Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Hemorrhoids have been referenced in ancient texts dating back 4000 years. Included in many of these Egyptian and Greek writings are multiple recommended treatment regimens including anal dilation, topical ointments, and the intimidating red hot poker. Although few people have died of hemorrhoidal disease, many patients wish they had, particularly after therapy, and this fact led to the sanctification of St. Fiachre, the patron saint of gardeners and hemorrhoidal sufferers. This discussion will guide the practitioner in a more humane approach to hemorrhoidal disease, with the emphasis on cost-effectiveness with minimal morbidity and mortality.
Hemorrhoids are normal vascular cushions suspended in the submucosal layer of the anal canal by longitudinal connective tissue and muscle fibers. Internal hemorrhoids originate above the dentate line, while external hemorrhoids occur below this level. Mixed component hemorrhoids can occur above and below the dentate line. These vascular cushions appear predictably in the right anterior, right posterior, and left lateral positions, although there may be intervening secondary hemorrhoidal complexes that blur this classic anatomy. Their blood supply is derived from the superior rectal artery via the inferior mesenteric, the middle rectal arteries via the internal iliac arteries, and the inferior rectal arteries via the pudendal arteries that derive flow from the external iliac arteries. The venous drainage transitions from the portal venous system above the level of the dentate line to the systemic venous system below this level. The columnar epithelium of internal hemorrhoids is viscerally innervated and therefore not sensitive to pain, touch, or temperature. On the other hand, external hemorrhoids are covered by squamous epithelium anoderm, which contains an abundance of somatic pain fibers, making thrombosed external hemorrhoids extremely painful and sensitive.
The pathogenesis of symptomatic hemorrhoids is most likely due to the weakening of the connective tissue within these vascular cushions which produces bleeding, with or without prolapsing of the hemorrhoidal tissue. These symptoms occur as a result of low-fiber dietary intake, excessive straining, chronic constipation, prolonged sitting, pregnancy, advanced age, and in patients on anticoagulation or antiplatelet therapy. Many factors contribute to symptomatic hemorrhoids such as deterioration of the anchoring connective tissue that occurs with advanced age. Internal anal sphincter dysfunction may also play a role in the development of hemorrhoidal disease, and a number of investigators have demonstrated increased internal anal sphincter tone in patients with hemorrhoidal disease. Abnormal distention or dilation of the arteriovenous formations within the hemorrhoid plexus may also play a role, although it is unclear whether this association is causal or a result of constipation and straining.
The standard classification for hemorrhoidal diseases is as follows:
Grade I, visualized on anoscopy and may bulge into the lumen but do not prolapse below the dentate line, bleed during defecation
Grade II, prolapse out of the anal canal with defecation or with straining but reduce spontaneously, bleed and secrete mucus
Grade III, prolapse requiring manual reduction
Grade IV, prolapse that cannot be manually reduced, generally mixed hemorrhoids that include internal and external components
Although this staging system tends to correlate with patients' symptoms, it is unclear that it can be completely relied on when making therapeutic decisions. Alternative anorectal pathology must be considered, such as mucosal prolapse or skin tags, to produce the symptoms.
Only 30% of patients seen for “hemorrhoids” will actually have true hemorrhoidal disease. Bleeding, protrusion, and pain are among the most common symptoms associated with hemorrhoidal disease. Hemorrhoidal bleeding from internal hemorrhoids typically results in bright red blood either on the toilet paper or may drip into the toilet at the end of defecation and is generally painless in nature. More vigorous bleeding can occur as the hemorrhoids enlarge and the hemorrhoidal complex becomes displaced and is fixed externally, allowing the blood to drip or spurt into the toilet. Patients with grade III or IV internal hemorrhoids may also complain of a sensation of fullness, fecal incontinence, and constant mucous discharge. Usually, prompt reduction of the protruding mass causes this symptom to abate. Acute thrombosed internal or external hemorrhoids are usually associated with severe pain and a palpable perianal mass or lump. These patients are generally quite uncomfortable, and the diagnosis is immediately obvious on clinical examination.
Examination of the patient with hematochezia, although tailored by the age of the patient, should include sufficient investigations to rule out a proximal source of bleeding such as inflammatory bowel disease and neoplasia. Other anorectal pathologies should also be considered as sources of pain, such as fissures, fistulas, abscesses, or neoplasm. We prefer to examine the patient in the prone jackknife position using the proctology table. This approach allows relative patient comfort and the ability to clearly inspect the perianal skin and perform anoscopy and proctosigmoidoscopy. Digital rectal examination should be performed at rest and with straining and should include palpation for masses, fluctuance, tenderness, and characterization of anal sphincter tone. Internal hemorrhoids are generally not palpable on digital examination in the absence of thrombosis. In addition, a thrombosed hemorrhoid is extremely tender to palpation, and a thrombus may be palpable within the hemorrhoid. The presence of thickening or scar in the posterior midline or roughening of the otherwise smooth anoderm is suggestive of a partially healed anal fissure. Hypertrophic, edematous eccentrically placed, and tender skin tags should raise suspicion for the underlying Crohn disease. An assessment of the sphincter tone and history of fecal incontinence should also be obtained, as this information may alter your surgical planning. In contrast, in the absence of a thrombosed external hemorrhoid, an anoscopy should be performed to evaluate the anal canal and the distal rectum. Internal hemorrhoidal bundles appear as bulging purplish-blue veins, and prolapsed internal hemorrhoids appear as dark pink, glistening, and sometimes tender masses at the anal margin. Thrombosed external hemorrhoids are acutely tender and have a purplish hue. Anoscopy has the advantage of being a quick, relatively painless, inexpensive procedure that can be performed in an unprepped patient to diagnose hemorrhoids and exclude other distal anorectal disorders.
If hemorrhoids or other pathology is not found, a colonoscopy should be done regardless of age, to rule other pathologic sources for the rectal bleeding. While performing a colonoscopy or flexible sigmoidoscopy, the distal rectum and anal verge should be inspected in retroflexion with the rectum partially insufflated. Complete insufflation should be avoided, as this causes the rectal vault to distend and stretch, thereby flattening internal hemorrhoids.
The initial and most efficacious nonoperative treatment for hemorrhoidal disease is implementation of fiber and increased liquid intake. A systematic review and meta-analysis showed significant resolution of hemorrhoidal symptoms by more than 50% at 6 weeks and incrementally more at 3 months. Further randomized controlled trials of 20 g of psyllium/day versus placebo showed symptomatic relief in 84% versus 54% of the patients. Patients should also be advised to implement other lifestyle modifications such as avoiding prolonged sitting or straining on the toilet, perianal hygiene, and avoiding foods or other triggers for constipation. The main goal of nonoperative treatment is to reverse the pathology of hemorrhoidal disease and to provide symptomatic relief. The downside of nonoperative therapy is that it may take several weeks to manifest and requires a great deal of patience and compliance.
Various topical agents propose to reduce hemorrhoidal symptoms, but in reality, these agents are aimed at providing symptomatic relief rather than altering the pathophysiology of hemorrhoidal disease. These preparations include local anesthetics, vasoactive agents, and corticosteroids. Although these treatments are plentiful, randomized controlled trials regarding their efficacy in comparison to other modalities are sparse.
Several office procedures are now commonly used in the management of symptomatic hemorrhoidal disease. Modalities include infrared coagulation, sclerotherapy, and rubber band ligation. Other novel techniques are constantly being introduced and evolving, but they are at their infancy and studies are lacking to reinforce their efficacy. The underlying mechanisms in all these techniques rely on tissue destruction and/or fixation.
The use of sclerotherapy to treat symptomatic internal hemorrhoidal disease was first advocated by Mitchell in 1871 and typically involves injecting a sclerosing agent into the submucosa, resulting in atrophy of the tissue and scarification with fixation of the hemorrhoidal complex within its normal location in the anal canal. A variety of injecting solutions have been advocated, although it appears that sodium morrhuate and sodium tetradecyl sulfate currently predominate. This modality is most effective in situations with minimal enlargement of hemorrhoidal complexes where the primary complaint is bright red rectal bleeding.
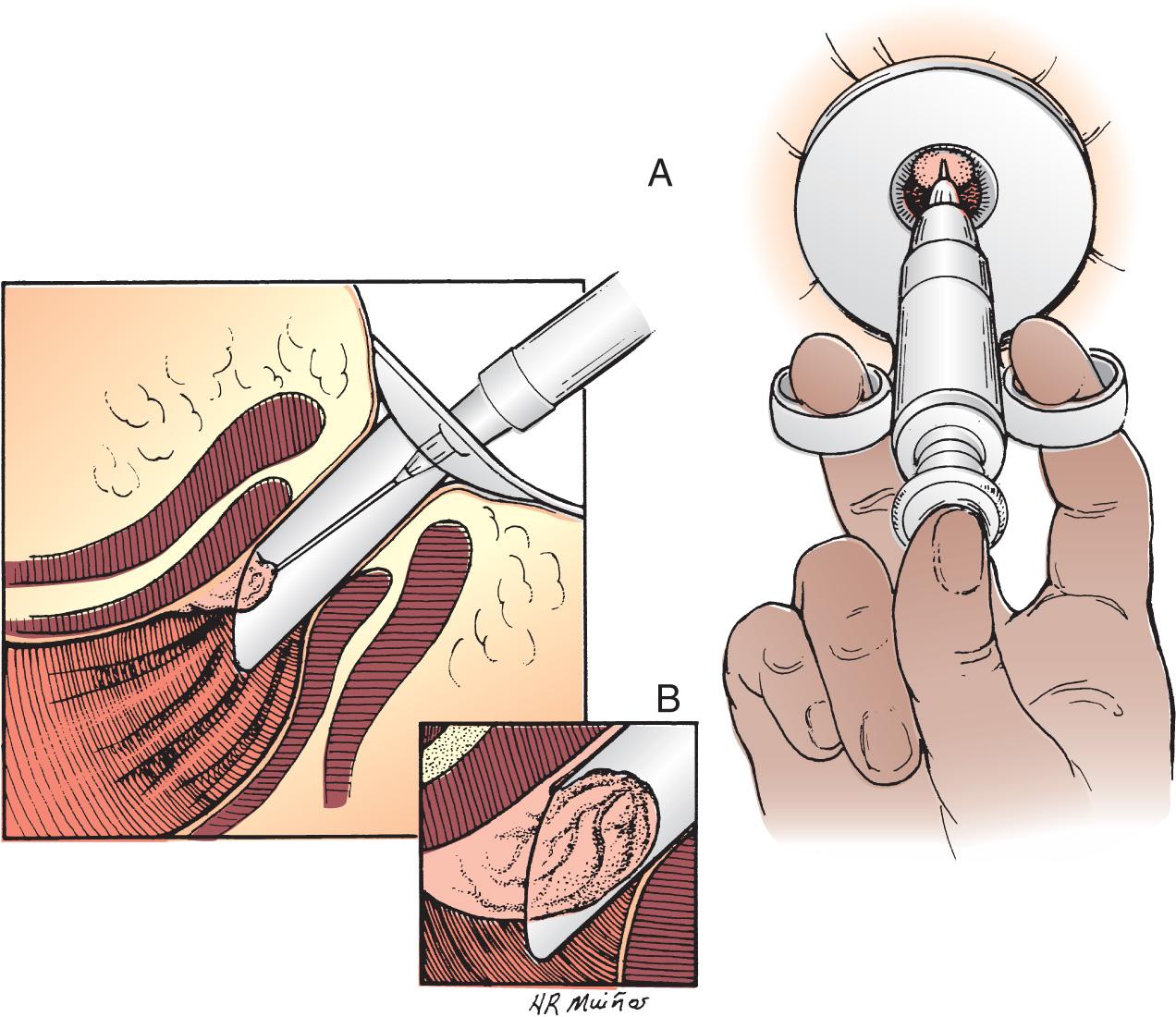
The procedure is performed with the patient in the left lateral decubitus or prone jackknife position. An anoscope is inserted to clearly identify the hemorrhoid complex and a 25-gauge spinal needle is used to instill the sclerosant into the submucosal space ( Fig. 158.1 ). The syringe should be aspirated before injection to avoid a direct intravascular injection. Typically, 3 to 5 mL of sclerosant is adequate. The surgeon can inject as many locations as desired, because the procedure is essentially painless. It is important, however, not to circumferentially inject the anal canal, because this may induce stricture formation. Other described complications, although rare, include bacteremia, pelvic sepsis, prostatic abscesses, creation of rectourethral fistulas, rectal perforations, and necrotizing fasciitis. Success rates of 75% to 89% have been reported in patients with grades I to III disease. However, longer follow-up intervals often demonstrate a relatively higher rate of symptomatic recurrence. The ideal candidates may be patients with bleeding tendencies or those on antiplatelet or anticoagulation therapy, since this provides a less invasive and perhaps less bloody alternative to excisional hemorrhoidectomy.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here