Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Central venous catheters play an important role in the treatment of patients with end-stage renal disease. Despite initiatives to improve fistula creation, more than 80% of patients initiated hemodialysis with a catheter, a number that has changed little over the past 15 years. Central venous catheters for hemodialysis are categorized by their intended duration as either acute or chronic. Both acute and chronic hemodialysis catheters can be placed percutaneously; however, chronic catheters feature a subcutaneous retention cuff near the skin exit site, whereas acute catheters do not. This cuff serves to provide a point for tissue ingrowth, ensuring that the catheter remains in place, and also acts as a barrier to prevent microbial migration into deeper tissues. As a result, acute catheters are at higher risk for infectious complications and can easily become dislodged. Thus acute catheters should be placed only in hospitalized patients and used for a short duration, usually less than 2 weeks. This time frame is in contrast to chronic catheters, which can be used in the outpatient setting indefinitely.
This chapter focuses on tunneled dialysis catheters (TDC) and their management, but the potential complications related to placement of acute nontunneled hemodialysis catheters mirror those of TDC. However, because of the short duration of use of acute catheters, long-term complications are less frequent but infectious complications are more common.
The most common indication for placement of a tunneled hemodialysis catheter is for urgent hemodialysis while the patient is waiting for an autogenous arteriovenous fistula (AVF) or arteriovenous graft (AVG) to be created or to mature. Other indications include patients in whom an AVF or AVG is not anatomically feasible or who are not operative candidates because of advanced comorbidities. Temporary TDC placement is also indicated after revision of an AVF or AVG for management of a complication (e.g., access revision for pseudoaneurysm formation or infection), after placement of a peritoneal dialysis catheter, and for a chronic ambulatory peritoneal dialysis patient requiring abdominal or inguinal surgery.
The benefits of TDC over AVF and AVG include immediate use for hemodialysis, uncomplicated and needle-free connection to the dialysis circuit, elimination of cannulation site complications, and simple insertion technique that can be performed by many different interventional specialists. While a mature and well-functioning AVF or AVG is preferred to TDC, recent guidelines recognize that in certain cases, creation of a functional AV access is severely challenged due to anatomic limitations. In these circumstances, a TDC can be considered for long-term or indefinite use.
Early cuffed catheters were straight in configuration and stiff. With technological advances, these catheter designs have been largely supplanted by flexible catheters with various tip designs.
Catheter designs aim to achieve one main goal: adequate dialysis clearance at a relatively high flow rate of 300 to 350 mL/min. In addition, the phenomenon of recirculation must be minimized to ensure adequate clearance. The “arterial lumen” of the catheter is the outflow to the dialysis machine from the patient; the “venous lumen” is defined as the inflow from the machine back to the patient. Access recirculation is the reentry of dialyzed blood from the venous lumen directly into the arterial lumen, thus bypassing the systemic circulation and leading to inefficient dialysis, lack of appropriate solute clearance, and possibly increased morbidity and mortality.
Numerous manufacturer modifications exist in an effort to satisfy the requirements of high flow rates and minimal recirculation. The modifications fall into four general categories.
Split-tip catheters have a double-lumen, single-body configuration in the midbody but separate into two distinct distal tips, each with side holes in all directions ( Fig. 176.1A ).
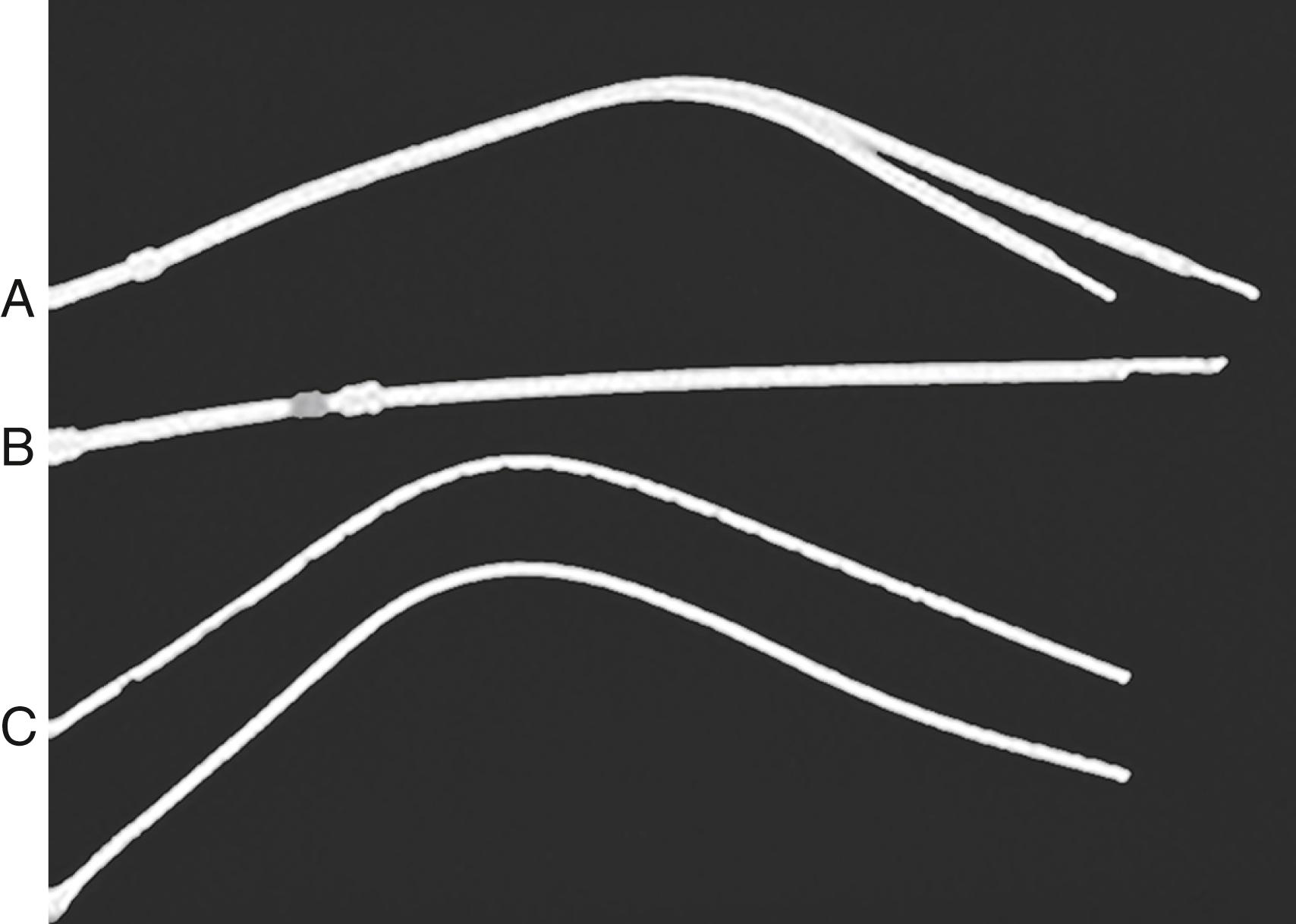
The staggered-tip or step-tip catheter is a double-lumen, single-body catheter with the venous limb extending at least 2.5 cm beyond the inflow tip (see Fig. 176.1B ).
The dual catheter design consists of two completely separate catheters that can be inserted in two different locations (see Fig. 176.1C ).
Symmetric tip catheters have equal length of arterial and venous limbs ( Fig. 176.2 ).

Numerous reviews directly compare performance of individual tunneled hemodialysis catheters with specific outcome variables of flow rate, recirculation time, and patency. Unfortunately, despite isolated beneficial characteristics of a particular catheter design, no particular catheter has been demonstrated to be superior over others. , , , A systematic review of catheter tip designs that included seven randomized controlled trials and one retrospective study and encompassed 988 patients demonstrated no advantage of a particular catheter design.
As with any clinical assessment, the proper preoperative evaluation of a patient begins with a detailed history and physical examination. Specific inquiries should include details such as prior long-term central line placement, prior AVF or AVG placement, prior tunneled hemodialysis catheter infections, history of a coagulation disorder, and history of a pacemaker. Physical examination of the neck and chest is mandatory. Evidence of a previously placed tunneled hemodialysis catheter, previous permanent accesses, upper extremity or facial edema, and ipsilateral venous distention with visible venous collaterals should alert the clinician to the possibility of central veno-occlusive disease.
Numerous specialists have the skill set to properly place a tunneled hemodialysis catheter. However, there is a significant advantage in terms of continuity of care when the same practitioner places the tunneled hemodialysis catheter and the permanent access or when a team approach coordinates these procedures. There are a finite number of access sites available for both tunneled catheter and permanent access placement. Therefore, a comprehensive plan that embraces all forms of hemodialysis access may provide maximum benefit of each crucial access site.
Noninvasive color-flow duplex imaging is the first-line method of preoperative imaging for the tunneled hemodialysis catheter. Patency of internal jugular veins and axillary veins is easily identified with compression of the vein. However, as imaging moves toward the central chest, the air interface with the lung tissue, as well as obstructing bone structures, makes subclavian vein and central vein imaging virtually impossible.
Three-dimensional gadolinium-enhanced magnetic resonance venography (MRV) has been shown to be highly sensitive in identifying central vein occlusions and stenoses greater than 50% when directly compared with digital subtraction angiography. Despite the accuracy of MRV, gadolinium must be administered with caution in patients with a glomerular filtration rate of less than 30 mL/min because of the risk of gadolinium-induced nephrogenic systemic fibrosis, which is rare even in this patient population, but has not been described in patients with normal renal function. An alternative to gadolinium is ferumoxytol, an ultrasmall, superparamagnetic iron oxide nanoparticle. Ferumoxytol is approved for a variety of magnetic resonance imaging applications, does not carry the risk of nephrogenic systemic fibrosis and results in accurate and reliable MRV images.
Computed tomographic venography (CTV) is similar to MRV in being able to image multiple vessels in the chest in one setting. However, CTV does have the advantages of being readily available in most medical centers, fast acquisition times, and fewer deleterious contrast agent concerns. Contrast-enhanced CTV provides excellent imaging of the superior vena cava and a study of 18 patients comparing CTV and digital subtraction venography for the diagnosis of benign thoracic central venous obstruction demonstrated that CTV findings correlated closely with those of digital subtraction venography.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here