10th week of gestation. At 9 to 10 weeks of gestation, little differentiation of the hypothalamic nuclei has occurred. By 24 to 33 weeks, the hypothalamus contains an increased number of better-defined structures and more closely resembles an adult hypothalamus. In the immediate postnatal period, the neonatal hypothalamic cell groups are remarkably similar to those structures in a mature adult.
Information regarding the embryology of the hypothalamohypophysial portal system is limited. Evidence exists that the primary plexus begins to develop as early as 11.5 weeks of gestation. Capillary penetrance of the median eminence is not evident until more than 16 weeks of gestation. Further development throughout gestation is indicated by the greater number of capillary loops and the maturer vasculature present at birth.
Our understanding of hypothalamic embryology has advanced from the morphologic to the genetic level. Development of the hypothalamus and pituitary gland is coordinated through parallel actions of genes expressed in both organs; extrinsic signals activate repertoires of transcription factors in a well-defined spatiotemporal pattern that leads to cellular differentiation into the various cell types that assume the distinct functions of the mature organs. , , Some of these genes are summarized in Table 139.2 . ,
| Gene | Normal Function | Consequences of Mutation or Deletion |
|---|---|---|
| HESX1 (also known as Rpx ) | Expressed during gastrulation in the midline endoderm-mesoderm (prechordal plate precursor), to induce anterior head structures | Deletions: absence of infundibulum and Rathke pouch (severest); hypothalamic floor expansion and abnormal bifurcation of Rathke pouch |
| Afterward, expression is restricted to Rathke pouch. Ventral → dorsal down-regulation of expression coincides with pituitary cell differentiation | Homozygous missense mutations (R53C) cause septooptic dysplasia, which is frequently associated with hypothalamic or pituitary dysfunction. Homozygous missense mutations (R160H) cause pan-hypopituitarism (anterior pituitary aplasia), thin pituitary stalk, but no midline defects (i.e., normal optic nerves) | |
| Shh | Expressed by oral ectoderm | Holoprosencephaly |
| Induces its own expression and that of other genes (e.g., Nkx-2.1 ) in ventral midline neural cells | Hypothalamic or pituitary absence or dysfunction | |
| Suppresses Pax6 expression in the midline | ||
| Required for resolution of the single retinal field into 2 separate primordia | ||
| Six3 | Transcription factor | Holoprosencephaly |
| Expressed in Rathke pouch and hypothalamus | Hypothalamic or pituitary absence or dysfunction | |
| Involved in early induction of the pituitary gland | ||
| Gli3 | Represses Shh signaling | Pallister-Hall syndrome (hypothalamic hamartomas) |
| Nkx-2.1 (also known as Tebp and TTF1 ) | Dorsoventral gradient of expression (higher in ventral region and posterior pituitary; none in Rathke pouch). Required for development of Rathke pouch | Absence of entire pituitary gland. Absence of selective hypothalamic nuclei (premammillary nucleus, arcuate nucleus, mammillary body, supramammillary nucleus) |
| Brn2 | Coexpressed with Brn4 in presumptive paraventricular and supraoptic nuclei | Magnocellular and parvocellular neurons fail to project axons into the posterior pituitary |
| Required for terminal differentiation and survival of magnocellular and parvocellular neurons in these nuclei | Complete loss of posterior pituitary | |
| Sim1 | Expressed in paraventricular and supraoptic nuclei | Paraventricular and supraoptic nuclei fail to express Brn2, oxytocin, antidiuretic hormone, thyrotropin-releasing hormone, corticotropin-releasing hormone, and somatostatin |
| Homozygous deletion: perinatal lethal from complete development defect of paraventricular nucleus | ||
| Haploinsufficiency: isolated hyperphagia, severe early onset obesity, increased linear growth, no decrease in energy expenditure | ||
| Nhlh2 | Expressed in developing hypothalamus | Hypogonadism and progressive adult obesity |
| Expressed in both embryonic and adult pituitary | Reduction of abundance of proopiomelanocortin-producing cells in the arcuate nucleus (increased leptin resistance) | |
| SF1 (also known as Ftzf1 ) | Expressed in developing adrenal glands, gonads, and diencephalon | Absence of adrenal glands. Absence of gonads |
| Regulates both androgens and müllerian inhibiting factor (i.e., male differentiation) | Absence of pituitary gonadotropes (no luteinizing hormone, follicle-stimulating hormone, and gonadotropin-releasing hormone) | |
| GSH1 | Binds to growth hormone–releasing hormone promoter | Hypoplastic pituitary gland |
| Dwarfism; growth hormone deficiency (from absence of growth hormone–releasing hormone in arcuate nucleus). Sexual infantilism and infertility | ||
| NDN | Paternal monoallelic expression in developing hypothalamus | Decreased number of oxytocin-producing cells in paraventricular nucleus |
| Decreased number of gonadotropin-releasing hormone–producing cells in preoptic region | ||
| Mutant mice show neonatal lethality with reduced penetrance | ||
| Maps to the critical region of Prader-Willi syndrome | ||
| Peg3 | Paternal monoallelic expression in developing hypothalamus | Decreased number of oxytocin-producing cells in paraventricular nucleus |
| Abnormal maternal behavior leading to perinatal lethality of offspring mice | ||
| Sox2 | Expressed in the developing central nervous system and placodes | Heterozygous mutations in humans: bilateral eye defects, anterior pituitary hypoplasia and hypogonadotropic hypogonadism, variable defects affecting the corpus callosum and mesial temporal structures, hypothalamic hamartoma, sensorineural hearing loss, esophageal atresia |
| SOX3 | Expressed in infundibulum | X-linked hypopituitarism, infundibular hypoplasia, variable learning difficulties |
| KAL1 | Encodes anosmin, a cell-surface protein that is proteolyzed to release a diffusible component that is incorporated into the extracellular matrix; promotes migration of olfactory axons and gonadotropin-releasing hormone neurons | X-linked Kallmann syndrome (hypoplasia of olfactory bulbs and absence of GnRH neurons from hypothalamus, leading to anosmia and hypogonadotropic hypogonadism) |
| PROKR2 | Expressed in brain, testis, small intestine (ileocecum), ovary, thyroid, pituitary, and salivary gland | Heterozygous or homozygous mutations cause Kallmann syndrome; mutations also found in patients with congenital hypopituitarism and septooptic dysplasia |
| Prokr2 −/− mice: partially penetrant postnatal lethality; surviving mice were underweight, failed to breed, and were hypokinetic, with nocturnal locomotor activity unsynchronized from circadian night |
Like other brain centers, the hypothalamus participates in neural pathways by synthesizing and secreting neurotransmitters that are chemical messengers used for synaptic transmission, signaling, and neuromodulation. Different pathways control various functions of the hypothalamus, although for some functions, discrete areas or nuclei are not identifiable as the control centers. Some of the neurotransmitters are summarized in Table 139.3 . For example, several hypothalamic nuclei project to the medulla oblongata to maintain homeostatic functions via the serotonergic system. Other neurotransmitters are also involved in hypothalamic functioning, such as the excitatory amino acids in a pathway connecting to the hippocampus and limbic system, but their actions are less well understood.
| Category | Neurotransmitter | Pathway | Function |
|---|---|---|---|
| Monoamines | |||
| Catecholamines | Dopamine | Incertohypothalamic tract | Influences secretion of pituitary hormones |
| Mesencephalic tract | Primary inhibitor of prolactin | ||
| Tuberoinfundibular tract | l -Dopa stimulates GH release | ||
| Median eminence | |||
| Norepinephrine | Lateral tegmental system | Regulates emotional and motivated behavior | |
| Dorsal tegmental system | Stimulates GH and gonadotropin release | ||
| Can be localized to all hypothalamic nuclei; highest concentrations in the arcuate nucleus and median eminence | Inhibits secretion of oxytocin, ADH, and corticotropin | ||
| Epinephrine | Cell bodies near the locus ceruleus | Inhibits secretion of ADH and oxytocin | |
| Indolamines | Serotonin | Most of the hypothalamic nuclei | Involved in cyclic release of some hypothalamic hormones |
| Highest concentrations in the arcuate and suprachiasmatic nucleus | Stimulates GH and prolactin release | ||
| Histamine | Tuberomammillary nucleus in the posterior lateral hypothalamus | May help maintain arousal. Stimulates oxytocin, ADH, and GH release | |
| Cholinergic | Acetylcholine | Large amount present in median eminence | Stimulates secretion of ADH, oxytocin, corticotropin, and gonadotropin. Inhibits somatostatin; stimulates GH release. Inhibits TSH release |
| Amino acids (inhibitory) | γ-Aminobutyric acid | Synthesized from glutamate. Basal ganglial system | In anterior hypothalamus, helps induce sleep. Inhibits oxytocin, ADH, corticotropin, prolactin, and TSH release. Stimulates GH and gonadotropin release |
| Peptides | Angiotensin II | Renin (from kidneys) cleaves angiotensinogen (made by liver) to angiotensin I; angiotensin I is cleaved by angiotensin-converting enzyme in lungs to angiotensin II | Stimulates secretion of ADH. Stimulates corticotropin and luteinizing hormone and inhibits prolactin and GH release. Induces thirst, drinking behavior. Involved in regulation of water balance |
| Atrial natriuretic peptide | Left atrium | Opposes ADH secretion | |
| Anterior tip of third ventricle | Involved in regulation of water balance | ||
| Many neuronal endings in the median eminence | |||
| β-Endorphins | Arcuate nucleus and basal tuberal area in the rat; project through the anterior hypothalamic area and innervate the median eminence | Released during stress. Stimulate corticotropin, prolactin, and GH release | |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here