Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The Papillomaviridae, Parvoviridae, and Polyomaviridae are three families of small, nonenveloped, DNA viruses. Despite their structural and taxonomic similarities, these viruses infect different tissue types and cause very different human diseases. This chapter examines the viruses in each family that are responsible for the most significant forms of human infection.
Human papillomaviruses (HPVs) are members of the Papillomaviridae family. These epitheliotropic viruses have a double-stranded circular DNA genome encapsulated within a nonenveloped viral particle and are grouped into more than 120 types based on genetic sequences of the L1 outer capsid protein. HPV has a high prevalence worldwide and infects a variety of anatomic sites, including the skin, male and female genital tracts, and oropharynx/larynx. Although infection is benign, in the majority of cases, many types are associated with premalignant changes and frank malignancy in a variety of tissues. Given the variety of lesions and clinical presentations associated with HPV infection, we have elected to focus on the more common and clinically important lesions, namely, cutaneous and anogenital warts and HPV-associated dysplasia and malignancy of the anogenital tract and oropharynx.
Infection begins when HPV enters the body through small abrasions, cuts, or tears in the skin or mucosal membranes. The virus then infects the basal keratinocytes that have the potential for differentiation and assumes control of cellular processes to make viral DNA and proteins. New viruses are assembled and released from the surface of the epithelium; there is no recognized blood-borne or systemic phase.
Based on their tissue tropism, HPV types are characterized as cutaneotropic or mucosotropic. Of the cutaneotropic viruses, HPV types 1, 4, 5, 8, 41, 48, 60, 63, and 65 are frequently identified in patients with cutaneous plantar warts, verruciform epidermodysplasia, and, rarely, cutaneous tumors. There are approximately 40 mucosotropic HPV types linked to human mucosal infection of the anogenital tract and head and neck, with these types being further classified as low risk and high risk based on their ability to induce malignant transformation of the infected cells. Low-risk HPV types such as HPV 6 and 11 are typically involved in nondysplastic lesions such as anogenital warts (condyloma acuminatum) of the vulva, vagina, and perianal regions and in laryngeal papillomatosis, whereas high-risk types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68, 69, 73, and 82 are associated with more than 95% of all cervical, vulvar, vaginal, penile, and anal squamous dysplasia and carcinoma. Specifically, HPV types 16 and 18 account for approximately 70% of cervical cancers worldwide, with HPV 16 accounting for 50% of cervical cancers. Given this high association, infection with HPV high-risk types is considered a necessary factor in the development of cervical cancer.
In the skin, the most common manifestation of HPV infection is the wart or verruca. Cutaneous warts are seen mostly in children and young adults, although they are also common in meat, poultry, and fish handlers. Patients at risk for more extensive or intractable skin involvement include those with atopic dermatitis or decreased cell-mediated immunity (e.g., solid-organ transplant recipients and patients with AIDS).
In contrast to cutaneous infection, anogenital HPV infection is primarily a sexually transmitted disease, with potential involvement of the cervix, vulva, vagina, scrotum, penis, perianal skin, and anal canal. Of these locations, the ectocervical-endocervical transformation zone and the pectineal line of the anal canal have the highest risk of infection with subsequent neoplastic transformation. The risk of cervical infection is thought to be the highest in young women because their transformation zone is exposed outside of the cervical os. With increasing age, the transformation zone recedes inside the cervical os where it is more protected from infection.
Anogenital infection is extremely common worldwide, with approximately 50% of all sexually active men and women acquiring infection in their lifetime. Risk factors for infection include an early age at first sexual encounter, a high number of sexual partners, smoking, immunocompromised state, and sex with high-risk individuals. Male circumcision and use of condoms have been shown to have a protective but not entirely preventative effect on acquisition of HPV infection.
Despite the high rates of anogenital HPV infection, most cases will spontaneously resolve, even when associated with low-grade dysplastic changes. Only a small percentage of infections persist for more than 1 year, and prospective studies have clearly demonstrated that persistent infection with high-risk types is required for development, maintenance, and progression of dysplastic lesions to invasive carcinoma. Infection typically precedes the development of malignancy by 10 to 15 years, thus providing a great window of opportunity for detection and removal of premalignant lesions using cervical cytology and HPV testing. Screening programs allow for multiple opportunities to detect and treat high-grade dysplastic lesions before they progress. It is estimated that greater than 10,000 women get cervical cancer in the United States each year due to HPV infection, and these cases are mostly in women who have never, or only rarely, undergone screening, or do not get appropriate follow-up following identification of a high-grade lesion. Women who are less likely to undergo regular screening include minorities, those with low socioeconomic status, those with no regular health care provider, and foreign-born women who have been in the United States for less than 10 years.
Other anogenital malignancies associated with HPV infection are less common than cervical cancer. According to the Centers for Disease Control and Prevention (CDC), there are about 2100 women who get HPV-associated vulvar cancer, 500 women who get HPV-associated vaginal cancer, 600 men who get HPV-associated penile cancer, and 2800 women and 1500 men who get HPV-associated anal cancer. A report by the American Cancer Society revealed that anal and vulvar cancers have been increasing.
The majority of anal cancers are caused by HPV 16, whereas HPV types 16 and 18 cause approximately 50% of penile, vulvar, and vaginal cancers. Similar to cervical dysplasia and carcinoma, HPV-dependent carcinogenesis is characterized by a stepwise progression through identifiable dysplastic precursor lesions, thus providing an opportunity for detection and intervention.
Finally, a significant number of HPV infections and associated malignancies occur in the oropharynx and larynx. In the United States, the percentage of oral cancers associated with HPV infection increased from 16% in the 1980s to 72% by 2004, surpassing tobacco and alcohol use as causative agents. According to the CDC, it is estimated that approximately 8400 out of 11,629 cases of oropharyngeal cancers are now associated with HPV infection in both men and women each year in the United States. By 2020, HPV will likely cause more oropharyngeal cancers than cervical cancers in the United States.
Having an understanding of certain HPV molecular characteristics is important for appreciating the pathways responsible for malignant transformation of infected cells and understanding the mechanisms behind HPV detection and vaccination. The genome of HPV virus contains three regions: early genes (E1-E8), late genes (L1 and L2), and the long control region. Of the early region genes, E6 and E7 are involved in host cell transformation and immortalization. These genes encode proteins that are associated with malignancy, whereas the L1 gene encodes the major capsid protein, which is highly conserved among HPV types. The L1 gene product is an abundant and highly immunogenic protein and is therefore the primary antigen used in HPV vaccine production. The L1 gene is also targeted by some commercially available molecular assays.
Based on the state of HPV within host cells, infection in human tissue can be divided into two biologic stages. Most of HPV infection stays at the episomal stage in which the virus forms circular viral particles coated with HPV L1 and L2 capsid proteins in the host cell cytoplasm. This stage is usually seen in condyloma acuminatum, as well as in the early dysplastic lesions caused by high-risk HPV infection referred to as low-grade squamous intraepithelial lesions (LSIL). The second biologic stage typically occurs after longstanding persistent HPV infection, in which viral DNA becomes integrated into the host genome. This is usually seen in high-grade squamous intraepithelial lesions (HSIL), the later stage of dysplasia caused by infection with high-risk HPV types, and in squamous cell carcinoma (SCC). Once integrated, viral DNA will actively produce E6 and E7 oncoproteins, which then associate with and disrupt the function of host cell tumor suppressors p53 and pRB, respectively. Expression of E6 and E7 is not thought to be sufficient for development of malignancy but seems to be involved throughout the multistep process of carcinogenesis. Of note, E6 and E7 genes of low-risk HPVs are unable to immortalize human cells, which is an important differentiating feature between high- and low-risk HPV types.
P16, the cyclin-dependent kinase inhibitor 2A (CDKN2A) gene product, is aberrantly expressed during HPV-induced tumorigenesis. In normal cells, the expression of p16 is negatively regulated by the pRb protein, whereas in HPV-infected cells, particularly when integration of viral DNA has occurred, E7 -mediated loss of pRb function contributes to p16 overexpression. As a result, p16 is overexpressed in HPV-related high-grade dysplasia and cancer and serves as a sensitive and specific surrogate marker for HSIL. This is reflected in the Lower Anogenital Squamous Terminology (LAST) guidelines released by the College of American Pathologists (CAP) and American Society for Colposcopy and Cervical Pathology (ASCCP); these guidelines recommend using p16 immunohistochemistry in confirming the identification of HSIL of the cervix, vulva, and anus.
Cutaneous warts vary in appearance depending on their location, ranging from flat smooth forms to rough papules. Typical locations include the hands, including around the nails (periungual warts) and palms (palmar warts), face, and the pressure-bearing regions of the soles (plantar warts). Warts may be found singly or in groups and occasionally coalesce into large plaques. Warts are often asymptomatic and concerning more for their cosmetic appearance than the physical discomfort they cause. Plantar warts, however, may be particularly painful.
Genital warts (condyloma acuminatum) present as a verrucous, cauliflower-like excrescences of anogenital skin. These warts may be numerous and become confluent, particularly in individuals with a compromised immune system ( Figure 4-1 ).

In contrast to benign lesions, premalignant lesions can be less obvious or asymptomatic. Severe squamous dysplasia is often in the form of one or several well-demarcated, erythematous, slightly thickened, and sometimes hyperkeratotic plaques. Invasive SCC usually appears as an indurated, sometimes ulcerated plaque or nodule ( Figure 4-2 ). Patients with cervical carcinoma may present with pain or bleeding during intercourse.

In the head and neck, HPV-associated carcinomas more often present at a higher clinical stage than their non-HPV-associated counterpart lesions, with patients presenting with metastatic disease involving the neck lymph nodes. The primary malignancy, usually in the tonsil or base of the tongue, is often unnoticed initially.
Diagnosis of verrucae is typically based on observation of their characteristic clinical appearance. If there is doubt, a blade can be used to scrape off any hyperkeratotic debris to reveal thrombosed capillaries (also known as “seeds”) that are common in warts. If dermatoscopic examination is performed, the thrombosed capillaries may appear as homogenous black to red dots and globules. Rarely, a biopsy with histopathologic examination is required to confirm the diagnosis. Like their cutaneous counterpart, genital warts may be diagnosed clinically or with biopsy confirmation.
In the anogenital tract, cervical and anal cytology play an important role in screening and identifying women and men with precancerous lesions. Cervical cytology using either conventional or liquid-based preparations has a high specificity but low sensitivity for detection of high-grade dysplasia. In contrast, detection of high-risk HPV types has a high sensitivity but low specificity for predicting the presence of high-grade dysplasia on subsequent biopsy. The specific detection of high-risk HPV types 16 and 18 provides additional specificity. When used according to current cervical cancer screening algorithms, cytology, high-risk HPV testing, and detection of HPV 16/18 has significantly increased our ability to identify women with high-risk lesions. We refer readers to the guidelines for cervical cancer screening put forth by the American Cancer Society, American Society for Clinical Pathology, and the ASCCP (2012), as well as guidelines presented by the American College of Obstetricians and Gynecologists (2012) and the U.S. Preventative Services Task Force (2012) for further information.
Several molecular platforms have been approved by the U.S. Food and Drug Administration (FDA) that employ signal and target amplification methods for detecting high-risk HPV types. There are also FDA-approved tests for specific detection of HPV 16 and 18. At the present time, these methods are only approved by the FDA for use with cervical specimens collected in ThinPrep PreservCyt media (or Digene Specimen Transport Media for use with the Digene Hybrid Capture 2 HPV DNA Test); additional validation must be performed by laboratories wishing to test specimens collected in other media. In the current screening algorithms, women with high-grade cytology or high-risk HPV positivity should progress to colposcopy-guided biopsy for histopathologic confirmation of dysplasia. The LAST guidelines provide a universal approach for the interpretation of all HPV-associated intraepithelial lesions of the cervix, vulva, vagina, penis, and anus on biopsy specimens using the two-tiered classification employed in cytology (i.e., LSIL and HSIL). In this new system, intraepithelial neoplasia (IN) level 1 is reported as LSIL, whereas IN 2 and 3 are reported as HSIL. The lesion can then be further subclassified by its IN terminology: CIN, VIN, VAIN, PeIN, and AIN, for cervical, vulvar, vaginal, penile, and anal intraepithelial neoplasia, respectively.
In the head and neck region, laryngoscopy and biopsy play an important role in the diagnosis of benign HPV-related lesions. In malignant lesions, however, the primary lesion may go unnoticed until patients present with metastatic disease, most commonly involving neck lymph nodes. Fine-needle aspiration or biopsy of enlarged neck lymph nodes is often required for identifying these metastatic squamous cell carcinomas. The primary tumor is then subsequently identified during tonsillectomy or biopsy of the base of the tongue.
HPV viruses are small, epitheliotropic, icosahedral, nonenveloped, double-stranded DNA viruses.
They infect a variety of anatomic sites, including the skin, anogenital tracts, and oropharynx/larynx.
Worldwide distribution.
Skin warts are common in children, young adults, and meat, poultry, and fish handlers.
Anogenital HPV infection is extremely common in men and women. Most infections regress spontaneously.
Almost all cervical dysplasia and malignancy are HPV associated, with types 16 and 18 being found in 50% to 70% of high-grade cervical squamous intraepithelial lesions (SILs) and invasive cervical carcinoma.
Approximately 10,000 women acquire cervical cancer annually in the United States.
HPV infection is also now associated with up to 72% of oropharyngeal cancers in the United States.
Cutaneous warts may be single or multiple and range from flat to papillary lesions.
Genital warts typically present as a verrucous, cauliflower-like excrescences. Numerous warts may be seen in immunocompromised individuals.
Premalignant lesions of the anogenital tract are often asymptomatic. Severe squamous dysplasia often presents as well-demarcated, erythematous, slightly thickened, and sometimes hyperkeratotic plaques. Invasive squamous cell carcinoma usually appears as an indurated, sometimes ulcerated plaque or nodule.
HPV-associated oropharyngeal and laryngeal carcinomas more often present at a higher clinical stage than their non-HPV-associated counterpart lesions, with patients presenting with metastatic disease involving the neck lymph nodes. The primary malignancy, usually in the tonsil or base of the tongue, is often unnoticed initially.
Wart treatment depends on the type of wart, location, degree of symptoms, and underlying immune status. Therapies are designed to destroy the virus-containing epidermis. Spontaneous regression occurs in as many as two thirds of warts within 2 years.
Excision or ablation is the choice for high-grade dysplasia of the cervix.
Cervical squamous cell carcinoma is an aggressive malignancy clinically, with 5-year survival rates of 93%, 63%, and 35% for stages IA, IIA, and IIIA, respectively.
HPV-positive oropharyngeal and laryngeal squamous cell carcinomas have a significantly better prognosis than their HPV-negative counterparts.
Cutaneous lesions associated with HPV infection.
In general, HPV infection and associated lesions are diagnosed using small biopsies that have nonspecific gross findings. The exception to this is with warts or condylomas, which when removed intact demonstrate the features described in the clinical signs and symptoms section presented earlier.
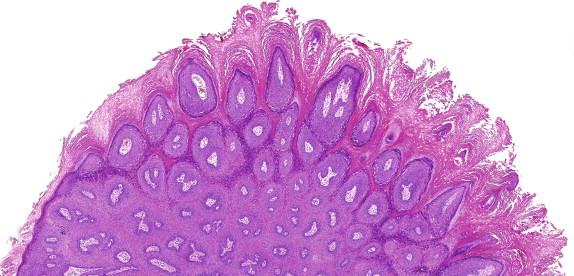
Histopathologically, common warts typically have an acanthotic epidermis with prominent papillomatosis, hyperkeratosis, and parakeratosis ( Figures 4-3 and 4-4 ). Prominent dermal blood vessels may be observed and are sometimes thrombosed. Large keratinocytes with eccentric pyknotic nuclei surrounded by a perinuclear halo (koilocytes) may be present but are often absent in older lesions. Infected cells may also contain numerous basophilic keratohyaline granules and small eosinophilic granules. It is worthwhile pointing out that these are not HPV viral particles. Flat warts do not exhibit papillomatosis and have less hyperkeratosis and acanthosis.
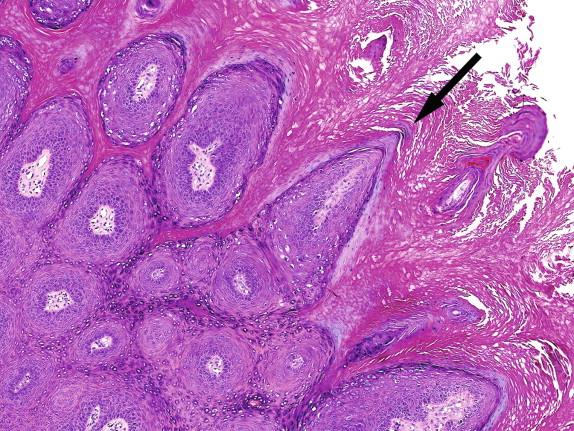
Genital warts (condyloma acuminatum) are characterized by complex branching exophytic papillae composed of acanthotic squamous epithelium and fibrovascular cores and an endophytic or downward proliferation of rete pegs. Koilocytes are usually present at the superficial layers.
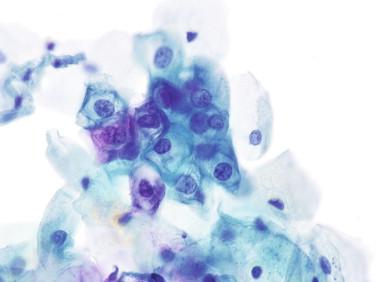
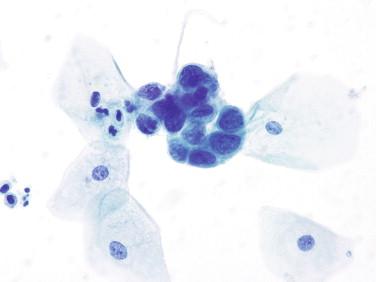
Low-grade squamous intraepithelial lesions are characterized by thickened squamous epithelium, variation of cell size and shape, and koilocytosis ( Figures 4-5 and 4-6 ) at the superficial or intermediate layers. In vulvar lesions, LSIL is often associated with hyperkeratosis and an undulated warty surface. The basal layer is proliferative but does not exceed one third of the full epidermal thickness. Mitoses are usually frequent.
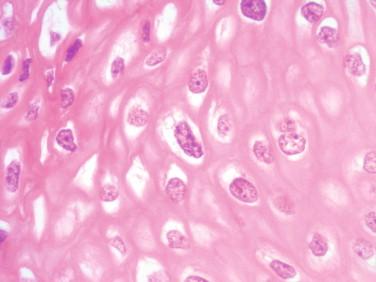
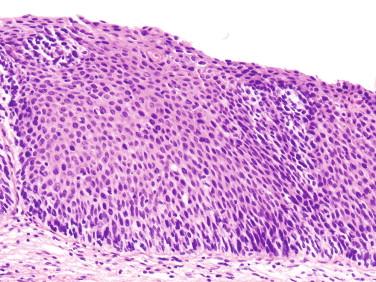
In contrast to LSIL, the HSIL lesion is characterized by clonal expansion of atypical basal cells, which extend beyond one third of the epidermis. Dysplastic cells in HSIL are usually less dramatically enlarged than those of LSIL but have a much higher nuclear/cytoplasmic (N/C) ratio, coarse chromatin, and thickened nuclear membranes ( Figures 4-7 and 4-8 ). Koilocytotic change is seen less often. Mitosis can be brisk. In contrast to LSIL, the thickness of HSIL can be much thinner than normal squamous epithelium, which is one of the reasons attributed to low accuracy of conventional acetic acid colposcopy-guided biopsy.
Finally, HPV-related head and neck cancers are often nonkeratinized squamous cell carcinoma and prominent basaloid features. Lymphoepithelial features may also be seen. Although these histopathologic features are associated with HPV-positive squamous cell carcinoma of the oropharyngeal and laryngeal regions, immunohistochemical staining for p16 and HPV ISH should be applied to confirm the relationship with HPV infection.
Both immunohistochemical staining (IHC) for p16 and HPV in situ hybridization (ISH) are commonly used ancillary methods for addressing anogenital lesions and cancers of the mouth and throat. HPV in situ hybridization is particularly useful when trying to differentiate between a condyloma and a non-HPV-related papilloma, as the former will usually be positive for low-risk HPV types. As discussed previously, immunohistochemistry for p16 antigen is recommended by the LAST guidelines for confirming a diagnosis of CIN 2, thus differentiating between low-grade dysplasia (p16 negative/focal positive) and high-grade dysplasia (p16 diffusely positive). HPV ISH staining is also used for confirming the presence of viral DNA in squamous cell carcinomas of the oropharynx and larynx. Due to the lower analytical sensitivity (65% to 90%) for HPV ISH in identifying HPV on formalin-fixed paraffin-embeded tissue, compared to HPV testing in liquid cytologic materials (sensitivity 94% to 97%), a negative HPV ISH result does not necessarily exclude HPV infection. In contrast, the strong and diffuse p16 immunostaining in an oropharyngeal cancer highly indicates its association with HPV infection.
Common warts are characterized by acanthosis, papillomatosis, hyperkeratosis, parakeratosis, prominent keratohyaline granules, and elongated rete ridges. Koilocytes are common but may be absent in older lesions.
Low-grade squamous intraepithelial lesions of the anogenital tract demonstrate thickened squamous epithelium and prominent koilocytosis. The basal layer is proliferative but does not exceed one third of the full epidermal thickness.
High-grade squamous intraepithelial lesions of the anogenital tract contain enlarged nuclei atypical with a high nuclear/cytoplasmic ratio, coarse chromatin, and thickened nuclear membranes. Atypical cells extend through one third or more of the epidermal layer. Immunohistochemistry for p16 is useful for differentiating LSIL and HSIL in questionable cases.
HPV-related head and neck cancers are often nonkeratinized squamous cell carcinomas with “basaloid” features. Immunohistochemical staining for p16 and HPV ISH should be applied to determine the relationship with HPV infection.
Skin warts can be confused with lichen planus, seborrheic keratosis, and skin tags both clinically and histopathologically, whereas the flat-topped papules of lichen planus and globoid papules of lichen nitidus may be confused clinically with verruca plana (flat warts). Compared to the typical gross appearance of warts, seborrheic keratoses have a stuck-on appearance, are commonly pigmented, and have visible “horn cysts” on close examination. Similarly, acrochordons (skin tags) superficially resemble the papillary protuberances of warts but are usually smooth and pedunculated. These entities are differentiated histologically by their lack of characteristic verruca features such as koilocytic change, prominent keratohyaline granules, papillary appearance, and spires of parakeratosis.
The histopathologic differential diagnosis of LSIL includes reactive changes secondary to inflammation, uterine prolapse-related changes, and condyloma. HSIL can be confused with atrophy, immature squamous metaplasia, regenerative changes, and sometimes endometrial breakdown stroma. As discussed previously, p16 IHC can be used to accurately differentiate HSIL from LSIL and can also be used to differentiate HSIL from nondysplastic HSIL mimics.
In oropharyngeal and laryngeal carcinoma, the most important histopathologic consideration is classifying the lesion as HPV positive or HPV negative, thus highlighting the role of HPV ISH. This HPV result will be used to guide treatment and predict prognosis.
Warts are benign growths that are primarily of cosmetic importance, and thus the type and aggressiveness of therapy will depend on the clinical appearance, location, degree of symptomatology, and patient immune status. Current HPV therapies are not specific for the virus but rely primarily on tissue destruction, local chemotherapeutic effect, or enhancing innate immunity, with the goal of destroying viral-containing epidermis while preserving as much uninfected skin as possible. In general, relatively noninvasive and painless methods are employed on small lesions, whereas more aggressive therapies are reserved for large, recalcitrant, or highly symptomatic lesions. Common, plantar, and palmar warts are most commonly treated with salicylic acid or liquid nitrogen, whereas flat warts are most often treated with cryotherapy or topical applications of 5-fluorouracil, imiquimod, or tretinoin. Given that up to two thirds of warts may regress spontaneously within 2 years, observation alone may also be appropriate. However, it should be noted that warts may enlarge or multiply, thus making treatment more difficult, and new warts may appear while others are regressing. For this reason, many patients pursue treatment.
As mentioned previously, the majority of anogenital infections will regress spontaneously provided that the patient has a normal and healthy immune system. Therefore, the goal of published cervical cancer screening guidelines for normal-risk women is to prevent cervical cancer while avoiding excessive treatment of precursor lesions that are likely to resolve. To this end, cervical cytology and HPV testing are not recommended for women under the age of 21 due to the high rate of infection and subsequent resolution of HPV infection in young women. Given that longstanding HPV infection is required for development of most cervical malignancies, routine testing by cervical cytology +/− HPV at defined intervals has a high likelihood of detecting important precursor lesions.
Women with biopsy-confirmed diagnosis of HSIL typically proceed to loop electrosurgical excision procedure (LEEP) or cold knife cone in order to destroy or excise the entire squamous-columnar junction where the high-grade changes are present. Targeted cryotherapy or laser therapy may also be performed. Detection of high-risk HPV following these procedures is associated with a higher risk of dysplasia recurrence.
Cervical squamous cell carcinoma is an aggressive malignancy clinically. The 5-year survival rate of treated cervical squamous cell carcinoma depends on the stage of disease. The average 5-year survival for stages IA, IIA, and IIIA is 93%, 63%, and 35%, respectively, thus highlighting the utility for the early detection and treatment of premalignant lesions.
It is worth noting that there are no widely accepted screening algorithms for other HPV-related anogenital malignancies. However, screening for anal dysplasia is recommended by some specialists in high-risk populations such as men who are positive for the human immunodeficiency virus (HIV) and engage in anal receptive intercourse. Use of anal cytology-based screening has allowed for recognition and treatment of precursor lesions before they could progress to squamous cell carcinoma. The prognosis for anal cancer is stage dependent, with 5-year survival rates of 71%, 64%, 48%, 43%, and 21% for stages I, II, IIIA, IIIB, and IV squamous cell carcinoma, respectively, thus suggesting a role for screening in detecting high-grade dysplasia and early-stage malignancy.
It is well documented that HPV-positive oropharyngeal and laryngeal SCCs have a much better prognosis than HPV-negative SCCs, responding better to chemotherapeutic and radiation therapies than their HPV-negative counterparts. The reported 5-year survival rates are 62% and 26% for HPV and non-HPV-associated tumors with radiotherapy, respectively. Therefore, HPV ISH and p16 IHC positivity are important indicators of treatment response and prognosis.
The polyomaviruses are small (45 nm), icosahedral, nonenveloped, double-stranded DNA viruses that have genomes between 4.5 and 5.5 kb. Three polyomaviruses of primary medical importance are covered here. These are the BK virus (BKV), the JC virus (JCV), and the more recently described Merkel cell carcinoma virus (MCCV). A number of other polyomaviruses have been discovered, such as the KIV, WUV, TSV, and human polyomaviruses 7, 8, 9, and 10, but consideration of these in detail is beyond the scope of this text.
Polyomaviruses are highly prevalent in humans based on serologic studies. Exposure to BKV begins early in life, and seropositivity rates rise until around 40 years of age and then slightly decline. Exposure to JCV also begins in childhood, but seropositive rates continue to rise throughout life. The seroprevalence for BKV is greater than 90%, whereas the seroprevalence for JCV is between 50% and 80%. Although fewer studies have examined the seroprevalence rates of MCCV, the adult seroprevalence is likely between 60% and 80%.
BK and JC viruses cause asymptomatic infections to subclinical disease in the immunocompetent host and go unrecognized during the primary infection. After infection, viremia is thought to occur, wherein the virus disseminate to both sites of latency and sites permissive for low-grade, subclinical viral replication. Evidence of subclinical ongoing replication and latency include studies that have demonstrated asymptomatic viral shedding into the urine of pregnant women and detectable virus in the bone marrow and splenic tissue of HIV-infected patients that was obtained for other reasons long before they developed progressive multifocal leukoencephalopathy (PML).
The prevalence of clinically appreciable disease caused by BKV and JCV is limited to populations of immunocompromised patients. The populations at highest risk for disease are those with advanced HIV infection (i.e., AIDS) and transplant recipients.
Polyomaviruses belong to the genus Orthopolyomavirus . These viruses infect a variety of animals, including humans. There is a high degree of genetic homology between the polyomaviruses. Although both humans and animals are infected by polyomaviruses, specific polyomaviruses largely infect a particular group of animals. Polyomaviruses that infect humans are thought to be largely restricted to causing human infections.
Both BK and the JC viruses were discovered in 1971, interestingly by different researchers. BK virus was discovered in a renal transplant recipient with ureteral stenosis, whereas JC virus was discovered in the brain of a patient with PML who had lymphoma. These two viruses received their taxonomic designation (i.e., BK and JC) from the initials of the patients from whom they were originally isolated. Merkel cell carcinoma was originally described in 1972, but a viral mechanism of carcinogenesis was not suspected at that time. Advances in molecular diagnostic methods, such as digital transcriptome substraction, allowed for the detection and subsequent characterization of the MCCV genome that was integrated into the genome of this malignancy.
The small genomes of the polyomaviruses have been extensively studied. One of the major interests in these viruses is the large tumor (T) antigen protein and the encoding gene, which have been studied with respect to their role in carcinogenesis. This protein interacts with tumor suppressor genes, such as the retinoblastoma gene and p53, and inhibits apoptosis. It is not surprising that researchers have been tantalized by the potential connection between these common viruses and cancers and have therefore ardently sought a definitive link. Studies of these genetic elements and associated protein products have failed to show a direct link between BKV and JCV infection and human malignancy. However, a direct link has been established between MCCV and Merkel cell carcinoma.
One hypothesis regarding the lack of evidence for a direct cause of cancers by BK and JC viruses involves the difference between permissive and nonpermissive cells. When permissive cells are infected, viral replication ensues. When nonpermissive cells are infected and the virus becomes integrated, then cellular changes ensue that promote malignancy. Supportive of this hypothesis is the fact that BK and JC viruses in renal and CNS infections, respectively, infect permissive cells, whereas MCCV is integrated into the genome of the cells that constitute this malignancy.
The comparative analyses of a variety of strains of BK and JC polyomaviruses have demonstrated loci of genetic conservation, as well as loci of greater genetic variability. This information has proven useful in the construction of molecular diagnostic assays. Targeting the conserved regions for polymerase chain reaction (PCR) primer hybridization sites helps to assure the detection of the most strains possible. Two of the currently marketed products target the large T antigen gene and the VP2 and VP3 genes. The noncoding control region and the gene for the structural protein VP1 are areas that contain significant variability and should be avoided as targets for PCR primer hybridization sites.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here