Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Hand and upper extremity transplantation is the most common form of vascularized composite allotransplantation (VCA) or reconstructive transplantation and has evolved from a procedure only performed at the distal forearm level to a procedure now being performed above the elbow more proximally. At the time of writing this chapter, the authors can count 107 hand and upper limb transplants performed throughout the world. The “modern era” of hand transplantation was ushered in with the first hand transplants performed with modern immunosuppressive medications in 1998 in Lyon, France, and 1999 in Louisville, KY. While both transplants were unilateral distal forearm level transplants performed 4 months apart, the Louisville transplant was the first to demonstrate long-term success due to patient compliance. This emphasized patient-centric factors, which are critical to the success of any kind of transplant. Psychological and social factors are the most important elements in long-term “graft” maintenance. Therefore, all successful upper extremity transplantation begins with screening. Following screening, careful surgical planning must be performed and precise execution of both donor and recipient portions of the transplant operation must be accomplished. Postoperative monitoring and therapy are instituted and therapy may be required for several years to come. Rejection episodes and complications should be expected and anticipated. This chapter discusses the key portions necessary for performing and maintaining a successful upper limb allotransplant.
Despite the fact that the clinical results and outcomes with hand and upper extremity transplantation have been highly encouraging, the requirement of life-long, high-dose, multidrug immunosuppression associated with a profound side-effect profile still hampers broader application of these life-changing reconstructive modalities. Currently, there is no standard immunosuppressive regimen established for extremity transplantation; however, most patients have been treated with a “conventional” triple-drug immunosuppressive strategy, largely extrapolated from solid organ transplantation. This includes either polyclonal (antithymocyte globulin, ATG) or monoclonal (alemtuzumab or basiliximab) antibody induction therapy followed by high-dose tacrolimus, mycophenolate mofetil (MMF), and steroids for maintenance immunosuppression.
The adverse effects and toxicities of these immunosuppressive agents include metabolic, infectious, and neoplastic sequelae, and in extreme cases may contribute to patient mortality. Specifically, the triple-drug regimens have resulted in nephrotoxicity, hypertension, new-onset diabetes mellitus, hyperlipidemia, leukopenia, cardiovascular disease, and bilateral hip osteonecrosis. Opportunistic infections have also been observed, most commonly with cytomegalovirus (CMV), which can be potentially life-threatening and can trigger acute rejection. This has led some centers to avoid the high-risk combination of CMV-positive grafts in CMV-negative recipients in upper extremity transplantation. Other encountered opportunistic infections include human papillomavirus, herpes simplex, Staphylococcus aureus osteitis, Clostridium difficile , molluscum contagiosum, and mycoses. Malignancy is another common complication after solid organ transplantation, with an incidence up to five-fold higher in transplant recipients compared with the general population. However, most hand and upper extremity transplant recipients have been followed for <10 years, so it is difficult to assess the true risk and incidence faced by these patients with regard to malignancy.
The risks associated with the long term, potentially lifelong usage of these drugs have prevented the widespread application of VCA as a first-line reconstructive modality in patients with complex tissue defects and limb loss. Therefore, there is a critical need for novel protocols that will allow patients to be weaned off immunosuppression or to induce tolerance to their grafts.
Several centers around the world, including our own, have attempted to develop novel, innovative therapeutic concepts of immunoregulation to reduce systemic immunosuppression to minimal levels. Similarly, recent advances in cell-based therapies and immunosuppressive drug development that incorporate the unique elements and biology of vascularized composite allografts have also shown favorable results at achieving this goal. Clearly, the induction of donor-specific tolerance would obviate the need for long-term maintenance immunosuppression after extremity transplantation, and great strides in this regard have currently been made in translational large animal models. However, until those strategies are implemented in the clinical arena, we advocate for short-course depletional induction followed by low-dose maintenance monotherapy to minimize toxicities of conventional immunosuppression and maximize the risk–benefit ratio for hand and upper extremity transplantation. Our group has recently successfully implemented such a protocol for upper extremity transplantation with favorable functional and immunologic outcomes.
The authors feel that upper extremity transplant is indicated for individuals of adequate social, psychological, medical, and immunologic health who have unilateral or bilateral hand/upper limb loss that has resulted in significant functional and/or psychological disability, when a substantial enough improvement (based on the level of transplantation and expected functional recovery) can be anticipated that ethically weighing the balance of risks and benefits favors transplantation. We hesitate to create specific indications such as only bilateral amputees or bilateral or dominant hand unilateral amputees only, because this does not incorporate the global assessment of function and potential benefit that a patient may experience through a thoughtful application of reconstructive transplantation. The authors apply this philosophy also through their cell-based, nonsteroid, monotherapy, immunoregulatory protocol, as indicated above. However, many centers worldwide, using traditional immunosuppression do consider only bilateral amputees or unilateral amputees of dominant hands only, and exclude nondominant unilateral amputees and above elbow amputees.
The importance of screening cannot be emphasized enough. Screening includes evaluations of the patient's psychological and social problems, tools, weaknesses, and strengths. Some patients are hand transplant candidates due to “bad luck” or circumstances out of their control. But some are missing limbs due to poor decision-making that may have been a single episode of lack of judgment, or a long-standing pattern of bad choices. One must consider if a pattern of bad choices will change because of a hand transplant. The single best predictor of transplant medication compliance by a patient is the presence of stable and caring family/friends actively engaged within the patient's life.
Further screening involves evaluation of the patient medically to see if they are healthy enough to undergo a long and physiologically taxing procedure and the immunotherapy regimen to follow without substantially worse risks for problems such as malignancy, renal disease, heart disease, pulmonary disease, infection, ocular disease, dental disease, etc. Many patients may have added risk for infection due to their initial disease process causing limb loss. Our liver transplant anesthesia providers also evaluate the patient for possible line placement and anesthesia risk/concerns.
Immunological screening involves blood and HLA typing, assessment for pre-formed donor-specific (DSA) or HLA antibodies and sensitization, as well as further assessment for infectious diseases known to complicate the immunological management and prognosis for rejection and malignancy in the future such as CMV and EBV infection. It is the authors' practice that recipients who are seronegative for antibodies, indicating no prior infection with these viruses, should not receive transplants from CMV+ or EBV+ donors. All patients should include an evaluation by a transplant infectious disease physician to screen for these and other problems.
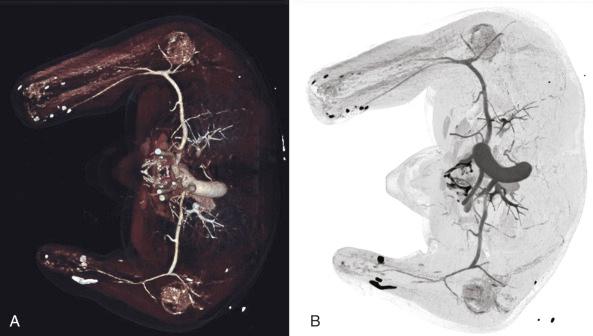
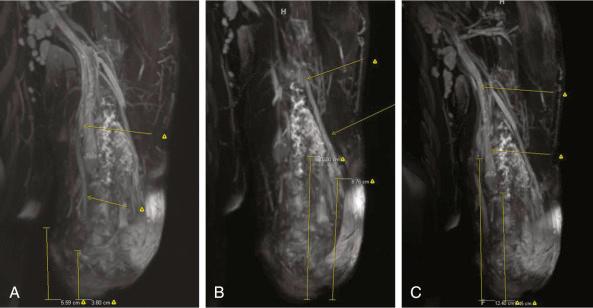
Surgical evaluation focuses on the function of the patient with and without prostheses, and one should also consider their prior participation in rehabilitation. Surgical planning focuses on the level of amputation along with associated hard and soft tissue deficits proximal to the amputation site, which may either complicate a transplant or require reconstruction before or during the transplant. Physical evaluation for skin quality, joint range of motion, remaining motor group strength, location of scars, location of Tinel's sign over nerve stumps, limb/stump length and circumference, palpable pulses, wounds, heterotopic ossification, etc. should be noted. Radiographic evaluation includes plain films of both upper limbs and either conventional or computed tomographic angiography, along with venous phase reconstructions ( Fig. 65.1 ). Venous mapping is also performed by ultrasound with vein locations and diameters recorded. We physically map the veins with a surgical marking pen and then photograph the limbs for a permanent record of vein location. MR neurography ( Fig. 65.2 ) may be employed when necessary to evaluate for location of nerve stumps or possible traction/avulsion injury of peripheral nerves more proximal than expected by location of amputation. The authors perform this imaging on all patients capable of having MR neurography performed if their mechanism of injury/amputation allows for the possibility of stretch or avulsion injury and/or an obvious Tinel's sign that is reproducible to the correct nerve sensory distribution cannot be elicited in the vicinity of the amputation stump.
Once patients have been approved following close and detailed screening, they may be enrolled into our IRB-approved hand and upper extremity transplant program. Patients will not be enrolled if they use any form of tobacco, illegal substance, or cannot commit to staying at our institution for at least 3 months postoperatively or treating rehabilitation as their full-time job for the first 1–2 years after transplantation.
Each patient gets a reconstructive transplantation operative plan specifically designed for their particular anatomic needs. While many will have certain similarities, none are exactly the same. Planning incorporates known factors such as soft tissue coverage and skin quality, skeletal factors such as limb length, joint condition, presence of heterotopic ossification, vascular imaging, and possible nerve imaging, as well as unknown factors such as the degree of muscle versus scar present, quality of remaining muscle, potential nerve quality and length, tendon length, potential for indolent infection, etc. All surgical planning incorporates our desire to protect the length of the patient's limb if at all possible, assuming the transplant were to fail. This means preserving a proximal forearm stump with muscle coverage while still transplanting adequate forearm motors to make a forearm-hand transplant functional, for example. Conversion of a below elbow to above elbow prosthesis user would be a devastating complication for a patient who suffers a transplant loss. However, for a patient with significant elbow pathology already, replacing this joint with a transplant may actually allow for better ultimate function and may be a consideration.
Surgical plans are discussed in classroom format with group input and then any remaining questions are worked out as a group in the cadaver anatomy laboratory. Once the various components of the surgical plan have been discussed and worked through, another cadaver rehearsal is performed with the correct surgical sequence used and the plan is continually refined until all group members are satisfied.
Surgeons are assigned by name to specific teams and tasks, both incorporating their clinical strengths as well as their ability to work with individual team members. Usually we use a plastic surgery hand surgeon and an orthopedic surgery hand surgeon on each three-member team, with the additional member being either another hand surgeon, a microvascular plastic surgeon, or hand surgery/microsurgery fellow. This balance of team members ensures that appropriate soft tissue and hard tissue techniques and care will be provided. Osteosyntheses are performed by hand surgeons of either specialty, as long as they have the appropriate expertise.
Microsurgery (nerve and vascular) is performed by the plastic surgery hand surgeons, plastic surgery microsurgeons, or orthopedic hand surgeons who have adequate training and experience in microsurgery.
In an effort to prevent surgeon fatigue, surgeons are able to rotate in and out of the operation in teams once the osteosynthesis begins as the two teams per limb transplanted reduce to one team. Thus, half the previously operating members may break and further team members who may not have yet operated can also be used to help relieve surgeons. Typically, the microsurgery team is a different group than the team performing the osteosynthesis and tendon/muscle repairs. The microsurgery team may also rotate in/out individual members as the hours pass, as every vein capable of coaptation is usually anastomosed resulting in an artery to vein ratio of 2 or 3 : 1.
For many amputees in the middle third of the forearm and brachium, the decision to use the already present muscles to power the transplant or replace the existing muscles must be made. The authors are unaware of any current guidelines to help direct this decision. The surgeon must decide if the motors present have adequate length, and cross-sectional area, and if they themselves have sustained intrinsic damage that may result in loss of excursion or strength, such as fibrosis, based on their physical assessment of the patient and the mechanism of limb loss. It is likely that blast injuries and ischemic injuries may compromise surviving muscle and limit its ability to provide excursion or power. However, replacing these already innervated motors will result in some loss of motor axon count providing innervation and allows for “mistakes” in reinnervation, such as synkinesis, loss of specificity, or failure to reinnervate. In the authors' limited experience, we currently prefer to replace questionable forearm motors if half or more of the muscle-tendon unit length is considered compromised or missing. Even less experience is present to guide transhumeral transplants. However, based on our unpublished anatomic research, even up to the junction of the proximal and middle thirds, enough new elbow flexor and extensor motor units are being transferred so that this may be considered an innervated muscle transfer as well. For transplants at the mid-brachium to distal third, our experience is that adequate elbow strength is obtainable using the recipient's own motors if those muscles are otherwise uncompromised.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here