Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Herpes zoster ophthalmicus (HZO) involves reactivation of latent varicella-zoster virus from the trigeminal sensory ganglia along the V1 distribution of the trigeminal nerve with ocular manifestations.
Severe corneal complications from HZO may include a secondary infectious keratitis, ulceration with hypopyon, ulceration with mild to moderate keratolysis, or corneal perforation.
Approximately 10%–20% of herpes zoster cases involve the ophthalmic nerve division, with 20%–70% developing ocular findings.
An estimated 10%–30% of patients have unremitting pain lasting months to years after the acute infection has resolved, a phenomenon known as postherpetic neuralgia (PHN). PHN is the most common complication of herpes zoster.
A new recombinant vaccine, Shingrix, has replaced Zostavax as the recommended vaccine to protect against herpes zoster for ages 50 and older.
Shingrix was 97% effective in preventing shingles in ages 50-69, 91% effective in ages 70 and older and 91% effective in preventing PHN.
Varicella-zoster virus (VZV) is a member of the herpes virus family that causes varicella (chickenpox), an extremely contagious form, and herpes zoster (shingles), a reactivated and latent form. Varicella represents a primary infection after exposure of a susceptible or seronegative individual to VZV. Herpes zoster (shingles) is caused by reactivation of a latent VZV infection.
Herpes zoster derives its name from the Greek words herpein, meaning “to spread” or “to creep,” and zoster, meaning “girdle” or “zone.” The lifetime risk of herpes zoster is estimated to be 10%–30%. The reported incidence of herpes zoster prior to vaccination ranged from 1.2 to 6.5 cases/1000 person-years, with approximately 500,000 cases annually in the United States. A number of studies have reported on herpes zoster incidence in the postvaccination era in comparison to the prevaccination era. The data remain inconclusive as some studies have found a small increase in incidence of herpes zoster while others have found no change in herpes zoster in the postvaccination era.
Increasing age represents a significant risk factor for the development of herpes zoster, and the likelihood of infection increases directly in proportion to age. The incidence in persons older than 75 years of age exceeds 10/1000 cases annually. In addition, an 85-year-old individual has a 50% probability of developing herpes zoster once and a 1% chance of herpes zoster appearing twice. Another important risk factor for the development of herpes zoster is altered cell-mediated immunity. Patients with neoplastic diseases, those taking immunosuppressive drugs, and organ-transplant recipients are particularly at risk for herpes zoster. Patients who are seropositive for human immunodeficiency virus (HIV) also develop herpes zoster with a higher frequency than the normal population. A longitudinal study confirmed an incidence of 29.4/1000 cases annually in HIV-seropositive patients compared to 2.0/1000 cases annually in HIV-seronegative controls. The likelihood of infection with zoster is inversely proportional to the host’s immune response.
Herpes zoster in children represents an uncommon finding with potentially devastating sequelae. The incidence of herpes zoster in children is estimated at 0.2/1000 cases per year in those less than 5 years of age, but increases to 0.6/1000 cases per year at age 15–19. The incidence of childhood zoster is 122 times higher in children with a childhood malignancy. Other risk factors for childhood zoster include maternal infection with varicella during pregnancy and varicella in the first year of life. Varicella vaccination can also be a risk factor for development of infection because current vaccines are made from live attenuated viruses. Children who develop varicella before 1 year of age have a relative risk between 2.8 and 20.9 for developing herpes zoster in childhood. In children and young adults, serum antibodies directed against VZV represent a good surrogate marker for cell-mediated immunity (i.e., antibodies correlate with T-cell reactivity to VZV). In elderly persons, the presence of antibody does not always indicate T-cell reactivity to VZV.
Herpes zoster is the clinical entity caused by reactivation of the latent VZV from sensory ganglia. Acute herpes zoster includes 1–4 days of prodromal symptoms including fever, malaise, headaches, and hypesthesias, with pain, burning, itching, erythema, and edema in the affected dermatome. Viral release from the sensory nerve endings results in a macular rash that becomes papular and then vesicular within 24 hours. The grouped vesicles usually involve one dermatome but can include up to three adjacent dermatomes. New vesicles continue to develop for about 4 days and may continue for weeks in immunosuppressed patients. The vesicles become pustular and may eventually rupture or hemorrhage. Hemorrhagic necrosis of the deeper dermal tissues may occur with a propensity for permanent pigmentation and residual scarring. Occasionally, an attack will occur without the cutaneous skin eruption (zoster sine herpetica). Visceral dissemination is a more severe complication of herpes zoster with the lungs and gastrointestinal system most commonly involved. After 2–3 weeks, the acute phase subsides and the rash crusts over and dissipates, yet the pain may persist in the dermatome affected, resulting in a condition known as postherpetic neuralgia (PHN).
While any sensory ganglia may be involved with herpes zoster, herpes zoster ophthalmicus (HZO) is used to describe reactivation from the trigeminal ganglia with ocular involvement. Hutchinson was the first to describe the signs and symptoms of HZO in 1865. Of the three divisions of the trigeminal nerve (ophthalmic, maxillary, and mandibular), the ophthalmic division is most commonly affected in herpes zoster, in 8%–56% of cases ( Fig. 79.1 ). , The ophthalmic division further divides into the nasociliary, frontal, and lacrimal branches, of which the frontal nerve is most commonly involved and the lacrimal branch is least commonly involved in HZO. The nasociliary nerve innervates the anterior and posterior ethmoidal sinuses, the skin of both eyelids, and the tip of the nose, conjunctiva, sclera, cornea, iris, and the choroid. Because of the extensive innervations of the nasociliary nerve, its involvement in HZO is associated with a 50%–76% chance of ocular complications, which lowers to 34% in cases of HZO without nasociliary involvement. Vesicles at the side of the tip of the nose are known as Hutchinson sign and are indicators of potential ocular disease.

Approximately 10%–20% of herpes zoster cases involve the ophthalmic nerve division with 20%–70% developing ocular findings. The presence of Hutchinson sign is a poor prognostic indicator because of the increased risk of ocular sequelae secondary to its extensive intraocular innervation. Ocular involvement is not correlated with age, sex, or severity of the skin rash. The diffuse and multiple ocular complications of HZO are related to different mechanisms of disease, including antigenic viral components, immune reaction, vasculitis, neural involvement, and scarring. The disease may manifest with acute, chronic, or relapsing phases, depending on the mechanisms involved. Chronic disease can be present in 20%–30% of HZO cases. While the visual outcome in HZO is extremely variable, the visual prognosis in African-Americans with a high prevalence of HIV infection carries a much worse prognosis.
Lid edema is usually the first sign of HZO, accompanied by pruritus, hypesthesia, or pain. A maculopapular rash follows the initial findings and progresses to a vesicular skin eruption. VZV can be cultured from the skin vesicles for up to 5–7 days. Depending on the depth of dermal involvement and the presence of a secondary bacterial infection (usually Streptococcus species or Staphylococcus aureus ), there can be variable sloughing of the skin with resultant cicatricial contracture or gangrene. In most patients, the vesicles heal within 2–3 weeks, leaving some residual pitting or pigmentation change. Other lid changes include trichiasis, ectropion, entropion, madarosis, or poliosis. A hemorrhagic vesicular eruption in the skin may be indicative of anticoagulant use, a hematologic disease, or a severe vasculitis; this eruption heralds severe dermal scarring and PHN. Cicatricial contraction of the eyelids may lead to chronic corneal exposure and may require plastic surgical repair to protect the integrity of the globe. Other chronic changes include excavated scars, pigment changes, lid margin notching, ptosis, and sloughing of the skin.
The conjunctival changes in HZO can include a papillary or follicular reaction, chronic hyperemia, and/or pseudomembrane formation. A vesicular eruption may occur within the conjunctiva, leading to vesicle rupture with possible hemorrhagic changes. With severe conjunctival changes, extensive conjunctival scarring and symblepharon formation may ensue. Extension of the conjunctival changes to the lacrimal puncta may result in punctal scarring, punctal occlusion, and epiphora. The conjunctival cytology consists of mononuclear cells and lymphocytes.
HZO can cause an episcleritis, anterior scleritis, or posterior scleritis. Both episclera and sclera can become affected during the acute stages of HZO or months later after the disappearance of vesicles. While episcleritis is typically found early in the course of HZO, it may persist up to and beyond 3 months in a significant number of patients. Scleritis is usually diffuse, anterior, or nodular in nature and has a tendency to progress toward the perilimbal area, resulting in a peripheral limbal vasculitis. Scleral thinning and staphyloma formation can occur as a result of chronic scleritis. Posterior scleritis is less common and typically results from an infiltrative process involving the perivascular and perineural tissue.
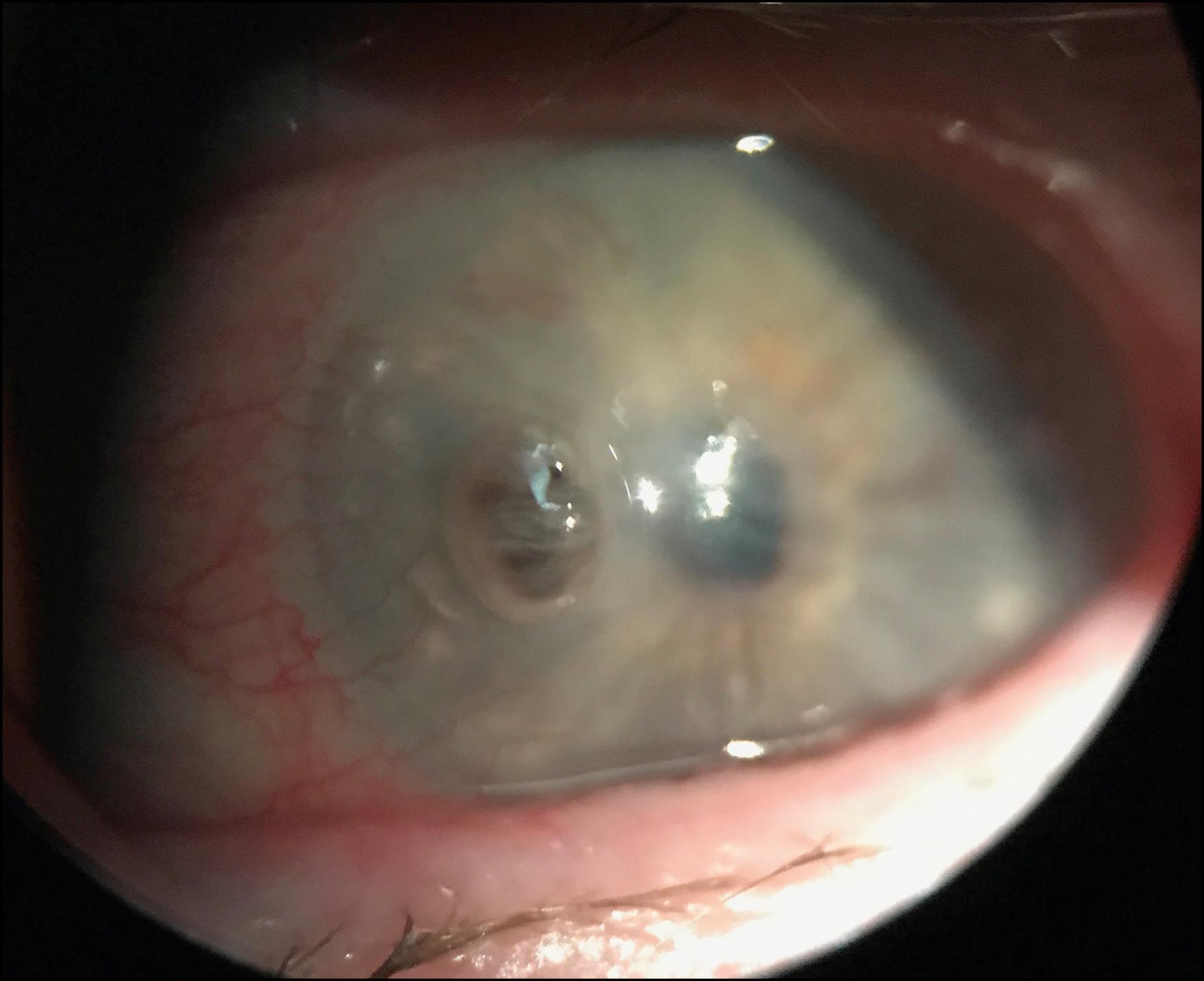
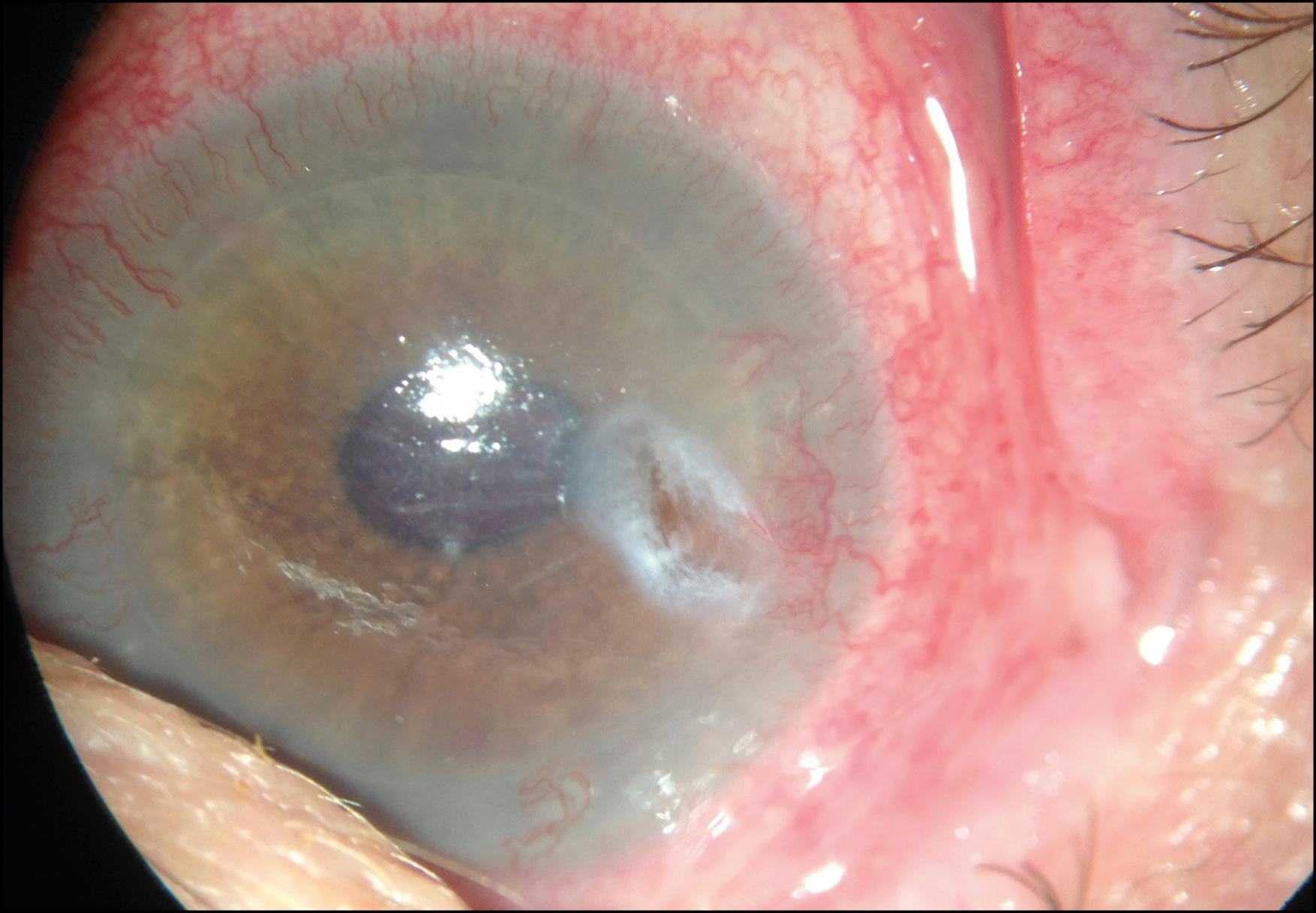
The cornea exhibits multiple manifestations, probably related to different mechanisms of disease. Corneal manifestations occur in about two-thirds of patients with ocular disease in acute HZO. It appears chronologically as punctate epithelial keratitis, early pseudodendrites, anterior stromal infiltrates, sclerokeratitis, keratouveitis/endotheliitis, serpiginous ulceration, neurotrophic keratopathy, and exposure keratopathy ( Table 79.1 ). , In severe cases, HZO may present with a secondary infectious keratitis, ulceration with a hypopyon, ulceration with mild to moderate keratolysis, descemetocele, or complete corneal perforation ( Figs. 79.2 and 79.3 ).
| Morphology/Pathogenesis | Frequency (%) | Usual Onset |
|---|---|---|
| Punctate epithelial keratitis | 50 | 2 days |
| Pseudodendritic keratitis | 50 | 4–6 days |
| Anterior stromal keratitis | 40 | 10 days |
| Keratouveitis/endotheliitis | 34 | 7 days |
| Serpiginous ulceration | 7 | 1 month |
| Sclerokeratitis | 1 | 1 month |
| Corneal mucous plaques | 13 | 2–3 months |
| Disciform keratitis | 10 | 3–4 months |
| Neurotrophic keratopathy | 25 | 2 months |
| Exposure keratopathy | 11 | 2–3 months |
| Interstitial keratitis/Lipid keratopathy | 15 | 1–2 years |
| Permanent corneal edema | 5 | 1–2 years |
The initial corneal manifestation is a coarse punctate epithelial keratitis with blotchy, swollen epithelial cells. They are usually peripheral, multiple, raised, small, and focal, and they stain with rose Bengal. A conjunctivitis usually accompanies the lesions. VZV has been cultured from these lesions.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here