Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
By the end of this chapter the reader should:
Know the anatomy and embryology of the liver and biliary tract and how variation relates to specific disorders, e.g. biliary atresia
Know the basic histopathology and cellular dysfunction of important disorders, e.g. autoimmune hepatitis, Wilson's disease
Understand the anatomical, physiological and hormonal changes in the liver that occur throughout childhood
Understand the physiological basis of normal liver function, including absorption and secretion
Know the genetic and environmental factors in the aetiology of liver disease
Understand the pathophysiology of infective agents in the liver
Understand the pharmacological basis of therapy in liver disorders
Know the possible impact on the hepatobiliary system of other system disorders and vice versa
The aetiology of liver disease varies according to age. In neonates, infective, genetic and metabolic causes are the most common. As the child gets older, autoimmune/infective causes predominate.
The liver is the largest intra-abdominal organ, with synthetic, metabolic, exocrine and endocrine functions. Liver development occurs through a progressive series of reciprocal tissue interactions between the embryonic endoderm and mesoderm. Application of this knowledge has allowed production of ‘hepatic-like’ tissue from embryonic stem cells, which may ultimately lead to their use in transplantation.
During gastrulation, a process which takes place in all animals, where the single layered blastula becomes a tri-layered gastrula comprising endoderm, ectoderm and mesoderm, the endoderm layer forms and leads to a primitive gut tubular structure comprising foregut, midgut and hindgut regions ( Fig. 21.1 ).
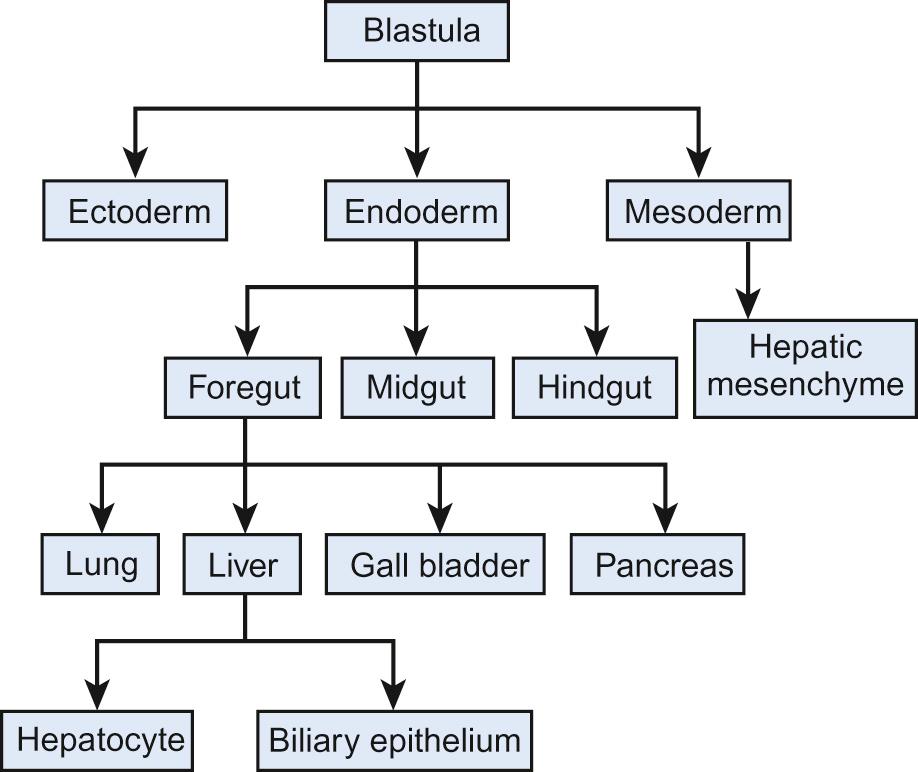
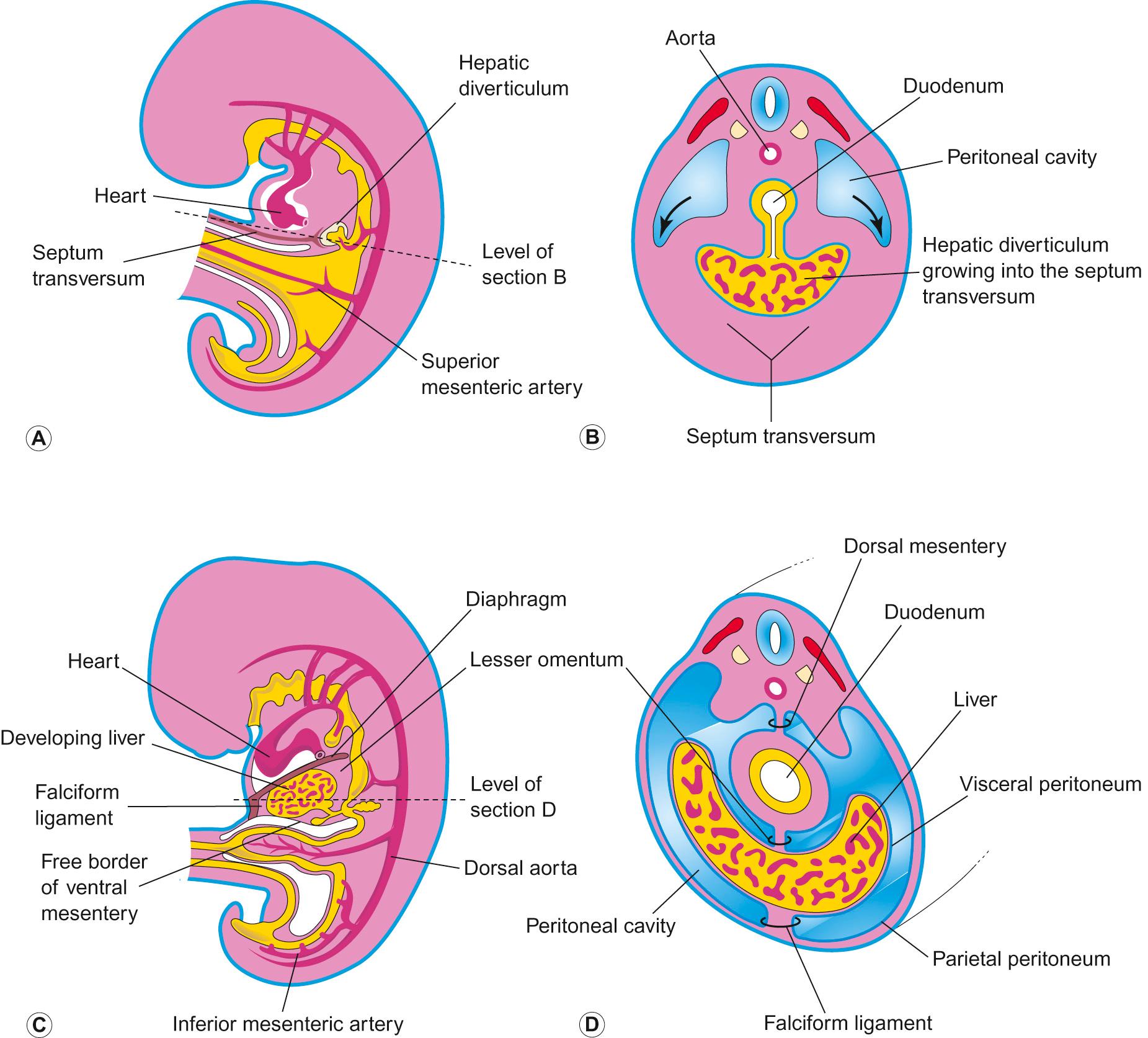
The liver originates from the ventral foregut. The first sign is formation of the hepatic diverticulum adjacent to the developing heart ( Fig. 21.2 ). Anteriorly it becomes the liver and intrahepatic biliary tree. Posteriorly it forms the gall bladder and extrahepatic bile ducts. Hepatoblasts invade the septum transversum, forming the liver bud. This undergoes accelerated growth as it is vascularized and colonized by haematopoietic cells, becoming the major fetal haematopoietic organ. Hepatoblasts are bi-potential, becoming either the lumen of the intrahepatic bile ducts or differentiating into hepatocytes. Between antenatal day 17 and into the perinatal period, focal dilations appear forming intrahepatic bile ducts, while the remainder regress.
Defects in early liver bud growth can be lethal. The molecular genetics of Alagille syndrome exemplify the interaction between endoderm and mesenchyme (see also Table 21.2 ). Mutations in the Notch ligand gene Jagged-1 leads to a paucity of intrahepatic bile ducts. Jagged-1 expressed in the portal mesenchyme activates NOTCH-2 in adjacent hepatoblast, required to maintain bile duct morphogenesis.
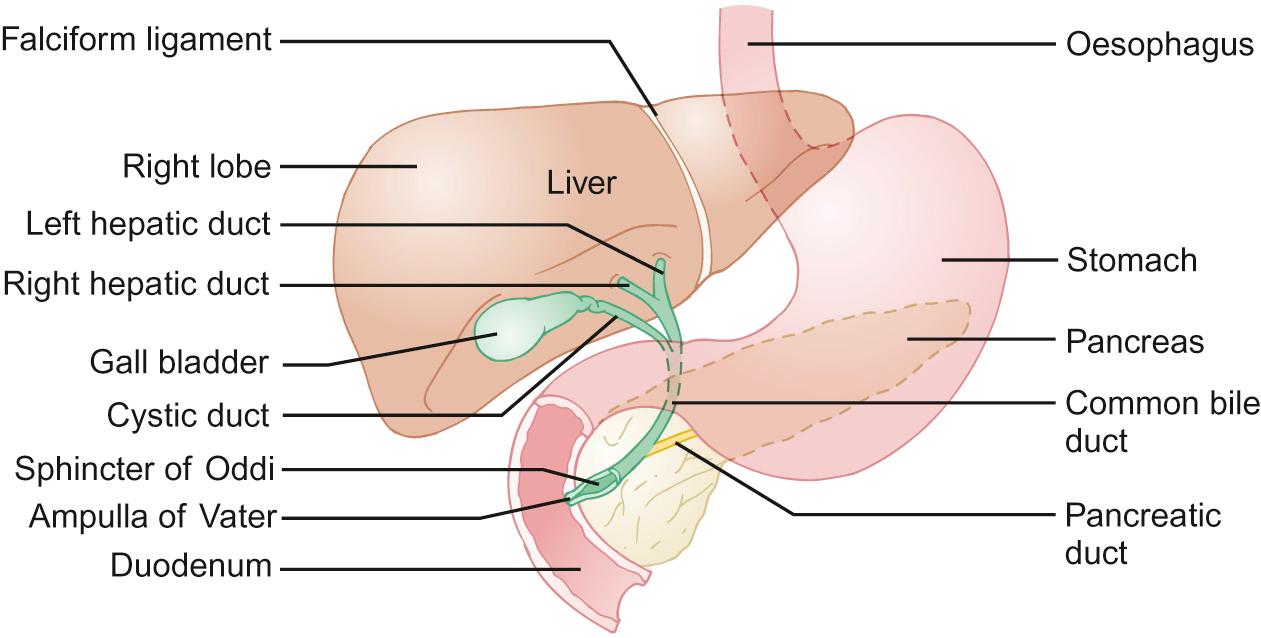
The falciform ligament divides the liver anteriorly; the round ligament and umbilical fissure inferiorly. The right lobe is further divided by the gall bladder fossa into the right hemiliver and quadrate lobe. The fourth lobe (caudate) is posterior and surrounds the inferior vena cava. The biliary tree connects the liver and duodenum, the primary purpose being bile transport and storage, under neuronal and hormonal regulation. Bile is formed in hepatocytes, and is transported into the extrahepatic ducts via the cannaliculi. Bile flows into the small intestine or into the cystic duct and then into the gall bladder, regulated by the sphincter of Oddi ( Fig. 21.3 ).
The arterial supply to the liver in utero is the left hepatic artery derived from the left gastric artery; the middle hepatic artery (common hepatic artery) derived from the coeliac trunk; and the right hepatic artery derived from the superior mesenteric artery. The blood supply assumes the adult pattern during early infancy, with atrophy of right and left hepatic arteries.
Concerning bile and the biliary tract, which of the following statements are true (T) and which are false (F)?
Bile is essential for the effective absorption of dietary fat
Bile is normally secreted into the jejunum and absorbed in the caecum
Bile is rich in copper
The absence of bile leads to dark, tarry stools
The gall bladder is easier to visualize on ultrasound scan in a starved patient
A. True; B. False; C. True; D. False; E. True.
See below for discussion.
Gut bile allows absorption of fat and excretion of cholesterol, bilirubin, iron and copper. Bile is secreted by the hepatocytes into the canalicular space by active and passive processes. It is the active process which generates bile flow. The products of active secretion comprise conjugated bile acids, conjugated bilirubin, glutathione, conjugates of steroid hormones and leukotrienes. Filterable solutes (plasma, glucose, electrolytes, low-molecular-weight organic acids and calcium) are generated by passive secretion induced by osmotic pressure and are called secondary solutes.
Between meals, the gall bladder relaxes and the sphincter of Oddi contracts, leading to the diversion of hepatic bile into the gall bladder for storage until the next meal (this observation becomes important when assessing a child with conjugated jaundice in whom you suspect biliary atresia, as a fasted ultrasound scan will fail to demonstrate a gall bladder). During a meal, the gall bladder contracts, the sphincter of Oddi relaxes and bile enters the duodenum. Bile acids are absorbed from the terminal ileum and return to the liver via the portal system. This is a process of both passive and active reabsorption. The most important mechanism is a sodium-coupled transporter present in the apical membrane of the enterocytes; the ileal bile acid transporter. In the distal ileum and large intestine, intestinal bacteria deconjugate bile acids, which are absorbed passively. A small amount of the bile acid is lost in the faeces.
In order to understand liver disease, it is necessary to understand how the liver regulates a number of important processes ( Table 21.1 ).
A 4-week-old baby girl is referred to the paediatric department for review of prolonged jaundice. The blood test results are as follows: Hb 142 g/L, WCC 9.8 × 10 9 /L, Plt 521 × 10 9 /L, total serum bilirubin 109 mmol/L, conjugated bilirubin 9 mmol/L, AST 42 µmol/L, ALT 19 µmol/L, GGT 32 µmol/L, alkaline phosphatase 1345 µmol/L. What do these results suggest? Select ONE answer only.
Biliary stasis
Mild hepatic necrosis
Possible biliary atresia and should be admitted for further imaging
Rapid bone growth of infancy
Vitamin D deficiency – this baby should be screened for possible rickets
D. Rapid bone growth of infancy.
This question demonstrates that, although commonly considered a ‘liver enzyme’, alkaline phosphatase is also produced during rapid bone growth – and can often be raised during so-called growth spurts.
| Function | Effect of dysfunction | Assessment |
|---|---|---|
| Metabolism/storage | ||
| Carbohydrate/glycogen | Loss of glucose homeostasis | Hypoglycaemia on fasting |
| Lipid | Lipid accumulation | Dyslipidemia |
| Reduced oxidation of fatty acids | Raised lactate Increased ratio free fatty acid : beta-hydroxybutyrate Increased acyl carnitine Organic aciduria |
|
| Protein | Increased catabolism | Low branch chain amino acids, urea |
| Hyperammonaemia Raised tyrosine, phenylalanine, methionine |
||
| Synthesis | ||
| Albumin Factors II, VII, IX, X |
Loss of muscle mass Coagulopathy |
Low albumin; protein energy malnutrition Prolonged PT/PTT |
| Degradation | ||
| Drugs | Prolonged drug effect, e.g. sedation | Clinical |
| Oestrogens Toxic products |
Telangiectasia; gynaecomastia. Encephalopathy |
Clinical Abnormal EEG |
| Bile synthesis and excretion | Cholestasis | Conjugated hyperbilirubinaemia, raised LFTs |
| Fat malabsorption Fat-soluble vitamin deficiency |
Hypercholesterolaemia | |
| Pruritus | ||
| Malnutrition | Anthropometry | |
Bilirubin, in particular conjugated (direct) bilirubin, is almost always raised in liver disease irrespective of its cause. It is produced from the breakdown of red blood cells, making unconjugated (indirect) bilirubin, which circulates bound to albumin although some is ‘free’ and hence able to enter the brain. Unconjugated bilirubin is metabolized in the liver to produce conjugated bilirubin which passes into the gut and is excreted in stool.
Transaminases are present in the liver, heart and skeletal muscle. They indicate the nature of liver dysfunction when taken in combination with a background history, e.g. raised alanine aminotransferase (ALT) and aspartate aminotransferase (AST) indicate hepatic necrosis and are indicators of hepatic damage. Alkaline phosphatase, although raised in liver disease, particularly biliary disease, can also be raised in rapid bone growth or secondary to vitamin D deficiency. Gamma-glutamyl transferase (GGT) is particularly associated with biliary obstruction and inflammation.
Assessment of liver synthetic function is useful when assessing liver disease. Albumin and coagulation are sensitive markers of liver dysfunction. Hypoglycaemia is a common finding in liver dysfunction.
Radiological investigations such as an ultrasound scan can give valuable information about the liver's architecture, such as the shrunken cirrhotic liver with heterogeneous appearance often seen in chronic liver disease, or the enlarged liver seen in some metabolic diseases such as glycogen storage disease type I. Developmental defects can be seen on fasting ultrasound scan, such as extrahepatic biliary atresia, where a gall bladder is not demonstrable after a fast (this is abnormal and must always be discussed with a tertiary centre). The other developmental defect commonly seen on ultrasound scan is a choledochal cyst (an outpouching of the bile ducts). Surgical correction is necessary as these can result in malignancy. Gallstones can be easily demonstrated on ultrasound scan as well as any ductal dilatation. It is also possible to assess the liver's blood supply, valuable in children who have liver disease or who have had a liver transplant, as vessel thrombosis or reversed vessel flow requires immediate assessment and management and is a poor prognostic sign. Other abdominal structures can be assessed, e.g. splenic enlargement associated with portal hypertension – a sequelae of chronic liver disease. The spleen is enlarged due to increased blood flow as a result of a stiffened cirrhotic liver (which is resistant to flow and therefore the blood takes the path of least resistance – see discussion below).
Jaundice in the neonatal period is common. About two-thirds of term babies have transient jaundice 3–5 days after birth. Most do not have liver disease. Unconjugated jaundice is often due to immaturity of the hepatic enzyme glucuronosyltransferase, responsible for glucuronidation of bilirubin. Unconjugated jaundice in the neonatal period may be due to ‘breastmilk jaundice’. Other causes include haemolysis, sepsis and hypothyroidism. This is considered in detail in Chapter 11 , Neonatal medicine. In contrast to this, conjugated hyperbilirubinaemia is often a reflection of hepatic dysfunction due to a number of potential causes, including biliary atresia or neonatal hepatitis syndrome.
Babies with significant liver problems usually have significant jaundice. Under these circumstances, the bilirubin level should be measured together with the fractional breakdown of the conjugated and unconjugated components. This will help to guide further investigation and management.
Crigler–Najjar syndrome types I and II are rare autosomal recessive disorders which cause intense unconjugated hyperbilirubinaemia in the first days of life, which persists thereafter. In type I, there is no UDP-glucuronosyltransferase. Hyperbilirubinaemia is very severe despite phototherapy and may result in kernicterus. Diagnosis is made by DNA analysis. In type I, there is no response to treatment with phenobarbital, which causes cytochrome P450 enzyme induction. Acute treatment is with exchange transfusion and liver transplantation is a long-term option. In type II, some UDP-glucuronosyltransferase is present, so hyperbilirubinaemia is less severe. Phenobarbital therapy is effective, generally with a marked decrease in serum bilirubin. Therapies based on gene and cell transfer techniques are likely to be helpful in the future.
A six-week-old male baby is referred to the general paediatric clinic as a ‘hungry baby who cries all the time’. Upon review, the baby is alarmingly malnourished and jaundiced. The stool is white ( Fig. 21.4 ) and urine dark orange. Which of the following is most likely to BEST describe the physiology underpinning the pale stool? Select ONE answer only. The stool is pale because it is lacking in:
Caesin
Hemosiderin
Ligandin
Lipase
Stercobilin
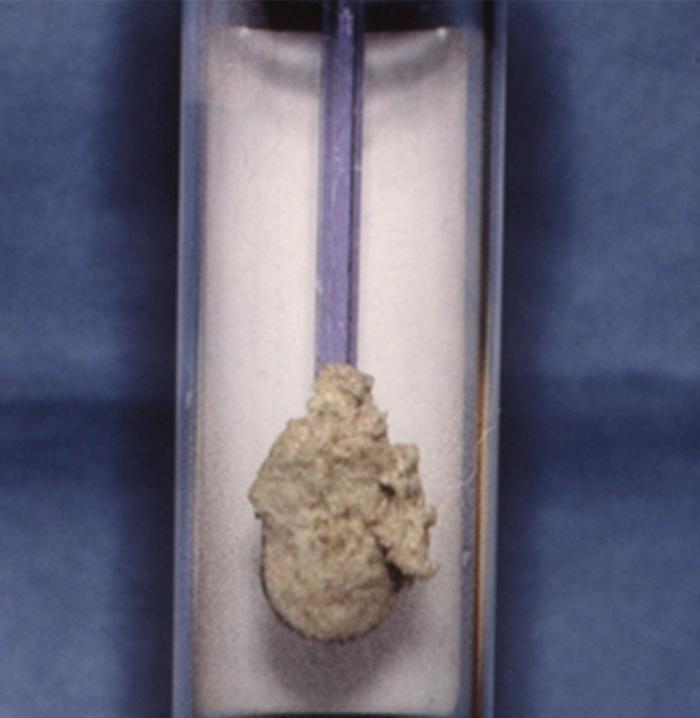
E. Stercobilin.
In order for bile to enter the stool it has to be conjugated, making bilirubin water soluble and easier to excrete. Once in the gut, conjugated bilirubin is either hydrolyzed and reduced by bacteria to form urobilinogen (which is colourless) or reabsorbed via the enterohepatic circulation. Most urobilinogen is eventually oxidized by intestinal bacteria to stercobilin in stool, which gives its brown colour. If conjugated bilirubin fails to be excreted into the gut, the stools will be pale.
In biliary obstruction, the amount of urobilinogen in the gut is reduced, so the urobilin in the urine is low. However, there is increased soluble conjugated bilirubin in the circulation which is excreted via the kidneys and results in the urine's dark colour.
In normal circumstances, only a small fraction of bilirubin is conjugated. In neonates, conjugated hyperbilirubinaemia is defined as a serum conjugated bilirubin of greater than 25% of the total (current BSPGHAN guideline) or >25 µmol/L (NICE guidelines). This most commonly occurs when there is cholestasis. With neonatal cholestasis, there is impairment of bile excretion caused by defects in intrahepatic production or transmembrane transport of bile, or mechanical obstruction to bile flow. The biochemical features of cholestasis reflect the retention of components of bile in the serum (bilirubin, bile acids, and/or cholesterol). The pattern and severity of each of these abnormalities varies with the underlying disorder.
Classically, patients present with jaundice, pale (acholic) stool and dark urine. Pale stools occur as no bilirubin reaches the gastrointestinal tract and dark urine results from excretion of water-soluble conjugated bilirubin in the urine. Both of these features suggest cholestasis.
Biliary atresia is the commonest cause of neonatal liver disease and indication for liver transplantation in children. It occurs in 1 : 17,000 live births. It presents with conjugated jaundice, acholic stools and hepatomegaly. There is failure of passage of bile from the liver into the gall bladder and onto the small intestine. Bile is essential for carrying waste from the liver and promoting absorption of fats and fat-soluble vitamins. Biliary atresia results in chronic liver failure if surgical correction is not performed. The Kasai portoenterostomy attempts to allow diversion of bile from the residual small bile ducts. The surgery involves attaching the porta hepatis to a loop of small intestine. Up to 60% will achieve biliary drainage (bilirubin <20 µmol/L) within 6 months. Most of these children will reach adolescence with a good quality of life (but with cirrhosis/evidence of portal hypertension) without undergoing liver transplantation.
Olivia is a 4-week-old infant referred to a tertiary centre due to prolonged jaundice. She is thriving, but noticed to have very pale chalky white stools. Her urine is dark in colour. Baseline blood investigations revealed mildly raised transaminases. Her total bilirubin concentration was 220 µmol/L, with a conjugated fraction of 185 µmol/L. A fasting ultrasound scan was organized which demonstrated a completely contracted gall bladder despite adequate 4-hour fast. TIBIDA scan was also performed which showed no excretion of technetium even after a prolonged exposure (>24 hours). Olivia underwent Kasai procedure at 5 weeks of age and by 3 months of age her bilirubin had reduced to normal range (bilirubin concentration <20 µmol/L). She will be followed up long term for any signs of chronic liver disease, including portal hypertension.
Where is the initial underlying defect MOST likely to occur? Select ONE answer only.
Extrahepatic biliary tree
Exocrine pancreas
Gall bladder
Intrahepatic biliary tree
Jejunum
If her Kasai operation ‘failed’, she would develop rising bilirubin, abdominal distension due to ascites and faltering growth from chronic liver disease. Why would she develop faltering growth? From the following list, which of the statements are true (T) and which are false (F)?
She has a chronic health problem and is likely to suffer from neglect from carers
Her metabolic rate is markedly increased
Lack of gut bile decreases the absorption of fat and fat-soluble vitamins
The growth failure is secondary to adrenal suppression
The main cause is likely to be corticosteroid therapy
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here