Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The incidence of sports- and recreation-related traumatic brain injuries (TBIs) has continued to increase during the past decade. The two most common athletic activities associated with emergency department treatment for TBI are bicycling and football. Risk for TBI is inherent to participation in sports and recreation activities, and compared with adults, children and adolescents have an increased risk for TBIs, with increased severity and prolonged recovery. TBI is a term that encompasses a broad range of head injuries and includes concussion, skull fracture, epidural hematoma, subdural hematoma, intracerebral hematoma, and subarachnoid hemorrhage.
Concussion is defined as a complex, transient, pathophysiologic process that affects the brain and is induced by traumatic biomechanical forces. Concussions occur with rapid onset and involve short-lived neurologic impairment that typically resolves spontaneously. Acute clinical presentation reflects a functional disturbance rather than structural injury. Injury occurs on a biochemical level without significant detectable gross anatomic changes, which supports the understanding that the changes are based on temporary neuronal dysfunction, not cell death. Biochemical neuronal dysfunction occurs as a result of a combination of shifts in ion balance, altered glucose metabolism, impaired connectivity, and changes in neurotransmission. This biochemical dysfunction presents clinically in patients with a constellation of symptoms that may include any combination of one of more of the following: headache, dizziness, confusion, disorientation, hearing/visual disturbances, and/or loss of consciousness. It is important to understand that this range of clinical symptoms may or may not involve loss of consciousness. Historically, athletes referred to concussive episodes as a “ding” or “getting your bell rung”; these terms may describe the disorientation experienced by the athletes and are suspicious, if not defining, for a concussive injury. Results of neuroimaging studies (i.e., skull radiographs and head computed tomography [CT] or magnetic resonance imaging [MRI]) are typically normal, further supporting the understanding that concussion is a functional disturbance without true gross structural abnormality.
When rotational or angular acceleration forces are applied to the brain, a shear strain occurs on the neural elements, leading to a neurometabolic cascade and the clinical features of concussion. The biomechanical injury to the brain causes an immediate release of excitatory neurotransmitters ( Fig. 139.1 ).
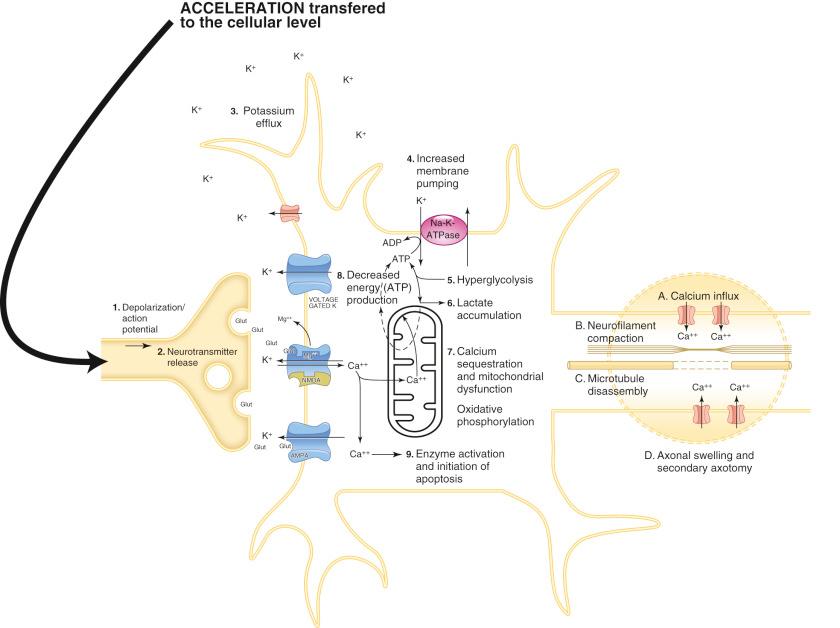
The binding of the excitatory neurotransmitters, such as glutamate, lead to further neuronal depolarization with further destabilization of the ionic equilibrium, including influx of calcium and efflux of potassium ( Fig. 139.2 ).
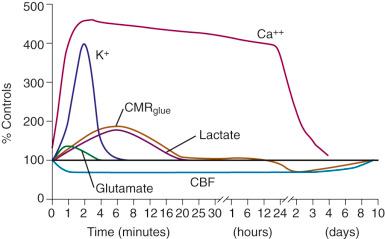
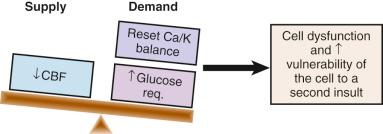
To restore the ionic homeostasis, neuronal membrane potential energy (adenosine triphosphate) is required to enable operation of the sodium-potassium pump. This increased glucose demand (“hypermetabolism”) occurs in the face of decreased cerebral blood flow. Metabolic supply/demand mismatch leads to cell dysfunction and increased vulnerability of the cell to a second insult ( Fig. 139.3 ).
After the initial period of “hypermetabolism,” a period of decreased metabolism occurs in the concussed brain. Calcium levels may remain elevated and impair mitochondrial oxidative metabolism, further worsening the energy deficits. In addition, neurofilament and microtubule function is disrupted by intra-axonal calcium flux, impairing posttraumatic neural connectivity.
On average, these biochemical changes take 7 to 10 days to normalize in adults (see Fig. 139.2 ), but normalization can take longer in the growing brain of a child and adolescent. Interestingly, the clinical recovery parallels this biochemical normalization. Changes in cerebral blood flow may also occur with concomitant impairment of vascular autoregulation, which can result in cerebral edema and may persist beyond the acute phase.
Twenty-one percent of all TBIs among children in the United States are associated with sports participation. Although death from a sports injury is rare, the leading cause of death from a sports-related injury is a brain injury. Football, gymnastics, and ice hockey reported the highest number of sports-related fatalities from 1982 to 2014 according to the 33rd annual report of the National Center for Catastrophic Sport Injury Research.
Concussions occur commonly in sports in which helmets are and are not worn. The rates of sports-related concussion are estimated at 1.6 to 3.8 million sports-related concussions per year ; however, only 8% to 19% of concussions are associated with a loss of consciousness. The rate in high school athletes is 0.14 to 3.66 injuries per 100 player seasons at the high school level, accounting for 3% to 5% of injuries in all sports. At the collegiate level, the exposure rate is 0.5 to 3.0 injuries per 1000 athlete exposures. Trends have shown a significant (60%) increase in concussion rates in young athletes (<19 years old) during the past decade.
Although sports participation overall is increased, this increase is likely related to better reporting, recognition, and diagnosis of concussion. Historically, concussion reporting rates have been poor. In a survey of 1532 varsity football athletes, 47% of players who sustained concussions continued to play without reporting their injuries to anyone. The most common reason athletes did not share the presence of symptoms was that the athletes did not believe the concussion was serious enough to report. Other reasons for underreporting were that athletes did not want to leave the game, did not realize a concussion was sustained, and did not want to let their teammates down. Another study reported that 70.4% of football players and 62.7% of soccer players experienced symptoms of concussion within one season, further supporting the understanding that the current reported concussion rates are likely much lower than actual rates because of unrecognized concussions.
Concussion can occur in any sport, from football to basketball to cheerleading; different studies have shown differing incident rates. A recent systematic review and meta-analysis showed the three sports with the highest incidence rates of sports-related concussion were rugby, hockey, and American football, with 4.18, 1.20, and 0.53 per 1000 athletic exposures (AEs), respectively, whereas another meta-analysis indicated the highest incident rates for tae kwon do (8.77 per 1000 athlete exposures), rugby (9.05 per 1000 player games), amateur boxing (7.9 per 1000 athlete exposures), and boys’ high school ice hockey (3.6 per 1000 athlete exposures). When specifically looking at rates of sports-related concussion in the high school population, another study showed that boys’ sports accounted for 53% of athlete exposures and 75% of all concussions. Football had the highest incident rate and accounted for the majority of concussions (53.1%), followed by boys’ lacrosse (9.2%). Among girls’ sports, soccer had the highest rate of concussions and was the second highest of the 12 high school sports studied.
Concussions can present seconds, minutes, or hours after an indirect or direct force to the head. The signs and symptoms of concussion fall into four main categories: physical, cognitive, emotional, and sleep ( Table 139.1 ).
| Physical | Cognitive | Emotional | Sleep |
|---|---|---|---|
| Headache | Feeling “foggy” | Irritability | Drowsiness |
| Nausea | Feeling slowed down | Sadness | Sleeping more or less than usual |
| Vomiting | Difficulty concentrating | Anxiety | Difficulty falling asleep |
| Balance problems | Amnesia | Emotional lability | |
| Visual problems | Confusion | Depression | |
| Sensitivity to light | Slow response to questions | ||
| Sensitivity to noise | Repeating questions | ||
| Fatigue | Difficulty with schoolwork | ||
| Dazed/stunned affect | Loss of consciousness | ||
| Seizure |
The self-reported Post-concussion Symptom Scale is a useful tool for initial assessment and also serves to facilitate follow-up. The scale is a 7-point Likert scale graded from 0 (no symptoms) to 6 (severe symptoms); multiple scales are available with a range of symptoms included. Although no specific scale has been assessed for reliability, self-reported postconcussive symptoms are associated with ongoing cerebral hemodynamic abnormalities and mild cognitive impairments. Headache is the most frequently reported symptom. Loss of consciousness occurs in only 8% to 19% of concussions and is not a defining feature of concussion; however, when prolonged loss of consciousness (>30 seconds) occurs, further evaluation may be necessary. The strongest and most consistent predictor of slower recovery from sports-related concussion is severity of symptoms in the first day, or initial days, after injury; conversely, a low level of initial symptoms is a favorable prognostic indicator. Understanding the presence of preexisting medical and mental health disorders, including migraine headaches, depression, anxiety, learning disabilities, cognitive delays, and attention-deficit disorders, is important because concussion may cause an exacerbation of underlying symptoms; in addition, athletes with preexisting mental health problems or migraine headaches may have a more prolonged recovery course, more than 1 month. However, although those with attention-deficit disorder or learning disabilities may require more extensive educational support in returning to school, they do not appear to be at greater risk for prolonged symptoms. Athletes with preinjury depression, sleep disturbances, and/or attention-deficit/hyperactivity disorder may not have a baseline (preinjury) symptom score of zero and thus are not expected to have a symptom score of zero prior to considering return to play (RTP).
Recognizing concussion may be difficult in athletes for a number of reasons. Athletes may not recognize symptoms as serious and thus not report them. Symptoms may be delayed and not appear until several hours after a concussive event occurs. In addition, athletes may not volunteer their symptoms to avoid restriction from play and because they fear they will let down their teammates.
Initial assessment on the sidelines follows the protocol of all acute head and neck injuries and begins with assessment of the airway, breathing, and circulation (ABCs) and stabilization of the cervical spine. If an athlete is unconscious after head or neck trauma, a cervical spine injury is assumed until neurologic function in all four limbs is determined to be intact and the athlete reports no neck pain or cervical spine tenderness on palpation. Immediate emergency transport with cervical precautions is essential if this evaluation is unable to be completed; if the athlete is wearing a helmet and pads, the gear should not be removed for transport, but the facemask should be removed to provide access to the airway. For athletes in whom cervical spine injuries are not suspected, evaluation can be performed on the sidelines.
When concussion is suspected, the athlete should be removed from the sporting environment and undergo a standardized multimodal assessment. Sideline assessment includes review of the athlete's symptoms, neurologic evaluation, and cognitive and balance testing. Initial neurologic testing should begin with evaluation of eye response, verbal response, and motor response as per the Glasgow Coma Scale. The next steps included further evaluation of neurologic status with examination of pupil size and symmetry, vision, reflexes, sensation, and strength. When the athlete appears stable, testing of memory, coordination, concentration, and gait/balance can ensue. Numerous sideline assessment tools are available to facilitate expedient and standardized assessments, both as printable forms and smartphone applications, including Maddocks questions, Standardized Assessment of Concussion, Balance Error Scoring System (BESS), and the Sport Concussion Assessment Tool version 5 (i.e., SCAT 5 or Child SCAT5). The SCAT5 and the Child SCAT 5 provide a comprehensive protocol ideal for sideline assessment. The SCAT 5 was released as part of the Consensus Statement on Concussion in Sport. The Child SCAT5 is designed for children 5 to 12 years old and has a symptom assessment for parent/teacher/coach/caregiver and children to report symptoms; in addition, portions of the examination, including neurologic screen and balance testing, are tailored to the younger athlete. In all of these tests, individualized baseline information is useful.
The Maddocks questions are a set of sport-specific questions designed to evaluate orientation, short-term memory, and long-term memory; these questions may provide more accurate responses than the usual orientation to time, day, date, and location. Examples of Maddocks questions are “Who scored last in the match?” and “Did your team win the last game?” These questions are useful only on the sidelines (not in a clinic setting) and are included in the comprehensive SCAT5.
Balance is an important part of the assessment after head trauma. Historically, the Romberg test has been used to assess balance subjectively. However, the BESS provides a quantifiable balance test that is straightforward to perform and objectively assesses postural stability. The BESS may be performed on the sidelines or in a clinic setting. The BESS test has been shown to be a valid and reliable tool. The BESS test is performed with the patient in three positions, first on a firm surface and then on a less-stable surface, a 10-cm-thick piece of foam. The three positions, which are well described in the SCAT5, include (1) standing flat on both feet with the hands placed on the iliac crest; (2) standing on a single leg on the nondominant foot; and (3) standing in tandem stance, heel-to-toe, with the nondominant foot in back of the other. The athlete is instructed to hold each position, to the best of his or her ability, for 20 seconds while the examiner observes the athlete for errors ( Box 139.1 ). The examiner scores the test by adding the number of errors (one error point for each error during each 20-second test). For the 5- to 9-year-old athlete, the single leg stance can be omitted to accommodate for normal developmental skillset. Because fatigue and setting have an effect on the test, it is recommended that the test be completed 15 minutes after cessation of exercise and in the same setting where the follow-up testing will be performed. Ideally, athletes will have a baseline evaluation that includes the BESS test prior to the start of the season so that comparison of postinjury and baseline testing may be incorporated to most reliably incorporate balance testing results into the RTP plan.
Hands lifted off the iliac crest
Opening eyes
Step, stumble, or fall
Moving the hip to >30 degrees of abduction
Lifting the forefoot or heel
Remaining out of the test position for >5 seconds
Although basic neurocognitive assessments are included as part of the Standardized Assessment of Concussion/SCAT5, more in-depth testing may be helpful to determine a player's readiness for safe RTP, especially in cases with chronic symptoms and questions of the athlete's truthfulness. Neuropsychological testing can be performed in one of two ways—with pencil-and-paper testing administered by a neuropsychologist or with computerized neuropsychological testing. Accessibility, time, and cost often limit the practical implication of the pencil-and-paper testing, but it can be extremely useful in cases complicated by prolonged symptoms and difficulty returning to school. Computerized testing is currently used more widely because of the ease of use and short testing times (30 to 45 minutes). Ideally, baseline neuropsychological testing is performed prior to injury to enable it to be used most effectively. Schools and teams have begun to offer and administer tests proctored by school personnel, usually athletic trainers.
Results of conventional neuroimaging (i.e., skull radiographs and head CT/MRI scans) are usually normal in persons who have had a concussion; however, prudent use of neuroimaging must be considered if an intracranial structural injury is suspected. The signs and symptoms that increase concern for a more serious injury include a worsening severe headache, seizures, focal neurologic signs, and circulatory changes ( Box 139.2 ).
Severe, worsening headache
Seizures
Focal neurologic findings
Repeated emesis
Significant drowsiness/difficulty awakening
Slurred speech
Poor orientation/significant confusion
Significant irritability
Slowed pulse
Increased systolic blood pressure with decreased diastolic blood pressure
Pupil irregularity
Loss of consciousness >1 minute
Other considerations to help determine when neuroimaging is appropriate are prolonged loss of consciousness (>30 seconds) and persistently worsening symptoms. A CT scan is the first-line testing modality recommended to evaluate for intracranial hemorrhage and skull fractures during the first 24 to 48 hours after injury. Performing a CT scan is absolutely not recommended for all concussed athletes, especially children, because of a small increased risk of brain cancer and leukemia as a result of radiation exposure. MRI is most effectively used in cases of prolonged symptoms (>3 weeks) and is primarily performed to rule out underlying structural pathology such as Arnold-Chiari malformation or arteriovenous malformation, which may cause a prolonged recovery from a concussive injury. Emerging MRI and functional imaging modalities including diffusion tensor imaging, magnetic resonance spectroscopy, single photon emission CT, and cerebral angiography may facilitate the diagnosis of concussion and assist in making RTP decisions.
The differential diagnosis of concussion includes epidural hematoma, subdural hematoma, intracerebral hematoma, and subarachnoid hemorrhage.
Epidural hematoma is a rapidly progressing intracranial hematoma that occurs from a tear of the middle meningeal artery that normally supplies the dura (the outermost covering of the brain). A fracture of the temporal bone often precipitates this hematoma. Blood accumulates between the skull and the dura and can rapidly reach a fatal size within 30 to 60 minutes. The classic clinical presentation is an athlete who sustains a blow to the head with immediate loss of consciousness followed by a lucid interval. However, the presentation can vary; sometimes the athlete may not lose consciousness, or he or she may regain consciousness with symptoms of severe, progressing headache followed by a decline in the level of consciousness. These worsening symptoms occur because the clot accumulation is causing increased intracranial pressure. If the diagnosis is an epidural hematoma, it is often obvious within the first 1 to 2 hours after injury. Treatment is emergent evacuation of the hematoma because, if the pressure is removed and no further bleeding occurs, a significant recovery can be made. However, if it is not treated expediently, an epidural hematoma can rapidly lead to death. All athletes who sustain a head injury must be monitored closely and frequently for the first 24 to 48 hours with direct access to full neurosurgical services in the event of emergency.
A subdural hematoma occurs as a result of bleeding between the brain surface and the dura; it is considered the most common fatal head injury in athletes. A subdural hematoma may occur as a result of one of a few different mechanisms, including a tear in a vein(s) running from the surface of the brain to the dura; diffuse injury to the surface of the brain; a torn venous sinus; or, less commonly, a torn small artery on the surface of the brain. Subdural hematomas are associated with brain tissue injury and thus are associated with a greater morbidity because even if the clot is evacuated early, underlying brain tissue injury has already occurred.
An intracerebral hematoma occurs from intracranial hemorrhage from bleeding into the brain substance itself, usually from a torn artery or congenital vascular lesion such as an aneurysm or arteriovenous malformation. Clinically, athletes present with rapidly progressive neurologic deterioration after a head trauma. Immediate medical attention is essential, but death occasionally occurs before the athlete is even transported to a medical facility. A full autopsy is recommended in these cases to establish the potential underlying anatomic malformation and to clarify the causative factors.
A subarachnoid hemorrhage is intracranial bleeding within the cerebrospinal fluid space along the surface of the brain. Bleeding occurs most commonly after head trauma from disruption of the tiny surface brain blood vessels. However, it can also result from a ruptured cerebral aneurysm or arteriovenous malformation. Brain swelling may be associated and may require a decompressive craniectomy, but surgery is not required for the hemorrhage itself.
Treatment of concussion is entirely nonoperative. The goal of managing an athlete with concussion is to facilitate expedient resolution of symptoms and safe RTP. Initial treatment involves physical and cognitive rest and requires comprehensive education of the patient and his or her caregivers so they understand the management plan. Management practices are based on the 5th International Conference on Concussion in Sports, which is the current standard of care. Previously many grading systems were used for concussions; however, all of the recent guidelines now focus on symptoms and returning to play. Regardless of the severity of the injury, an athlete is not allowed to RTP as long as symptoms are present.
Relative rest is an important part of the concussion management plan. This restriction is based on the pathophysiologic principle that in the setting of a metabolic imbalance and energy crisis within the brain, any increased energy demand in the brain from physical activity may worsen symptoms and delay recovery and concerns for repeat head injury during sports participation. However, limited early physical activity has been shown to be safe, effective, and better than rest alone after a brief period of rest during the acute phase (24 to 48 hours) after injury.
Cognitive rest is also essential to minimize symptoms and maximize recovery. After sustaining a concussion, athletes often report difficulty attending school, taking tests, and keeping up with assignments. Cognition is “exercise” for the brain and requires increased energy demand in the face of the postconcussion energy crisis in the brain and thus should be avoided until symptoms subside. Cognitive rest may involve staying home from school, attending only a few classes, decreased schoolwork load, allowance of extra time to complete coursework and tests, avoiding standardized testing, and taking rest breaks during the day. In addition, all activities that require concentration or offer stimulus to the brain must be avoided as part of cognitive rest, including playing video games, using the computer, watching television (especially intense, dramatic, violent programming), listening to loud music, and exposure to bright lights. Development of an individualized return to learn program with appropriate school accommodations is recommended to facilitate recovery. Lastly, because of slowed reaction times, licensed drivers with a concussion should avoid driving until they are cleared for activity.
Treatment should be individualized and specifically targeted at the symptom profile identified on assessment. In addition to symptom-limited aerobic exercise programs, targeted physical therapy programs addressing neck strain and vestibular dysfunction and cognitive behavioral therapy to address mood disturbances may be implemented as needed. If pharmacotherapy is prescribed, health care providers must recognize that pharmacologic agents may mask or modify symptoms of concussion.
After a concussion, athletes should not RTP on the day of injury, especially for the pediatric or adolescent athlete. Legislation in all 50 states in the United States requires all athletes with a suspected concussion to be removed from any sports participation until they are given clearance to RTP from a licensed health care professional. Although most athletes display resolution of symptoms within 7 to 10 days, the recovery time frame may be longer in children and adolescents.
For deciding when to RTP, asymptomatic athletes are directed to follow a medically supervised stepwise process, based on the summary and agreement statement of the 5th International Conference on Concussion in Sports. The patient should never return to contact play while symptomatic; however, athletes are encouraged to become gradually more active while staying below their cognitive and physical symptom-exacerbation thresholds. All RTP programs must be individualized because every athlete recovers at a different pace. In addition, concussed athletes should be free from concussion-related symptoms and not using any pharmacologic agents that may mask or modify symptoms; decisions regarding RTP while still on such medication must be considered carefully by the treating clinician. The following protocol is recommended by the 5th International Conference on Concussion as a guideline to be completed with appropriate supervision ( Table 139.2 ):
| Level | Activity |
|---|---|
| 1 | Symptom-limited activity (daily activities that do not provoke symptoms) |
| 2 | Light aerobic exercise (e.g., walking, stationary cycling) |
| 3 | Sport-specific training (e.g., skating for hockey, running for soccer) |
| 4 | Noncontact training drills (e.g., passing drills, progressive resistance training) |
| 5 | Full-contact training after medical clearance |
| 6 | Return to sport/normal game play |
Each level requires at least 24 hours, and a minimum of 5 days is required to progress through the protocol to be cleared for full participation. However, any return or increase of symptoms at any stage of the protocol is indication that concussion recovery is inadequate. If any postconcussion symptoms reoccur or worsen the patient should drop back to the previous asymptomatic level and try to progress again after 24 hours. If an athlete completes all levels with minimum of 24 hours between levels, tolerates noncontact training activities without symptom, the athlete is considered cleared to advance to contact practice and ultimately full game play if asymptomatic with practice. While athletes may advance through the RTP protocol with symptoms, they cannot advance beyond noncontact activity until at preconcussion baseline, ideally symptom free. Athletes with a history of multiple concussions or prolonged postconcussion syndrome may require longer intervals as they progress through each level of recovery.
Athletes who have sustained traumatic intracranial bleeding may begin the gradual RTP protocol for noncontact sports after a minimum of 6 weeks to enable the bone flap to heal after a craniotomy; however, after traumatic intracranial bleeding, decisions regarding return to activity and ultimate potential return to contact sport are determined by the neurosurgery team.
Although the large majority of concussions self-resolve within 7 to 10 days in adults and 3 to 4 weeks in children, complications may occur, including postconcussion syndrome (PCS), second-impact syndrome, long-term effects, and chronic traumatic encephalopathy (CTE).
PCS refers to the presence of symptoms beyond the normal duration of recovery. Many variations exist in the specifics of the PCS definition, and no set of criteria is universally accepted. PCS is commonly defined as the persistent presence of three or more symptoms with the duration loosely defined and broadly variable between sources. The two most commonly applied definitions are proposed by the World Health Organization International Statistical Classification of Diseases and Related Health Problems (ICD)-10 and the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) ( Table 139.3 ). However, the DSM-V significantly changed the specific defining criteria, and now classifies PCS within major or mild neurocognitive disorder due to TBI.
| Who ICD-10 | DSM-IV | |
|---|---|---|
| Minimum duration of symptoms | na | 3 months |
| Number of symptoms | 3 | 3 |
| Defining symptoms | Headache | Fatigue |
| Dizziness/vertigo | Disordered sleep | |
| Easily fatigued/easily tired | Headache | |
| Irritability | Vertigo/dizziness | |
| Poor concentration | Anxiety | |
| Forgetfulness | Depression | |
| Sleep disturbance | Personality changes | |
| Depression | Apathy | |
| Anxiety |
Second-impact syndrome is a debated term that applies to the pathophysiology that occurs when an athlete sustains a second head trauma prior to complete symptom resolution after an initial head injury. Second impact syndrome results in cerebral vascular congestion that progresses to diffuse cerebral swelling and is associated with a high mortality rate. This second hit occurs during the period of enhanced vulnerability characterized by an increased brain cell demand for glucose in the face of reduced cerebral blood flow and impaired cerebral vascular autoregulation. Because pediatric and adolescent athletes have demonstrated longer recovery times from the initial decreased cerebral blood flow, these younger athletes are at higher risk of second impact syndrome.
The long-term effects of one or multiple concussions are inconsistent and largely unknown because minimal large-scale scientific investigation of the long-term consequences of brain injury in athletes has been performed. Studies of amateur boxers reveal similar chronic neurocognitive effects ; however, professional boxers show much more significant long-term neurocognitive effects, with older studies showing that 17% of retired boxers demonstrate CTE. A genetic predisposition to CTE may exist. More recent studies accounting for the reduction in exposure to repetitive head trauma and increasing medical monitoring of boxers predict a lower incidence in the future. A recent systematic review looking at original research of retired athletes 10 or more years after injury found that some former athletes have depression and cognitive deficits later in life, and there is an association between these deficits and multiple prior concussions. Former athletes are not at increased risk for death by suicide. Former high school American football players do not appear to be at increased risk for later life neurodegenerative diseases; in two medical record linkage studies of former high school football players, the rates of dementia, mild cognitive impairment, and parkinsonism did not differ in comparison with control subjects. National Football League (NFL) retirees with a history of three or more concussions show a threefold increase in the risk of depression and memory problems and a fivefold increased prevalence of mild cognitive impairment (e.g., memory, concentration, and speech) when compared with retirees without a history of concussion. However, in a study of retired NFL players, mortality and suicide rates are lower than the general population. Further study is necessary to better understand long-term sequelae from concussion.
CTE is described as a progressive neurodegenerative disease that is associated with repetitive head trauma. CTE can only be diagnosed by neuropathologic examination of the brain. Consensus criteria that provide a standardized approach for the neuropathology of CTE have been developed by the US National Institutes of Neurological Disease and Stroke (NINDS) and the National Institute of Biomedical Imaging and Bioengineering (NIBIB). Trauma is hypothesized as a trigger of progressive brain cell degeneration, leading to an accumulation of an abnormal protein called tau; however, no direct cause-effect relationship has been demonstrated yet between CTE and sports-related concussion or exposure to contact sports. CTE presents clinically with symptoms of headaches, memory loss, disorientation, impaired judgment, impulse control problems, aggression, depression, tremors, abnormal gait/speech, and ultimately dementia and sometimes suicide; symptoms may develop months, years, and decades after the traumatic events and often the diagnosis is made postmortem at autopsy. Further prospective, longitudinal, population-based, blinded neuropathologic studies evaluating athletes involved in high- and low-impact sports are needed to further understand this pathology.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here