Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
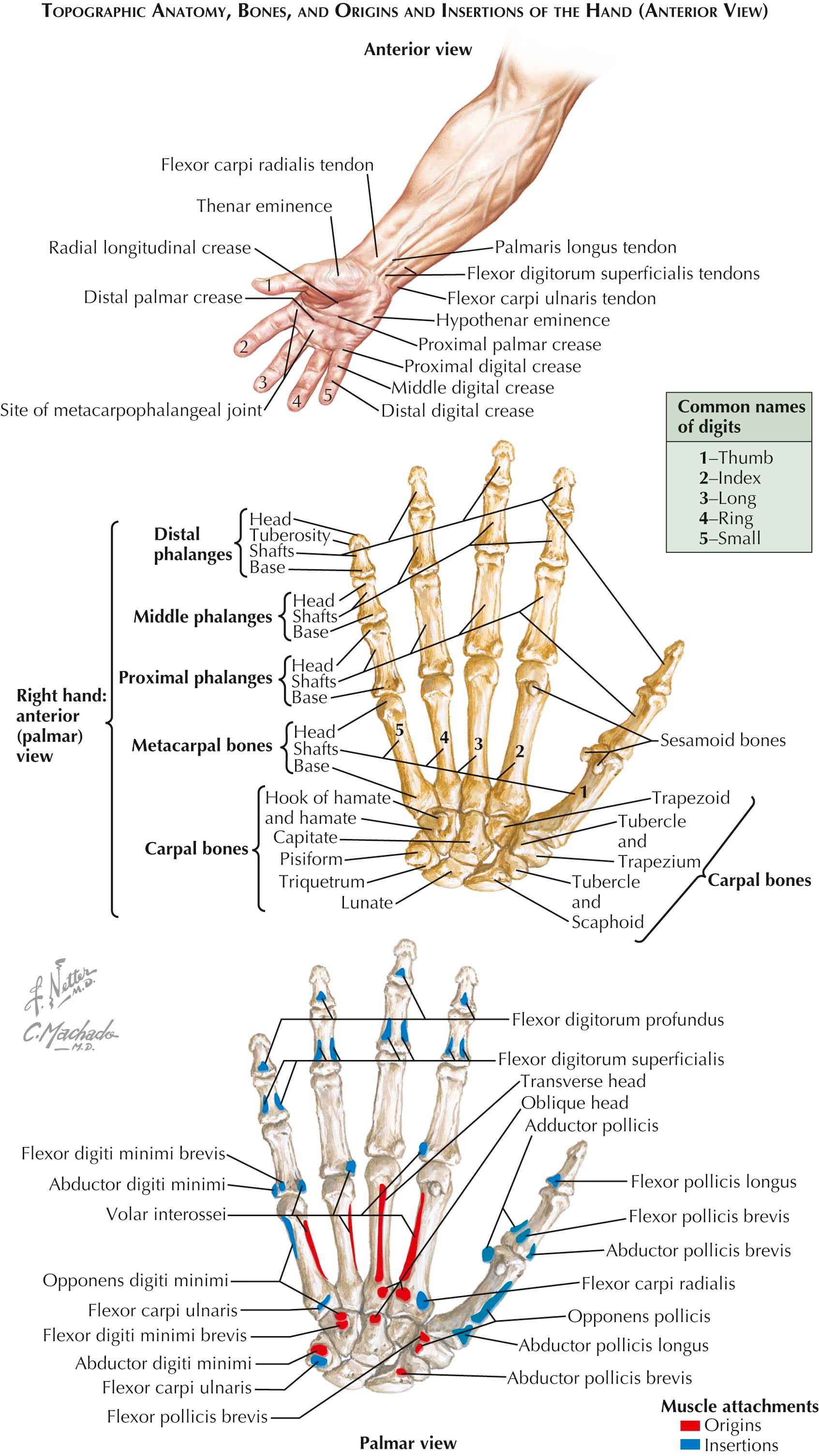
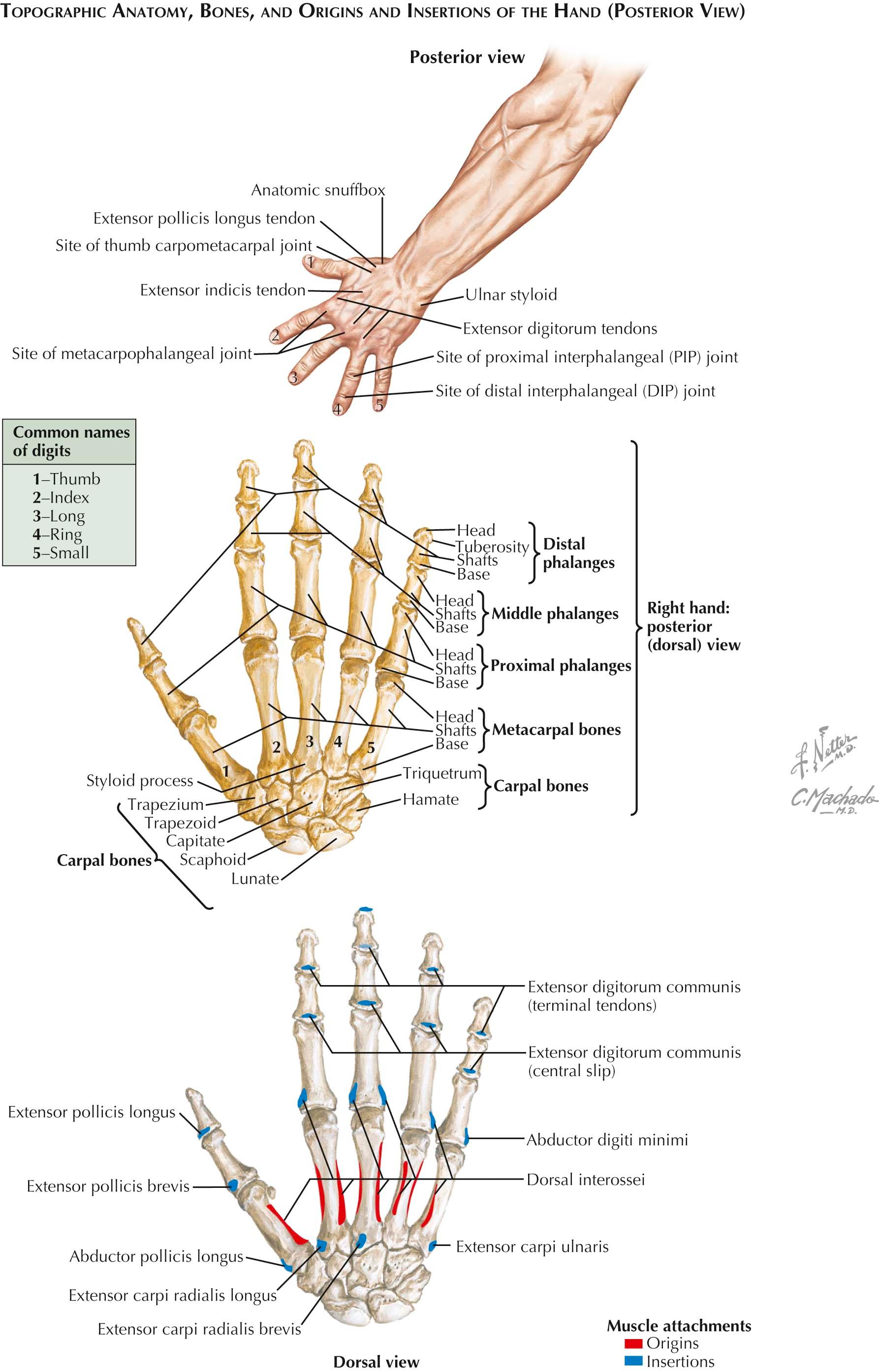
Five metacarpals form the skeleton of the hand. They are miniature “long” bones, comprising a shaft, a head, and a base. They are palpable on the dorsum of the hand and terminate distally in the knuckles, which are their heads (see Plates 4-1 and 4-2 ).
The shaft is curved longitudinally so as to be convex dorsally and concave on its palmar aspect. The head, the distal extremity, has a rounded smooth surface for articulation with the base of the proximal phalanx. The sides of the head exhibit pits, or tubercles, for the attachment of ligaments. The articular surface of the head is also convex transversely, although less so than dorsopalmarward so that the head fails to be a sphere; however, flexion and extension and abduction and adduction are permitted. The base is cuboidal and broader dorsally than palmarward. Its ends and sides are articular, and the dorsal and palmar surfaces are rough for ligamentous attachments.
The first (thumb) metacarpal is shorter and stouter than the others, and its palmar surface faces toward the center of the palm. It has a proximal saddle-shaped articular surface for contact with the trapezium. Apart from its regular head configuration, it has two palmar articular eminences for the sesamoids of the thumb.
The second (index finger) metacarpal is the longest, and its base is the largest of the metacarpals. There is a deep dorsopalmar groove in the base, which accepts the trapezoid, and the ridges bounding the groove make contact with the trapezium and the capitate. On the ulnar side of the base, there is an incompletely divided facet for the base of the third metacarpal. This complex articulation at the base makes it relatively immobile for power pinch and grip activities.
The third (long finger) metacarpal is distinguished by its styloid process, a dorsally and radially placed proximal eminence. The carpal surface of the bone is concave for the capitate. Subdivided facets exist on the sides of the base for articulation with the bases of the second and fourth metacarpals, also making it relatively immobile.
The fourth (ring finger) metacarpal has a square base that, proximally, has a large facet for the hamate and, laterally, a small facet for the capitate. Two facets on the lateral side of the base make contact with the base of the third metacarpal; and a single, oval facet on the other side faces the fifth metacarpal, allowing for significant motion during power grip.
The fifth (small finger) metacarpal has a single, concavoconvex facet on the proximal surface of its base for articulation with the hamate. A slightly convex facet on the radial side is received into the matching oval facet of the fourth metacarpal that allows for the most movement at the carpometacarpal joint of all the lesser fingers. On the ulnar side of the base there is a prominent tubercle for the attachment of the tendon of the extensor carpi ulnaris muscle.
Ossification of the metacarpals proceeds from two centers—one for the body of the bone and one for the distal extremity in each of the four fingers, except for the proximal extremity in the thumb. Ossification begins in the shafts in the eighth or ninth week of fetal life. The centers for the extremity epiphyses appear during the second year, and fusion takes place between ages 16 and 18.
The phalanges are 14 in number, being one short in the thumb (see Plates 4-1 and 4-2 ). These, too, are miniature long bones, with a shaft and two extremities. The dorsum of the shaft is markedly convex from side to side; its palmar surface is nearly flat. The margins of the palmar surfaces are ridged for attachment of the fibrous flexor sheaths of the digits. The proximal extremity of the first phalanx of each digit is concave and oval and broader from side to side for articulation with the head of the metacarpal. Distally, the proximal extremities of the middle and distal phalanges have two shallow concavities separated by an intervening ridge, which articulate with the pulley-like surfaces on the distal ends of the middle and distal phalanges. The distal phalanges exhibit terminal elevated roughened surfaces, which support the pulp of the fingers. The sides of the bases of the phalanges show tubercles for ligaments; the sides of the heads (except on the distal phalanx) exhibit shallow pits for ligamentous attachments.
Ossification of the phalanges proceeds from two centers—one for the body and one for the proximal extremity. Ossification in the shaft begins about the eighth week of fetal life and in the epiphysis occurs during the second and third years, with fusion taking place between 14 and 18 years of age.
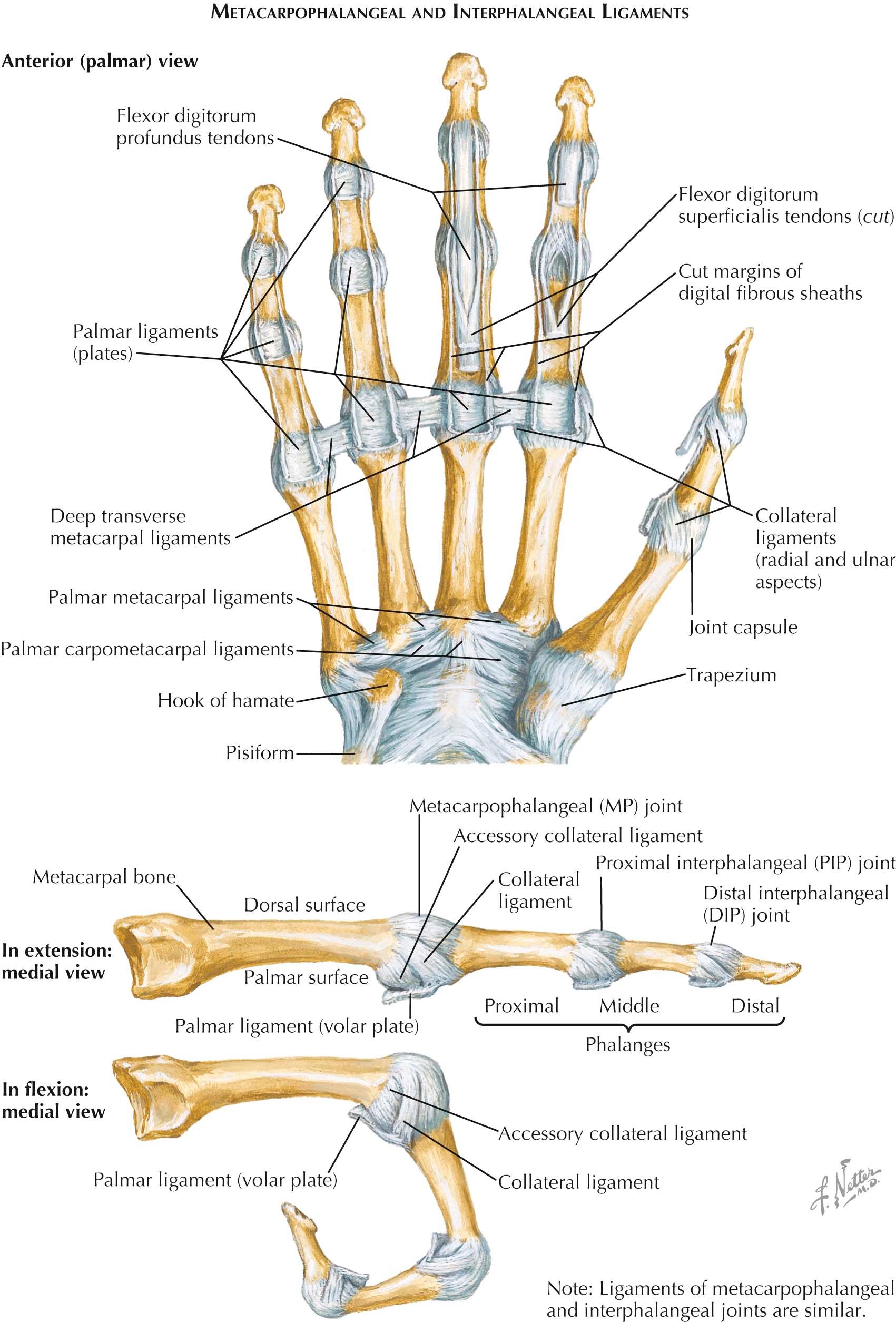
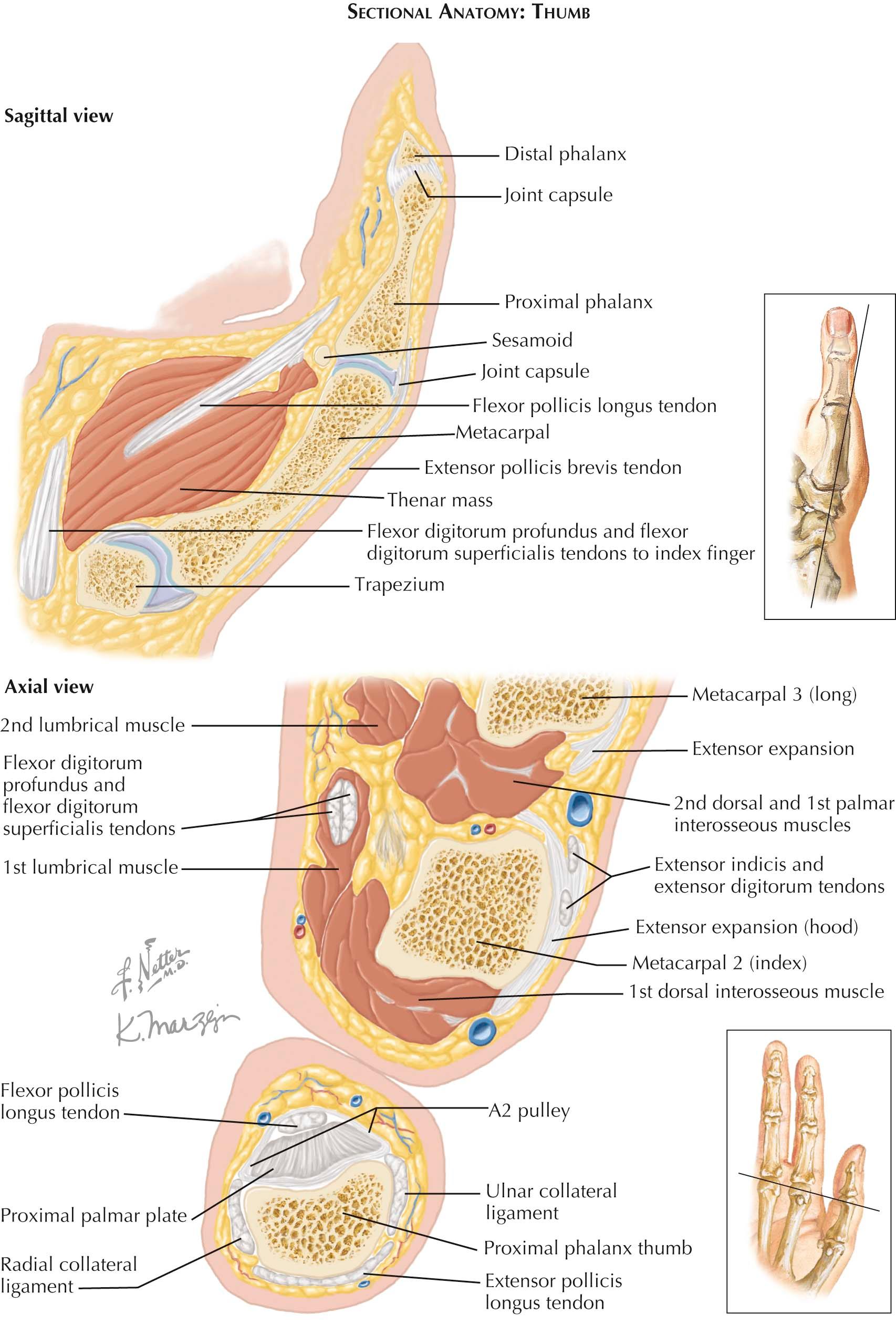
The carpometacarpal joint of the thumb is the independent joint between the trapezium and the base of the first metacarpal (see Plate 4-3 ). The articular surfaces are reciprocally concavoconvex, and a loose but strong articular capsule joins the bones. The biaxial nature of this joint provides for flexion and extension and abduction and adduction, and the looseness of its capsule allows opposition of the thumb that involves a small amount of rotary movement (circumduction).
The carpometacarpal joints of the four fingers participate with the intercarpal and intermetacarpal joints in a common synovial cavity. Dorsal and palmar carpometacarpal ligaments run from the carpals of the second row to the various metacarpals. Short interosseous ligaments are usually present between contiguous angles of the capitate and the hamate and the third and fourth metacarpals.
These joints occur between the adjacent sides of the bases of the four metacarpals of the fingers. Here, also, there are dorsal and palmar ligaments, and interosseous ligaments close off the common synovial cavity by connecting the bones just distal to their articular facets. Only slight gliding movements occur between the metacarpals and between them and the carpals to which they are related. However, the articulation between the hamate and the fifth metacarpal allows that bone to flex appreciably during a tight grasp and also to rotate slightly under the traction of the opponens digiti minimi muscle.
The deep transverse metacarpal ligaments are short and connect the palmar surfaces of the heads of the second, third, fourth, and fifth metacarpals. They are continuous with the palmar interosseous fascia and blend with the palmar ligaments of the metacarpophalangeal joints and the fibrous sheaths of the digits. They limit the spread of the metacarpals, and the tendons of the interosseous and lumbrical muscles pass on either side of them.
These joints are condyloid, and both the rounded head of the metacarpal and the oval concavity of the proximal end of the phalanx have unequal curvatures along their transverse and vertical axes. An articular capsule and collateral and palmar ligaments unite the bones. The articular capsule is rather loose. Dorsally, it is reinforced by the expansion of the digital extensor tendon.
The palmar ligament is a dense, fibrocartilaginous plate, which, by means of its firm attachment to the proximal palmar edge of the phalanx, extends and deepens the phalangeal articular surface. It is loosely attached to the neck of the metacarpal; in flexion, it passes under the head of the metacarpal and serves as part of the articular contact of the bones. At its sides, the palmar ligament is continuous with the deep transverse metacarpal ligaments and the collateral ligaments. The collateral ligaments are strong, cordlike bands attached proximally to the tubercle and adjacent pit of the head of the metacarpals and distally to the palmar surface of the side of the phalanx. Their fibers spread fanlike to attach to the palmar ligaments. Movements of flexion and extension, abduction and adduction, and circumduction are permitted at these joints. With extension is associated abduction, as in fanning the fingers; with flexion is associated adduction, as in making a fist. The metacarpophalangeal joint of the thumb is limited in abduction and adduction; its special freedom of motion derives from its carpometacarpal joint.
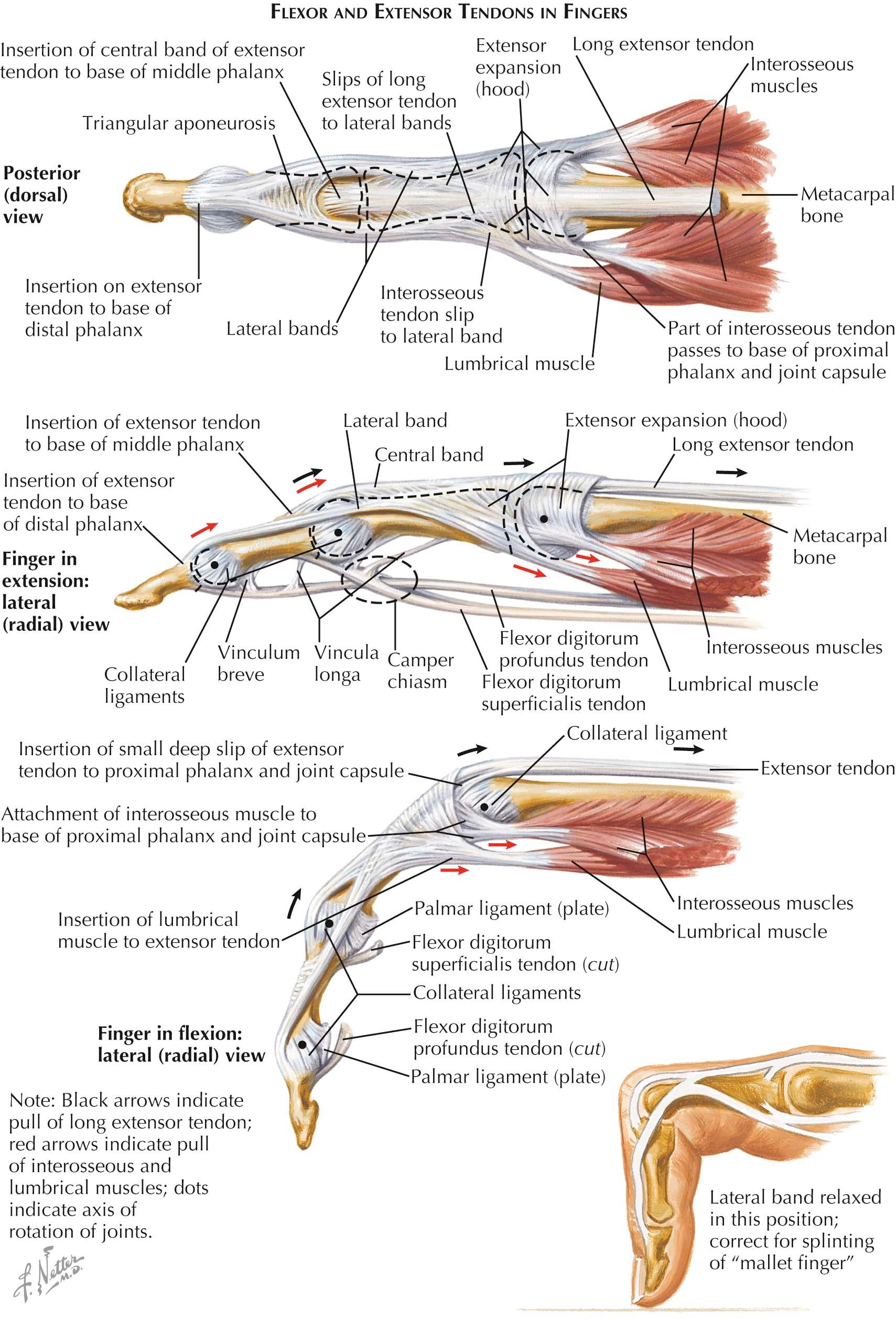
Structurally similar to the metacarpophalangeal series, the interphalangeal joints have the same loose capsule, palmar and collateral ligaments, and dorsal reinforcement from the extensor expansion. However, owing to the pulley-like form of their articular surfaces, action here is limited to flexion and extension. Flexion is freer than extension and may reach 115 degrees at the proximal interphalangeal joint. Arteries and nerves serving these joints are twigs of adjacent proper digital branches.
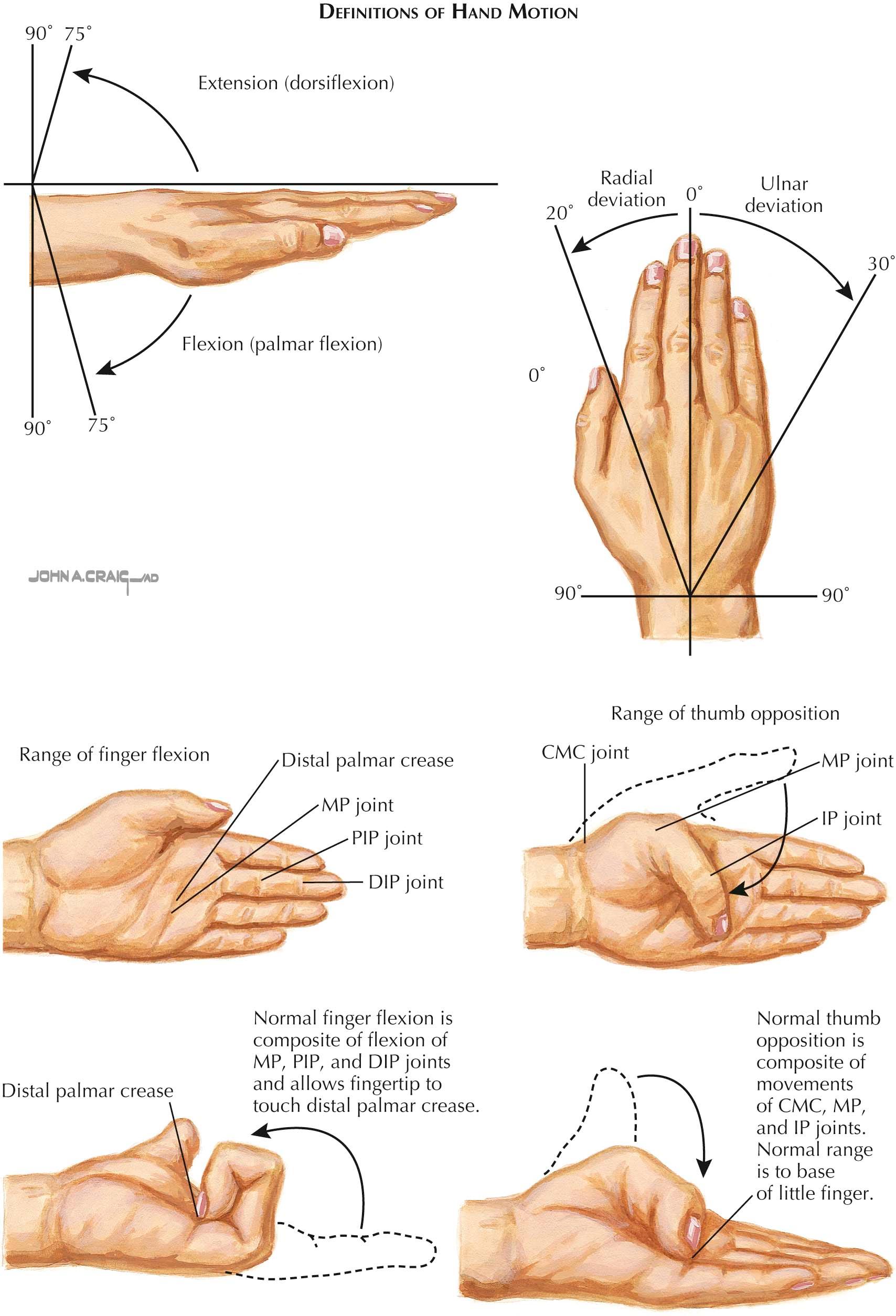
The unique bony and articular anatomy of the hand allow for a myriad of movements, and the cumulative movement of each joint in series increases the total active motion (TAM). By convention, movement toward the palm is described as palmar or volar or anterior and movement toward the back of the hand is described as dorsal or posterior. Movement of the hand toward the thumb side of the arm is described as radial or lateral and toward the small finger as ulnar or medial.
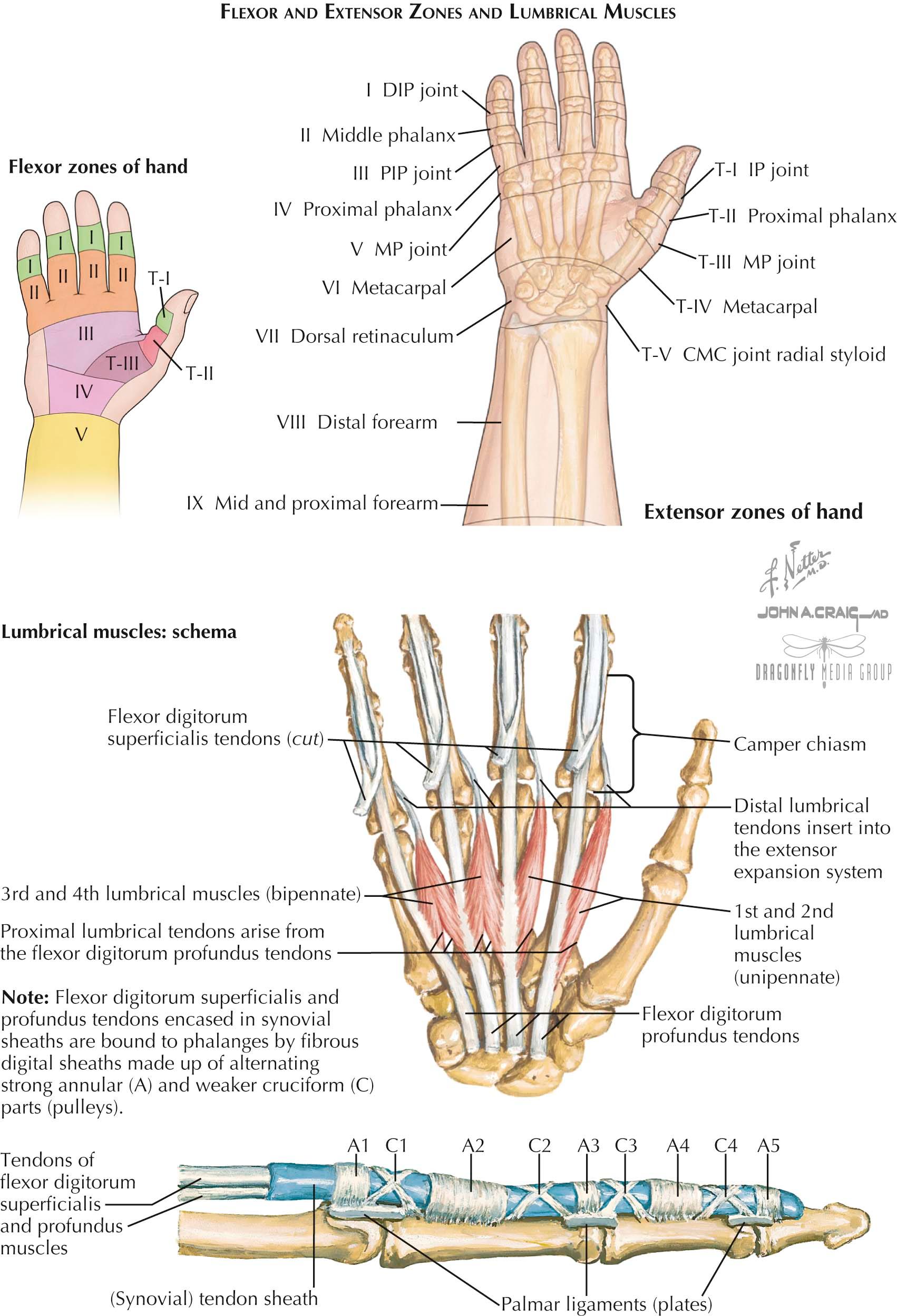
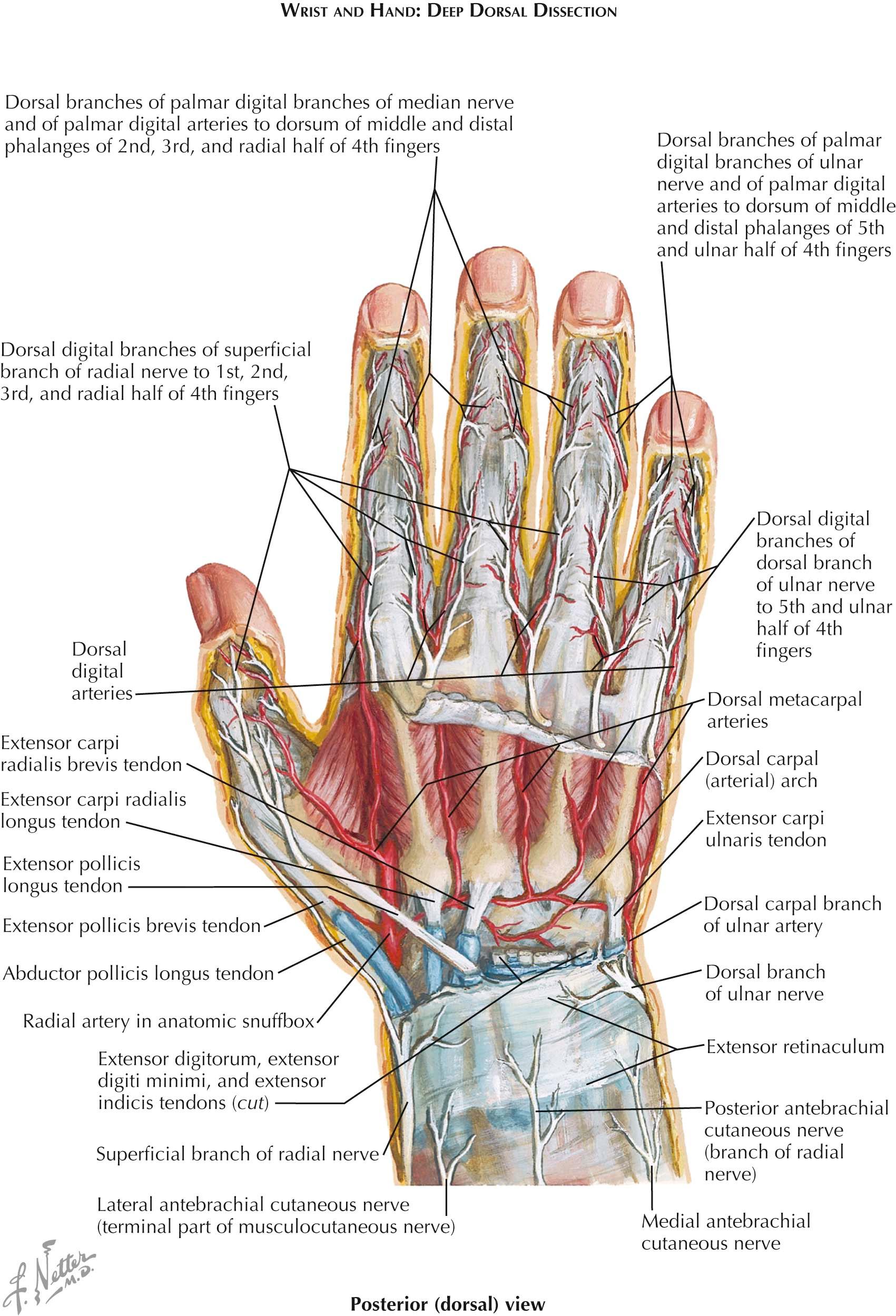
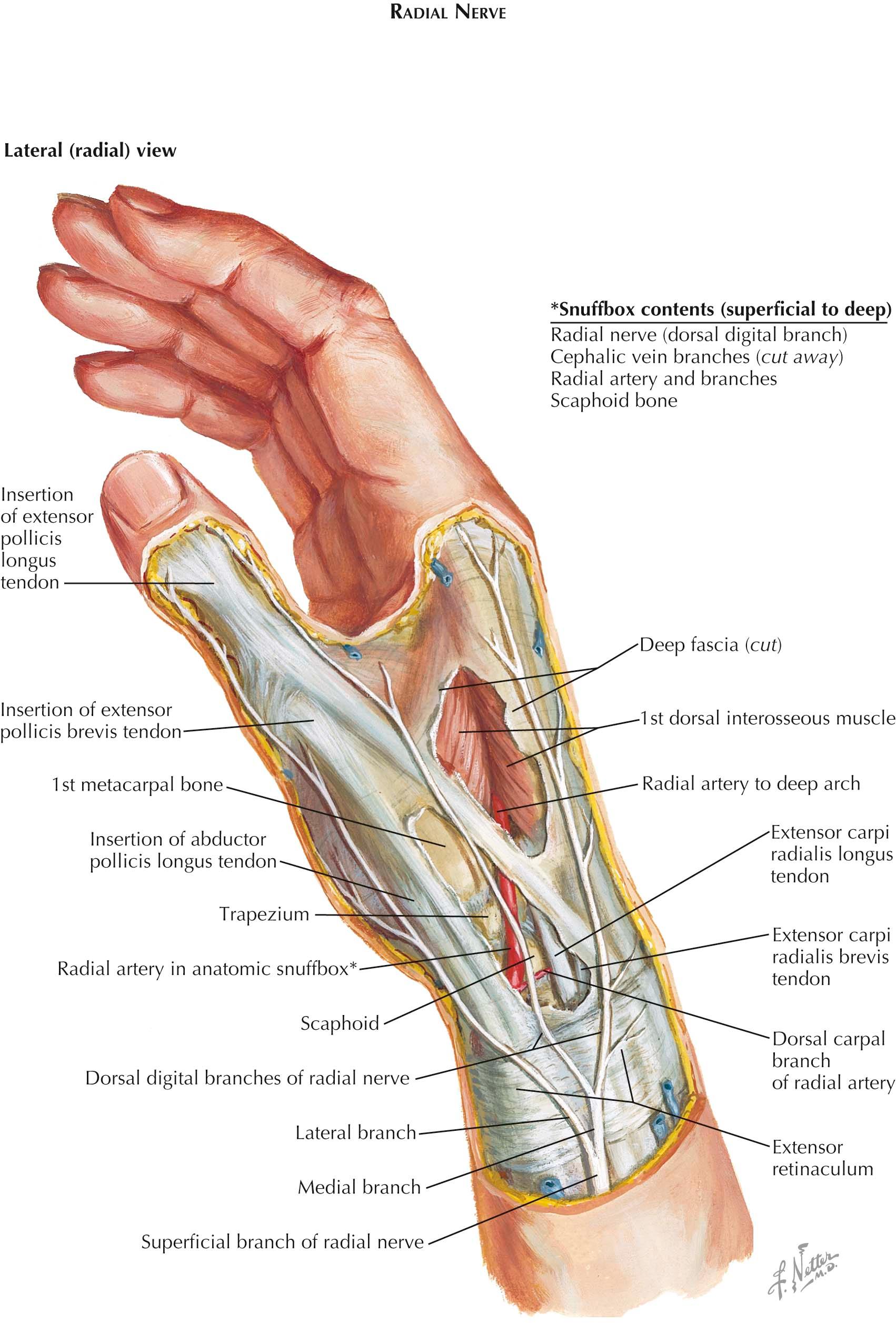
As the flexor and extensor tendons pass from the wrist to the hand, clinical zones have been described that help physicians articulate more precisely the significant anatomic differences that exist in each zone that affect finger function after injury (see Plates 4-5 and 4-6 ). As the extensor digitorum tendons diverge over the dorsum of the hand, they are interconnected by intertendinous connections. These prominently interconnect the tendons for the third, fourth, and fifth digits and severely limit the independent action of these digits, especially the fourth digit. Independent extensor action is retained for the index finger. The convergence of the tendon of the extensor pollicis longus muscle toward the tendons of the abductor pollicis longus and extensor pollicis brevis muscles defines a hollow known as the anatomic snuffbox (see Plate 4-14 ). In the floor of this hollow, the radial artery passes toward the dorsum of the hand and gives off its dorsal carpal branch.
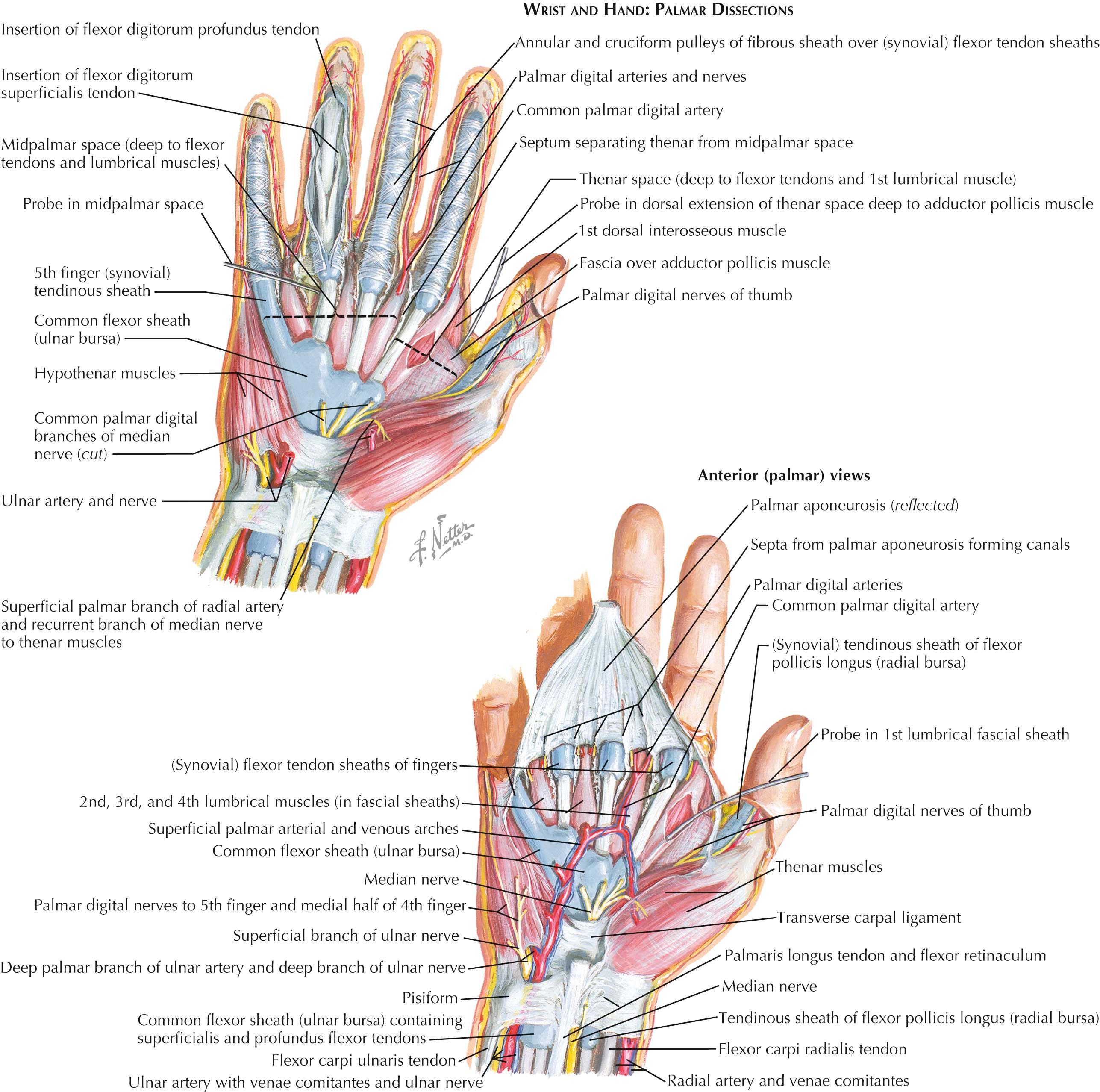
Digital synovial sheaths, after a gap in the midpalm, pick up over the heads of the metacarpals and continue over the pairs of tendons to the base of the distal phalanges of the second to fourth digits. Except for about 5 mm of their proximal ends, these synovial sheaths (and the tendons) are contained within the fibrous sheaths of the digits of the hand. The fibrous sheaths of the digits are strong coverings of the flexor tendons, which extend from the heads of the metacarpals to the base of the distal phalanges and serve to prevent “bowstringing” of the tendon away from the bones during flexion. They attach along the borders of the proximal and middle phalanges, the capsules of the interphalangeal joints, and the palmar surface of the distal phalanx. They form strong semicylindrical sheaths that, with the bones, produce fibro-osseous tunnels through which the flexor tendons pass to their insertions. Over the shafts of the proximal and middle phalanges, the sheaths exhibit thick accumulations of transversely running fibers (sometimes called annular ligaments, or pulleys), whereas opposite the joints, an obliquely crisscrossing arrangement is characteristic (cruciate ligaments). These latter portions of the fibrous sheaths are thin and do not interfere with flexion at the joints. Proximally, the digital slips of the palmar aponeurosis attach to the fibrous digital sheaths.
The tendons of the flexor digitorum profundus muscle insert on the bases of the distal phalanges of digits 2 to 5, while the tendons of the flexor digitorum superficialis muscle end on the shafts of the middle phalanges of these digits. It is thus necessary for the tendons of the flexor digitorum profundus muscle to pass those of the flexor digitorum superficialis muscle, and this is accomplished by a splitting of the tendon of the superficialis to allow that of the profundus to pass distalward. The division of the flexor digitorum superficialis tendon takes place over the proximal phalanx, and the two halves separate and roll in under the flexor digitorum profundus tendon to reach the bone of the middle phalanx, their fibers crisscrossing as they attach to that phalanx.
The vincula tendinum spring from the internal surface of the digital sheaths of these muscles. They are folds of synovial membrane strengthened by some fibrous tissue, which conduct blood vessels to the tendons. The smaller vinculum breve is at the distal end of the sheath; the vincula longa are narrow strands that reach the tendons more proximally.
The lumbrical muscles are four small, cylindrical muscles associated with the tendons of the flexor digitorum profundus muscle. The two lateral muscles arise distal to the flexor retinaculum from the radial sides and palmar surfaces of the flexor digitorum profundus muscle destined for the second and third digits. These are supplied by the median nerve. The two medial muscles arise from the contiguous sides of the tendons for the third and fourth and the fourth and fifth digits. These are innervated by the deep branch of the ulnar nerve. Each lumbrical tendon passes distalward on the palmar side of the deep transverse metacarpal ligament and then shifts toward the dorsum. It inserts, at the level of the proximal phalanx, into the radial border of the expansion of the extensor digitorum muscle.
The four tendons of the extensor digitorum muscle of the forearm pass across the metacarpophalangeal joints, become flattened and closely attached to the joint capsules, and substitute as dorsal ligaments for these capsules. At the metacarpophalangeal joint and over the proximal two phalanges, an extensor expansion is formed for each tendon by the participation of the tendons of the lumbrical and interosseous muscles of the hand. Opposite the metacarpophalangeal joints, a band of fibers passes from each side of the digital extensor tendon anteriorly on both sides of the joint and attaches to the palmar ligament of the joint. This proximal spreading of the extensor expansion appears like a hood of fibers over the metacarpophalangeal joint.
Over the dorsum of the proximal phalanx, the digital extensor tendon divides into three slips. Of these, the central, broader slip passes directly forward and inserts on the dorsum of the middle phalanx. The diverging bundles on either side, the lateral bands, receive and combine with the broadening tendon of a lumbrical muscle on the radial side of the digit, and with interosseous tendons on both sides of the digit. These tendons unite into a common band that proceeds distalward, the bands of the two sides forming a triangular aponeurosis over the distal end of the middle phalanx. The apex of this aponeurosis attaches to the base of the distal phalanx.
Certain forearm muscles participate in movements of the digits. The tendons of the flexor digitorum superficialis and flexor digitorum profundus muscles emerge from the wrist at the distal border of the flexor retinaculum and enter the central compartment of the palm (see Plate 4-9 ). Here, they fan out toward their respective digits, arranged in pairs, superficial and deep. They are invested by the ulnar bursa through the upper part of the palm, except that the extension of the bursa along the tendons for the fifth digit continues to the base of its distal phalanx.
The flexor digitorum superficialis muscle is a flexor of the proximal interphalangeal and metacarpophalangeal joints of the medial four fingers and is the principal flexor of the wrist. The flexor digitorum profundus muscle primarily flexes the terminal phalanx but, continuing to act, also flexes the middle and proximal phalanges. This muscle flexes the digits in slow action, the flexor digitorum superficialis muscle being recruited for speed and against resistance. The extensor digitorum muscle, assisted by the extensors of the index and fifth fingers, is the extensor of the fingers. Interconnecting tendinous bands between the tendons of the third to fifth digits prevent completely independent extension of these digits, but the index finger can be moved quite separately.
The interosseous and lumbrical muscles of the hand are essential for full extension of the digits. The interosseous muscles act most effectively when there is combined metacarpophalangeal flexion and interphalangeal extension, principally producing interphalangeal extension. The lumbrical muscles are silent during total flexion but are very active in extension of the proximal or distal interphalangeal joints and also when these joints are being maintained in extension during metacarpophalangeal flexion.
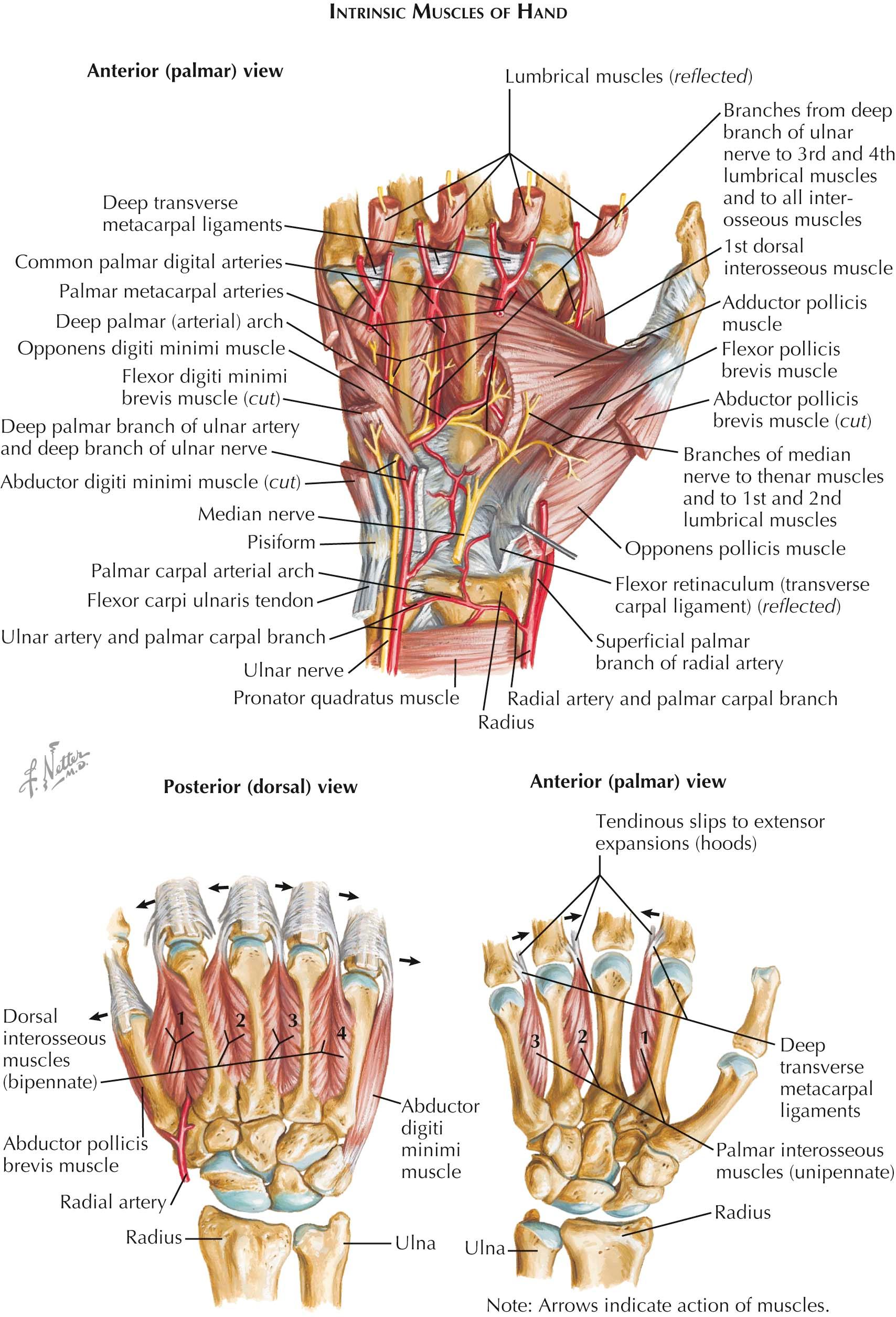
The interosseous muscles occupy the intermetacarpal intervals and are of two types: dorsal and palmar. Each intermetacarpal space contains one palmar and one dorsal interosseous muscle. The four dorsal interosseous muscles are abductors of the digits and are bipennate; the three palmar interosseous muscles are adductors and are unipennate. The plane of reference for abduction and adduction of the fingers is the midplane of the third digit. This is evident on simultaneously spreading and then approximating the extended digits. The placement of these muscles follows from the above considerations of actions and reference plane for abduction and adduction.
A dorsal interosseous muscle lies on either side of the third metacarpal, since any movement of the third digit away from its plane of reference is abduction. The other two dorsal interosseous muscles occupy the space between the first second metacarpals for the first dorsal muscle and between the fourth and fifth metacarpals for the fourth dorsal muscle. These latter two muscles abduct the second and fourth digits. The bipennate dorsal interosseous muscles arise by two heads from the adjacent sides of the metacarpals between which they lie. The first dorsal interosseous muscle is considerably larger than the others; the radial artery also passes into the palm between its heads. Dorsal perforating arteries pass between the heads of the other muscles.
The smaller palmar interosseous muscles adduct the same digit from whose metacarpal bone they arise and thus take origin from the palmar surfaces of the second, fourth, and fifth metacarpals. The tendons of both the dorsal and the palmar interosseous muscles pass dorsal to the deep transverse metacarpal ligaments between the heads of the metacarpals, and they have two insertions. The first insertion is to the base of the proximal phalanx; it is concerned with the abduction-adduction function. The second insertion is into the extensor expansion of the tendon of the extensor digitorum muscle; it produces flexion at the metacarpophalangeal joints and extension of the middle and distal phalanges at the interphalangeal joints. All the interosseous muscles are innervated by the deep branch of the ulnar nerve.
Free movement of the thumb is most important in the more precise activities of the hand. The flexor pollicis longus muscle flexes the thumb, and the extensor pollicis longus and extensor pollicis brevis muscles extend it. The abductor pollicis longus muscle is an accessory flexor of the wrist; it abducts and extends its metacarpal. The short muscles of the thumb provide flexion, abduction, adduction, and opposition. Abduction of the thumb carries it anteriorly out of the plane of the palm because of the rotated position of the first metacarpal, which directs its palmar surface medially. The abductor pollicis brevis muscle also assists in flexion. The opponens pollicis muscle acts solely on the metacarpal of the thumb, drawing the digit across the palm and rotating it medially.
The components of opposition are abduction, flexion, and medial rotation, the tip of the thumb reaching contact with the pads of the other slightly flexed digits. In firm grasp, the flexor pollicis brevis muscle is especially active. The motor, or recurrent, branch of the median nerve innervates the three muscles involved. The adductor pollicis muscle adducts the thumb. The abductor digiti minimi and the flexor digiti minimi brevis muscles produce their characteristic movements. The opponens digiti minimi muscle rotates the fifth metacarpal medially and deepens the hollow of the hand.
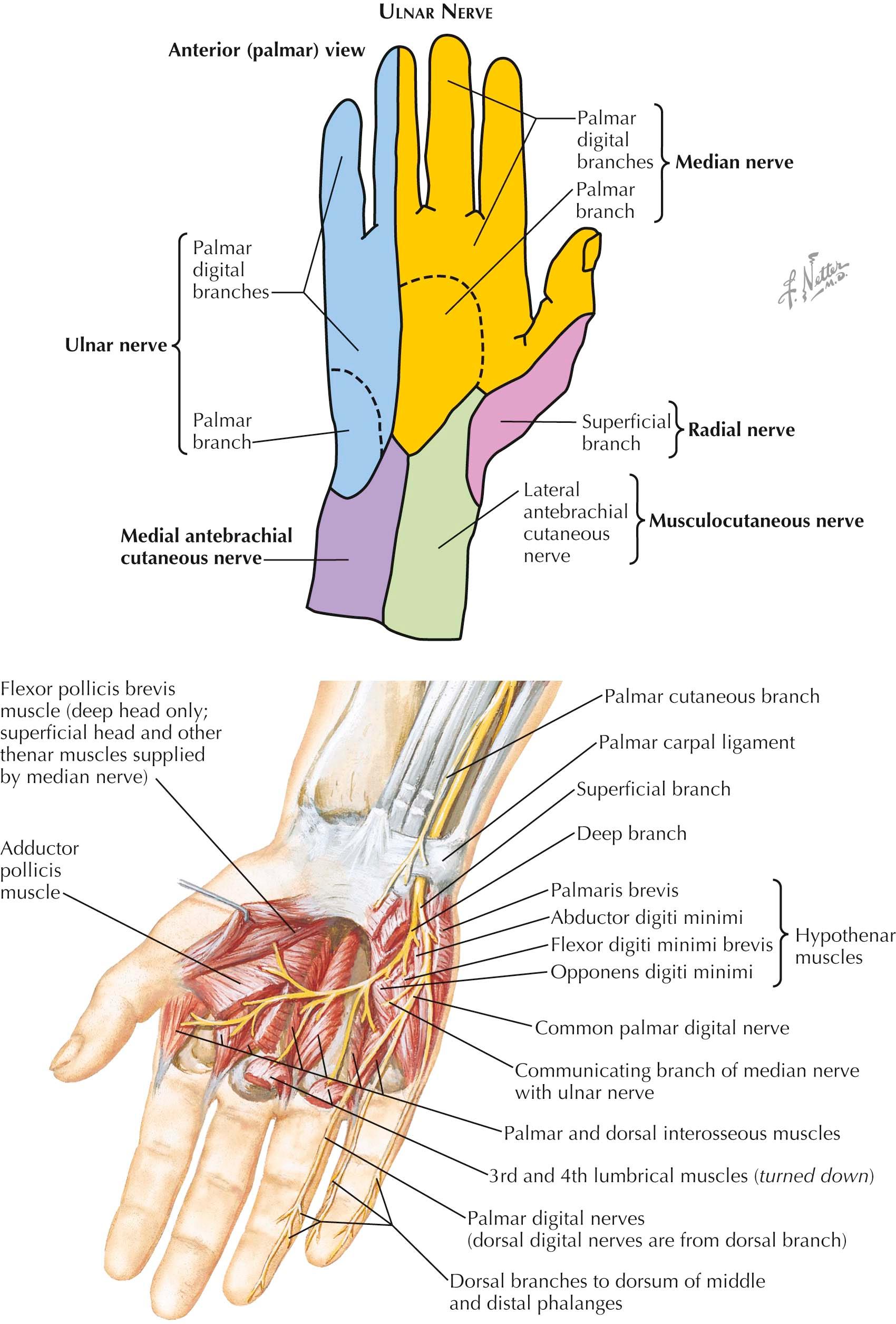
The intrinsic muscles of the hand are palmar and are therefore innervated by either the median or the ulnar nerve. Specific sets of muscles of the thumb and little finger, respectively, occupy the thenar and hypothenar compartments.
Each compartment contains an abductor, an opponens, and a flexor muscle for its specific digit (abductor pollicis brevis, flexor pollicis brevis, opponens pollicis, abductor digiti minimi, flexor digiti minimi brevis, and opponens digiti minimi muscles). In each compartment, the positions and attachments of these muscles are similar. The flexor retinaculum and the bones to which it attaches (the scaphoid and trapezium radially and the hamate and pisiform on the ulnar side) provide the sites of origin for these muscles. The insertions of comparable muscles on the two sides are also the same: the base of the proximal phalanx for the abductor and flexor muscles and the shaft of the metacarpal for the opponens muscles.
The central compartment contains four slender lumbrical muscles associated with the flexor digitorum profundus tendon. The interosseous muscles located in the intervals between the metacarpals occupy, with the adductor pollicis muscle, a deeply placed interosseous-adductor compartment that is bound by the dorsal and palmar interosseous fasciae. To complete these generalizations, the rule of nervous innervation may also be stated: the median nerve supplies the abductor pollicis brevis, opponens pollicis, flexor pollicis brevis, and the most radial two lumbrical muscles; the ulnar nerve supplies all the other intrinsic muscles of the hand.
The adductor pollicis muscle has two heads of origin, separated by a gap through which the radial artery enters the palm. The oblique head arises from the capitate and from the bases of the second and third metacarpals. The transverse head arises from the palmar ridge (shaft) of the third metacarpal. The two heads insert together by a tendon that ends in the ulnar side of the base of the proximal phalanx of the thumb.
This tendon usually contains a sesamoid that together with the sesamoid in the tendon of the flexor pollicis brevis muscle forms a pair of small sesamoids on either side of the tendon of the flexor pollicis longus muscle. The adductor pollicis muscle overlies the interosseous muscles on the radial side of the third metacarpal. This muscle is supplied by the deep branch of the ulnar nerve.
Friction between tendons and compartments or bony surfaces is reduced by synovial sheaths. A sheath is formed like a double-walled tube: the delicate inner wall is closely applied to the tendon, and the outer wall is the lining of the compartment in which the tendon lies. The layers are continuous with each other at the ends of the tube (as elsewhere); their facing surfaces are smooth and separated by a small amount of synovial fluid.
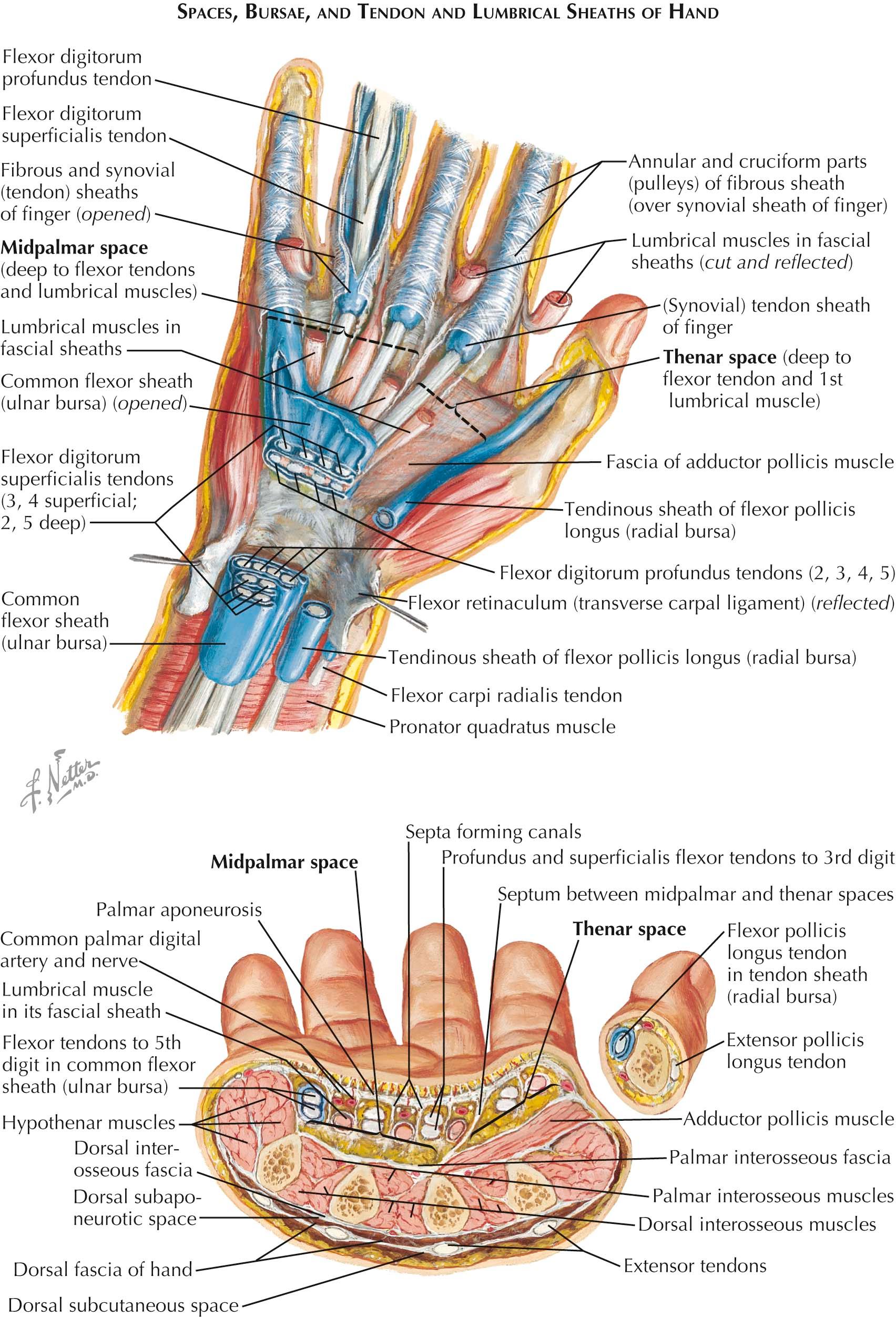
In the hand, the flexor tendons have significant excursion, which causes friction between the tendons and the carpal ligament and in each finger against the fibro-osseous pulley system during gripping activities. Accordingly, the tendons to the thumb and fingers are protected and lubricated for optimal movement. Variations in the anatomy of the synovial sheaths (bursae) exist and have an impact on the pattern of presentation of infections when they occur (see Plates 4-37 and 4-38 ). Similarly, several potential spaces exist in the palm and can become sites of infection. The thenar space exists just anterior to the adductor pollicis muscle. The midpalmar space exists posterior (deep) to the central compartment that contains the long flexor tendons and lumbrical muscles.
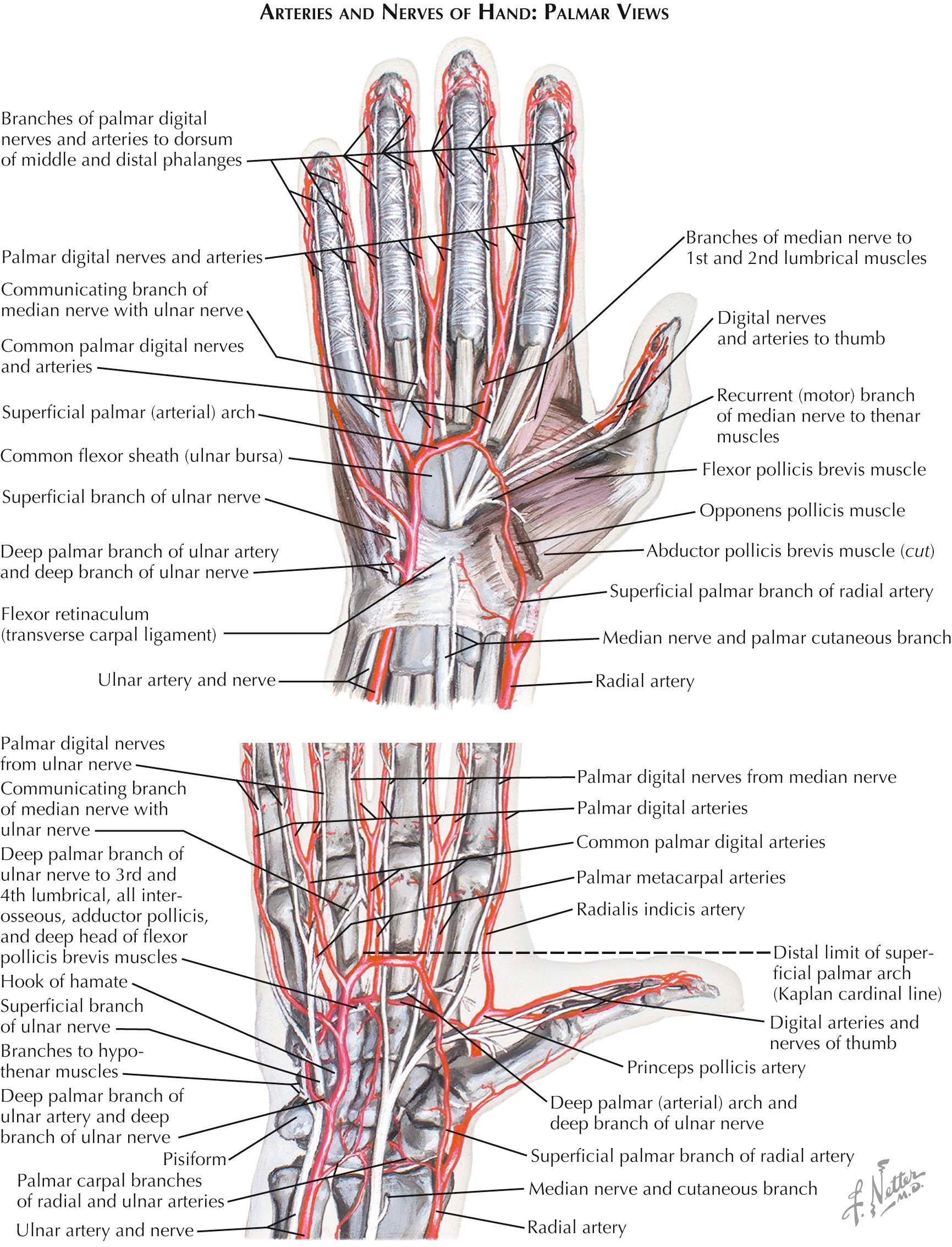
The ulnar artery, with its accompanying nerve, enters the hand superficial to the flexor retinaculum and to the radial side of the pisiform (see Plates 4-10 and 4-11 ). It descends, curving radially, to about the midpalm and there anastomoses with the superficial palmar branch of the radial artery. This branch passes across or through the muscles of the thenar eminence, supplies this group of muscles, and emerges medial to the eminence to help form the superficial palmar arterial arch. The arch is convex distalward and crosses the palm at the level of the line of the completely abducted thumb.
The branches of the superficial arch supply the medial three and one-half digits; the radial one and one-half digits are supplied from the deep palmar arterial arch. The superficial arch gives origin to three common palmar digital arteries, which proceed distalward on the flexor tendons and lumbrical muscles and superficial to the digital nerves of the palm. They unite at the webs of the fingers with the palmar metacarpal arteries and with distal perforating branches of the dorsal metacarpal arteries. From the short trunks thus formed spring proper palmar digital arteries.
Two proper palmar digital arteries run distalward along the adjacent margins of the second to fifth digits. A proper digital branch to the ulnar side of the fifth digit arises from the ulnar artery in the hypothenar compartment. At the webs of the fingers, the digital nerves cross the arteries to become superficial to them along the margins of the digits. Thus, in each digit, the palmar and dorsal digital arteries lie within the span of the corresponding cutaneous nerves. The proper palmar digital arteries anastomose to form terminal plexuses in the fingers. They also give off branches that supply the last two dorsal segments of the digits.
At the wrist, the radial artery shifts from the expanded palmar surface of the radius, through the floor of the anatomic snuffbox, to reach the dorsum of the hand at the proximal end of the first dorsal interosseous space. As it passes under the tendon of the abductor pollicis longus muscle, it gives origin to its dorsal carpal branch; continuing distally over the first dorsal interosseous space, it gives origin to the first dorsal metacarpal artery. (The radial artery then turns deeply into the palm of the hand and participates in forming the deep palmar arterial arch.) The dorsal carpal branch of the radial artery passes ulnarward across the distal row of carpal bones and under the extensor tendons and joins the dorsal carpal branch of the ulnar artery. Thus is formed the dorsal carpal arterial arch.
Three dorsal metacarpal arteries descend from this arch on the dorsal interosseous muscles of the second, third, and fourth intermetacarpal intervals, respectively. Opposite the heads of the metacarpals, these vessels divide into proper dorsal digital arteries, which proceed distally along the dorsal borders of contiguous digits. These vessels are small and fail to reach the distal phalanges of the digits. Anastomoses are formed between the dorsal metacarpal arteries and the palmar arterial system in two locations: by perforating branches at the bases of the metacarpals and at the division into proper dorsal digital arteries.
The deep palmar arterial arch is formed by the junction of the terminal portion of the radial artery and the deep branch of the ulnar artery. The radial artery enters the palm at the base of the first intermetacarpal space by penetrating between the two heads of origin of the first dorsal interosseous muscle. Passing then between the transverse and oblique heads of the adductor pollicis muscle, it joins the deep branch of the ulnar artery.
The princeps pollicis artery arises from the radial artery as it emerges from the first dorsal interosseous muscle. At the head of the first metacarpal, it provides two proper palmar digital branches for the thumb. The radialis indicis artery arises with the princeps pollicis to run along the radial side of the index finger. It is a proper digital artery to the radial side of the index finger.
From the convexity of the arch arise three palmar metacarpal arteries. These descend under the palmar interosseous fascia of the second to fourth intermetacarpal intervals. At the webs of the fingers, they join the common digital arteries from the superficial arch. Recurrent carpal branches are small. They ascend to and help form the palmar carpal network. Perforating branches anastomose with the dorsal metacarpal arteries on the dorsum of the hand.
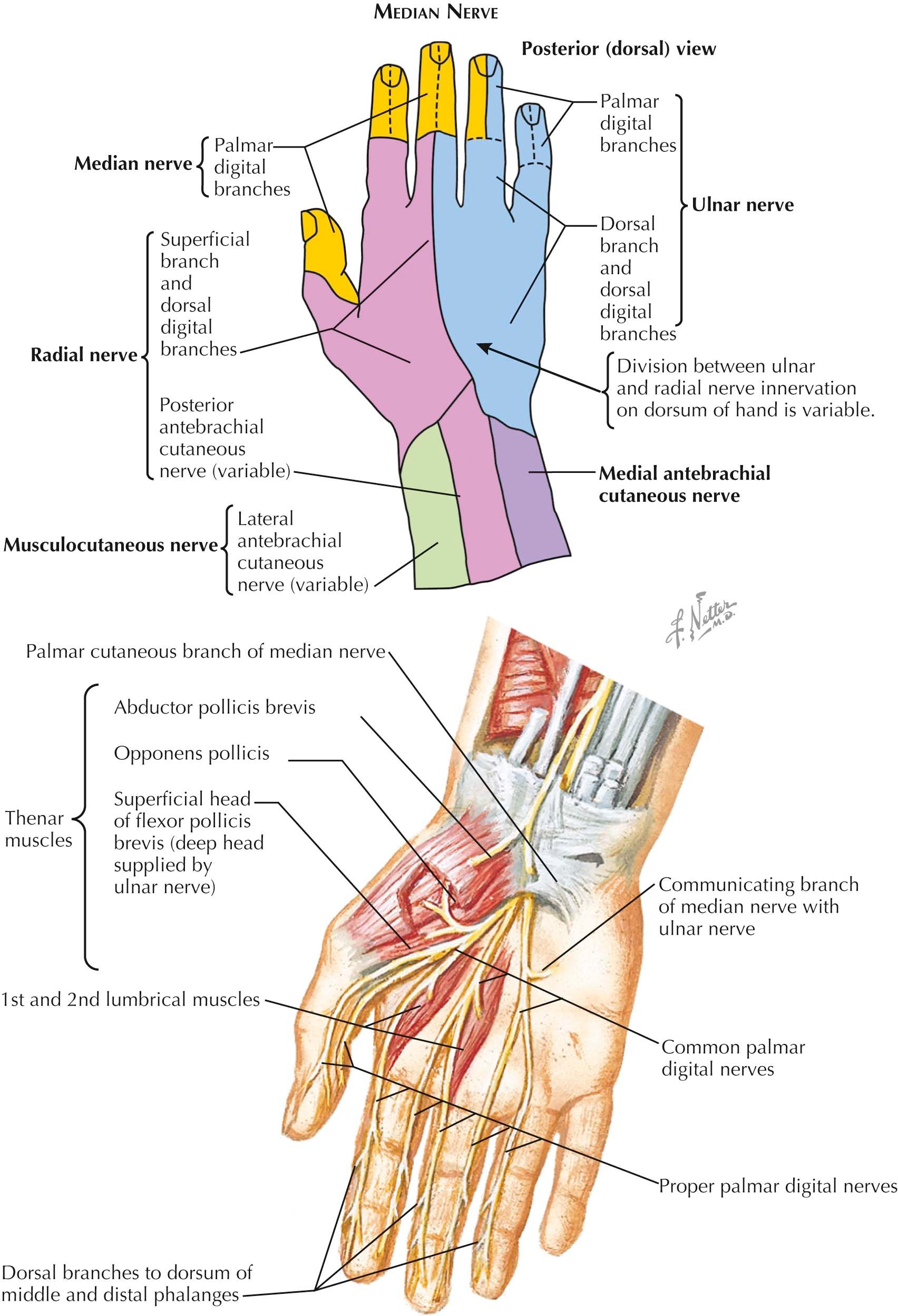
Nerve branches from the ulnar, median, and radial nerve supply motor, sensory, and autonomic vasomotor function in the hand.
The ulnar nerve (C[7], 8; T1) is the main continuation of the medial cord of the brachial plexus. In the forearm and hand, the ulnar nerve gives off articular, muscular, palmar, dorsal, superficial and deep terminal, and vascular branches. It divides into branches for the areas of skin on the medial side of the back of the hand and fingers (see Plate 4-12 ). The ulnar nerve enters the hand to the radial side of the pisiform between the palmar carpal ligament and the flexor retinaculum. Just distal to the pisiform, the ulnar nerve divides into superficial and deep branches.
The superficial terminal branch supplies the palmaris brevis muscle, innervates the skin on the medial side of the palm, and gives off two palmar digital nerves. The first is the proper palmar digital nerve for the medial side of the small finger; the second, the common palmar digital nerve, communicates with the adjoining common palmar digital branch of the median nerve before dividing into the two proper palmar digital nerves for the adjacent sides of the small and ring fingers. Rarely, the ulnar nerve supplies two and one-half rather than one and one-half digits, and the areas supplied by the median and radial nerves are reciprocally reduced.
The deep terminal branch of the ulnar nerve, with the deep branch of the ulnar artery, sinks between the origins of the abductor digiti minimi and the flexor digiti minimi brevis muscles and perforates the origin of the opponens digiti minimi muscle. It supplies these muscles and then curves around the hamulus of the hamate into the central part of the palm of the hand in conjunction with the deep palmar arterial arch. As it crosses the hand deep to the flexor tendons to the digits, the nerve gives twigs to the ulnar two lumbrical muscles and to all the interosseous muscles, both dorsal and palmar. It then supplies the adductor pollicis muscle and gives articular twigs to the wrist joint, and it may send a terminal branch into the deep head of the flexor pollicis brevis muscle.
Variations in the nerve supplies of the palmar muscles are as common as the variations in the cutaneous distribution; they are due to the variety of interconnections between the ulnar and median nerves.
The dorsal branch of the ulnar nerve completes the cutaneous supply of the dorsum of the hand and digits. It arises about 5 cm above the wrist, passes dorsalward from beneath the flexor carpi ulnaris tendon, and then pierces the forearm fascia. At the ulnar border of the wrist, the nerve divides into three dorsal digital branches. There are usually two or three dorsal digital nerves, one supplying the medial side of the small finger, the second splitting into proper dorsal digital nerves to supply adjacent sides of the small and ring fingers, and the third (when present) supplying contiguous sides of the ring and long fingers.
The first branch courses along the ulnar side of the dorsum of the hand and supplies the ulnar side of the small finger as far as the root of the nail. The second branch divides at the cleft between the ring and small fingers and supplies their adjacent sides. The third branch may divide similarly; it may supply the adjacent sides of the long finger and ring finger, or it may simply anastomose with the fourth dorsal digital branch of the superficial branch of the radial nerve. The dorsal branches to the ring finger usually extend only as far as the base of the second phalanx, with the more distal parts of the ring and small finger supplied by palmar digital branches of the ulnar nerve.
The palmar branch of the ulnar nerve arises about the middle of the forearm, descending under the antebrachial fascia in front of the ulnar artery. It perforates the fascia just above the wrist and supplies the skin of the hypothenar eminence and the medial part of the palm.
The median nerve (C[5], 6, 7, 8; T1) is formed by the union of medial and lateral roots arising from the corresponding cords of the brachial plexus (see ( Plate 1-18 ).
The palmar branch of the median nerve arises just above the wrist (see Plate 4-13 ). It perforates the palmar carpal ligament between the tendons of the palmaris longus and flexor carpi radialis muscles and distributes to the skin of the central depressed area of the palm and the medial part of the thenar eminence.
The digital branches of the median nerve, the proper palmar digital nerves, lie subcutaneously along the margins of each of the digits distal to the webs of the fingers (see Plates 4-12 and 4-13 ). They arise from common palmar digital nerves, which lie under the dense palmar aponeurosis of the central palm. The first common palmar digital nerve gives rise to the muscular branch to the short muscles of the thumb and then divides into three proper palmar digital nerves. Just distal to the flexor retinaculum, its motor, or recurrent, branch curves sharply into the thenar eminence and supplies the abductor pollicis brevis, flexor pollicis brevis (sometimes only its superficial head), and opponens pollicis muscles. This branch frequently arises from the median nerve together with its first common digital branch. The first common digital branch then runs to the radial and ulnar sides of the thumb, giving numerous branches to the pad and small, dorsally running branches to the nail bed of the thumb. The third proper digital branch supplies the radial side of the index finger. The second common palmar digital branch provides two proper palmar digital nerves, which reach the adjacent sides of the index and long fingers. The third common palmar digital nerve communicates with a digital branch of the ulnar nerve in the palm and divides into two proper palmar digital nerves supplying adjacent sides of the long finger and ring fingers.
Proper palmar digital nerves are large because of the density of nerve endings in the fingers. They lie superficial to the corresponding proper palmar digital arteries and veins. As each nerve passes toward its termination in the pad of the finger, it gives off branches for the innervation of the skin of the dorsum of the digits and the matrices of the fingernails. These dorsal branches innervate the dorsal skin of the distal segment of the index finger, the two terminal segments of the long finger, and the radial side of the ring finger. The common and proper palmar digital nerves vary in their origins and distributions, but the usual arrangement innervates the skin (including the nail beds) over the distal and dorsal aspects of the lateral three and one-half digits. Occasionally, they supply only two and one-half digits. The proper palmar digital branches to the radial side of the index finger and to the contiguous sides of the index and long fingers also carry motor fibers to supply the first and second lumbrical muscles, respectively. Therefore, the digital nerves are not concerned solely with cutaneous sensibility. They contain an admixture of efferent and afferent somatic and autonomic fibers, which transmit impulses to and from sensory endings, vessels, sweat glands, and arrectores pilorum muscles and between fascial, tendinous, osseous, and articular structures in their areas of distribution.
Dorsally the superficial branch pierces the deep fascia and commonly subdivides into two branches, which usually split into four or five dorsal digital nerves. The cutaneous area of supply is shown in Plate 4-14 . The smaller lateral branch supplies the skin of the radial side and eminence of the thumb and communicates with the lateral antebrachial cutaneous nerve. The larger medial branch divides into four dorsal digital nerves. The first dorsal digital nerve supplies the ulnar side of the thumb; the second supplies the radial side of the index finger; the third distributes to the adjoining sides of the index and long fingers; and the fourth supplies the adjacent sides of the long and ring fingers.
There is usually an anastomosis on the back of the hand between the superficial branch of the radial nerve and the dorsal branch of the ulnar nerve, and there is some variability in the apparent source of the last (more median) branch of either nerve. In some such cases, the adjacent sides of the long and ring fingers are in the territory of the ulnar nerve. Dorsal digital nerves fail to reach the extremities of the digits. They reach to the base of the nail of the thumb, to the distal interphalangeal joint of the index finger, and not quite as far as the proximal interphalangeal joints of the long and ring fingers. The distal areas of the dorsum of the digits not supplied by the radial nerve receive branches from the stout palmar digital branches of the median nerve.
The dorsal digital nerves also supply filaments to the adjacent vessels, joints, and bones. (Note that the dorsal digital nerves extend only to the levels of the distal interphalangeal joints and that the first dorsal digital nerve gives off a twig that curves around the radial side of the thumb to supply the skin over the lateral part of the thenar eminence.)
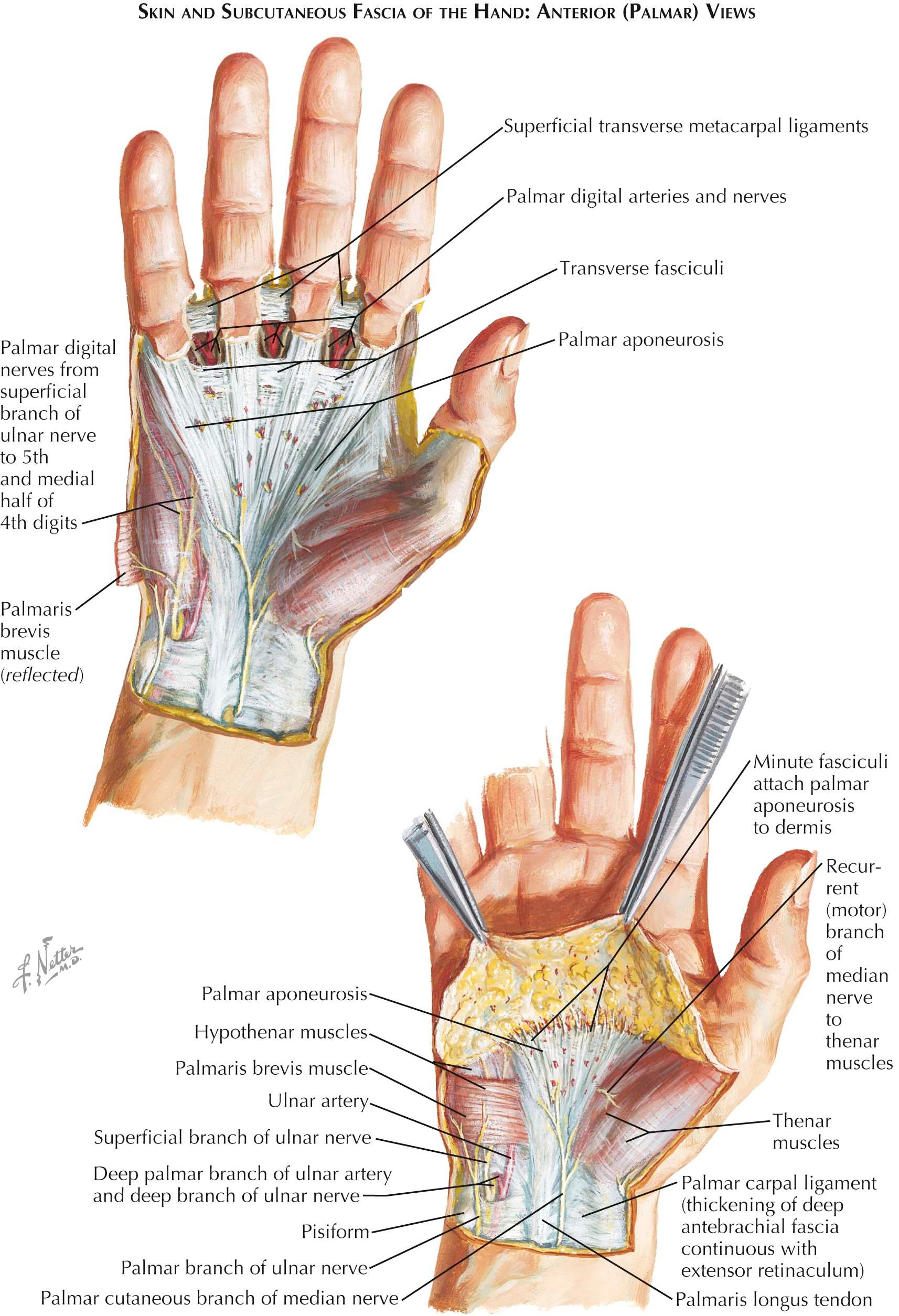
The fascia of the palm of the hand is continuous with the antebrachial fascia of the flexor aspect of the forearm and with the palmar carpal ligament. At the borders of the hand, it is continuous with the fascia of the dorsum at attachments to the first and fifth metacarpals. The hypothenar fascia invests the muscles of the little finger and bounds the hypothenar compartment of the hand by means of a palmar attachment to the radial side of the fifth metacarpal. In a similar manner, the fascia over the thumb muscles dips deeply to attach to the palmar aspect of the first metacarpal and bounds, with the metacarpal, a thenar compartment in the hand. The central compartment of the palm is covered by the intervening part of the fascia of the palm, but this portion is reinforced superficially by the palmar aponeurosis, an expansion of the tendon of the palmaris longus muscle.
Recognizable in the palmar aponeurosis are a superficial stratum of longitudinally running fibers (which is continuous with the tendon of the palmaris longus muscle) and a deeper layer of transverse fibers. The transverse fibers are continuous with the thenar and hypothenar fasciae; proximally, they are continuous with the flexor retinaculum and the transverse carpal ligament. The palmar aponeurosis broadens distally in the palm and divides into four digital slips, some of its fibers meanwhile attaching to the overlying skin at the skin creases of the palm. The central parts of these slips pass into the digits, attaching superficially to the skin of the crease at the base of each digit; deeply, they attach to the fibrous sheath of the digit. The marginal fibers sink deeply between the heads of the metacarpals and attach to the metacarpophalangeal joint capsules, the deep transverse metacarpal ligaments, and the proximal phalanges of the digits. There is usually no digital slip for the thumb, but longitudinal fibers of the aponeurosis usually curve over onto the thenar fascia.
The deep attachments of the margins of the digital slips of the palmar aponeurosis define the entrance to the fibrous sheath of each digit, but they are also continued proximally into the palm for varying distances. They attach to the palmar interosseous fascia and to the shafts of the metacarpals, thus providing communicating subcompartments for each pair of flexor tendons and the associated lumbrical muscles (see Plate 4-15 ). The septum reaching the third metacarpal is stronger and more constant; it separates a surgical thenar space under the aponeurosis to its radial side and a midpalmar space to its ulnar side.
Accumulations of the deeper transverse fibers of the aponeurosis appear between the diverging digital slips. Located at the level of the heads of the metacarpals, these fibers are designated as the superficial transverse metacarpal ligament. Distally, the webs of the fingers are reinforced by another accumulation of transverse fibers designated as transverse fasciculi.
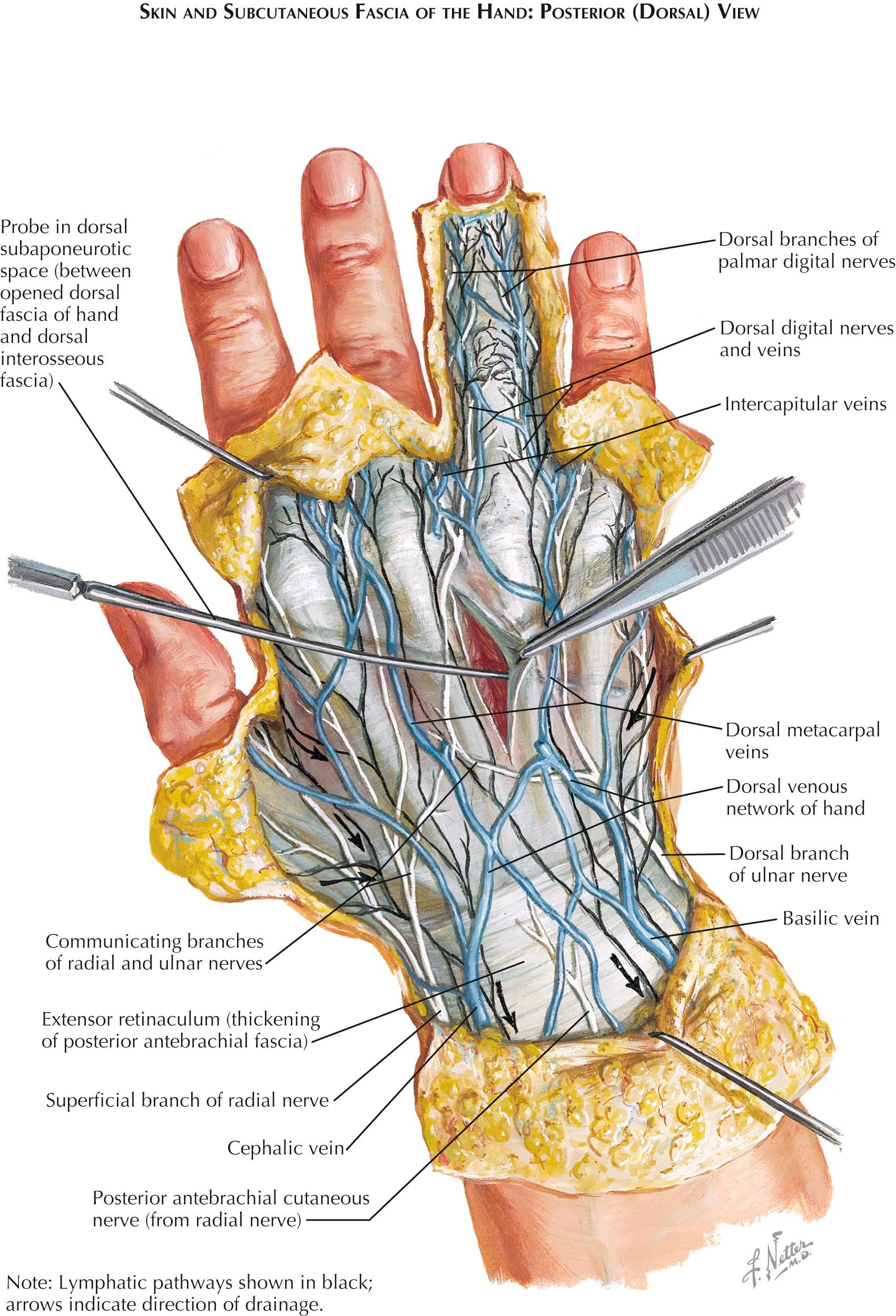
The fascia of the dorsum of the hand is continuous with the antebrachial fascia of the extensor surface of the forearm and with the extensor retinaculum. It encloses the tendons of the extensor muscles as they pass to the digits and continues into the extensor expansions on the dorsum of the digits; deep to it is a subaponeurotic space. This interfascial cleft separates the fascia of the dorsum from the deeper dorsal interosseous fascia covering the dorsal interosseous muscles and the descending branches of the dorsal carpal arterial arch (see Plate 4-16 ).
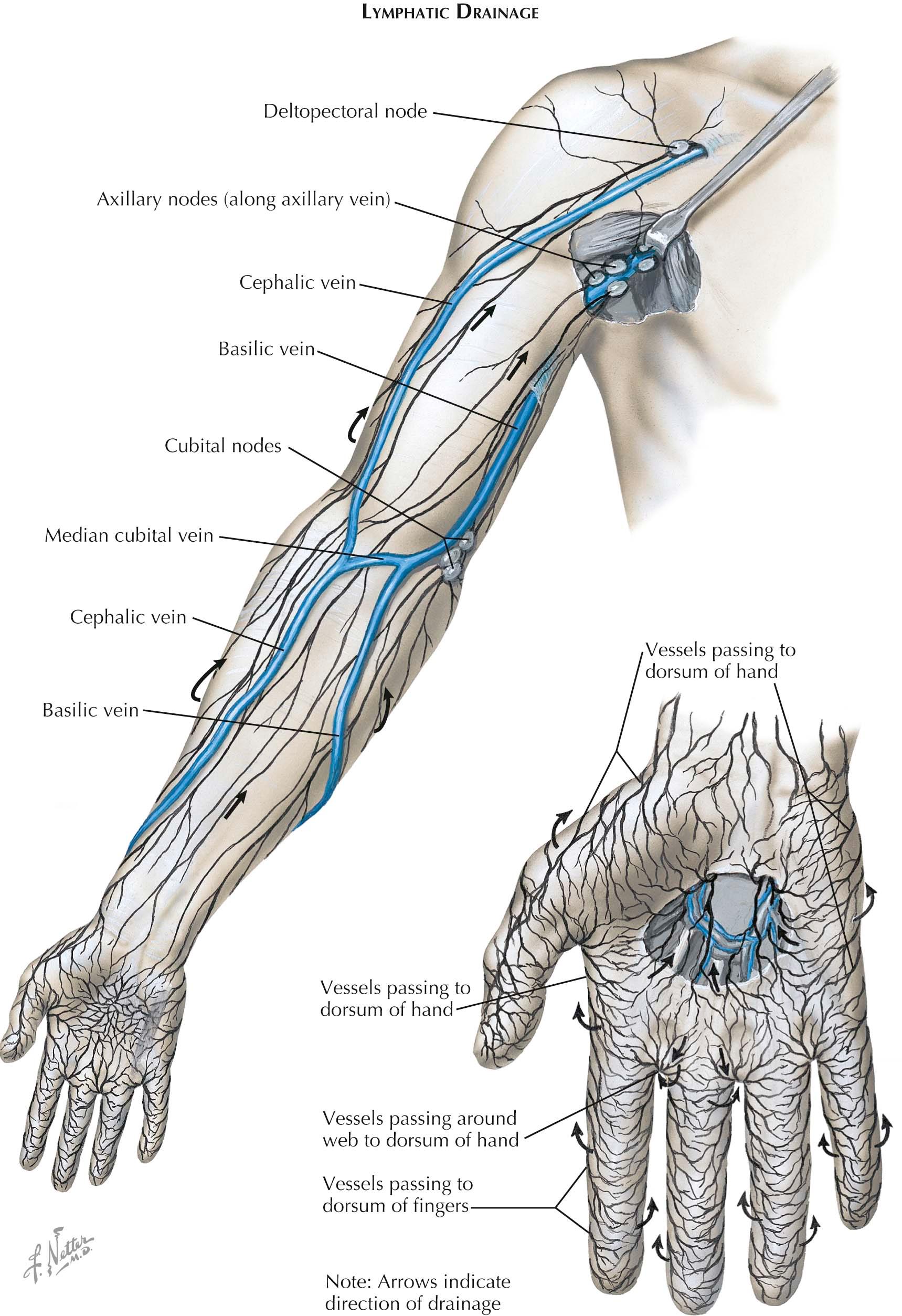
The superficial lymphatic vessels of the upper limb begin in the hand and pervade the skin and subcutaneous tissues (see Plates 4-16 and 4-17 ). The dense digital lymphatic plexuses are drained by channels accompanying the digital arteries. At the interdigital clefts (and also more distally), collecting vessels of the palmar surfaces of the fingers pass to join dorsal collecting vessels and empty into the plexus of the dorsum of the hand.
Drainage of the thumb, index finger, and radial portion of the third finger is by collecting vessels that ascend along the radial side of the forearm; channels draining the ulnar fingers ascend along the ulnar side. Vessels from the lymphatic plexus of the palm radiate to the sides of the hand and also upward through the wrist, coalescing into two or three collecting vessels that ascend in the middle of the anterior surface of the forearm. The radial and ulnar channels turn onto the anterior surface of the forearm, lying parallel to the middle group, and all continue subcutaneously through the forearm and arm to reach the axillary nodes.
Some of the ulnar lymphatic channels are efferent to the cubital lymph nodes. This superficial group of one or two nodes is located 3 to 4 cm above the medial epicondyle of the humerus and below the aperture in the brachial fascia for the basilic vein. The afferent vessels of these nodes include channels originating in the ulnar three fingers and the ulnar portion of the forearm. The efferent vessels accompany the basilic vein under the brachial fascia and reach the lateral and central groups of axillary lymph nodes.
Several lymphatic channels collecting from the dorsal surface of the arm follow the upper course of the cephalic vein to the deltopectoral triangle, perforate the costocoracoid membrane with the vein, and terminate in an apical node of the axillary group. In about 10% of cases, this channel is interrupted in the deltopectoral triangle by one or two small deltopectoral nodes.
The axillary lymph nodes, usually large and numerous, are arranged in five subgroups, some related to the axillary walls and others to vessels.
A lateral group of three to five nodes lies medial and posterior to the distal segment of the axillary vein. These nodes are in the direct line of lymph drainage from the upper limb, except for the drainage lymphatics along the cephalic vein. Efferent vessels from these nodes drain to the central and apical nodes.
A pectoral group is located along the lateral thoracic artery adjacent to the axillary border of the pectoralis minor muscle. These three to five nodes receive the lymphatic drainage of the anterolateral part of the thoracic wall, including most of the lateral drainage from the mammary gland, and of the skin and muscles of the supraumbilical part of the abdominal wall. Efferent lymphatic vessels reach the central and apical groups.
A subscapular group of five or six nodes is stretched along the subscapular blood vessels, from their origin in the axillary vessels to their contact with the chest wall. These nodes drain the skin and muscles of the posterior thoracic wall and shoulder region and also the lower part of the back of the neck. Their efferent lymph channels pass to the central axillary nodes.
A central group of four or five nodes lies under the axillary fascia, embedded in its fat. Among the largest of the axillary nodes, these nodes receive some lymphatic vessels directly from the arm and mammary regions; but primarily, they receive lymph from the lateral, pectoral, and subscapular groups. Their efferent channels pass to the apical nodes.
The apical group, consisting of 6 to 12 nodes, lies along the axillary vein at the apex of the axilla and adjacent to the superior border of the pectoralis minor muscle. The apical nodes receive efferent vessels of all other axillary groups, lymphatic vessels that accompany the cephalic vein, and lymphatic vessels from the mammary gland. From lymph vessels interconnecting the apical nodes arises a larger common channel, the subclavian lymphatic trunk.
These vessels serve the upper limb, draining joint capsules, periosteum, tendons, nerves, and, to a lesser extent, muscles. Collecting vessels accompany the major arteries, along whose paths lie small intercalated lymph nodes. The deep lymphatics are afferent to the central and lateral axillary nodes.
The subcutaneous veins of the limb are interconnected with the deep veins of the limb via perforating veins. Certain prominent veins, unaccompanied by arteries, are found in the subcutaneous tissues of the limbs. The cephalic and basilic veins, the principal superficial veins of the upper limb, originate in venous radicals in the hand and digits.
Anastomosing longitudinal palmar digital veins empty at the webs of the fingers into longitudinally oriented dorsal digital veins. The dorsal veins of adjacent digits then unite to form relatively short dorsal metacarpal veins, which end in the dorsal venous arch. The radial continuation of the dorsal venous arch is the cephalic vein , which receives the dorsal veins of the thumb and then ascends at the radial border of the wrist. In the forearm, it tends to ascend at the anterior border of the brachioradialis muscle, with tributaries from the dorsum of the forearm. In the cubital space, the obliquely ascending median cubital vein connects the cephalic and basilic veins. Above the cubital fossa, the cephalic vein runs in the lateral bicipital groove and then in the interval between the deltoid and pectoralis major muscles, where it is accompanied by the small deltoid branch of the thoracoacromial artery. At the deltopectoral triangle, the cephalic vein perforates the costocoracoid membrane and empties into the axillary vein. An accessory cephalic vein passes from the dorsum of the forearm spirally laterally to join the cephalic vein at the elbow.
The basilic vein continues the ulnar end of the venous arch of the dorsum of the hand (see Plate 4-17 ). It ascends along the ulnar border of the forearm and enters the cubital fossa anterior to the medial epicondyle of the humerus. After receiving the median cubital vein, the basilic vein continues upward in the medial bicipital groove, pierces the brachial fascia a little below the middle of the arm, and enters the neurovascular compartment of the medial intermuscular septum, where it lies superficial to the brachial artery. In the distal axilla, it joins the brachial veins to form the axillary vein.
The median antebrachial vein is a frequent collecting vessel of the middle of the anterior surface of the forearm. It terminates in the cubital fossa in the median cubital vein or in the basilic vein. It sometimes divides into a median basilic vein and a median cephalic vein, which borders the biceps brachii laterally and joins the cephalic vein. The median antebrachial vein may be large or absent.
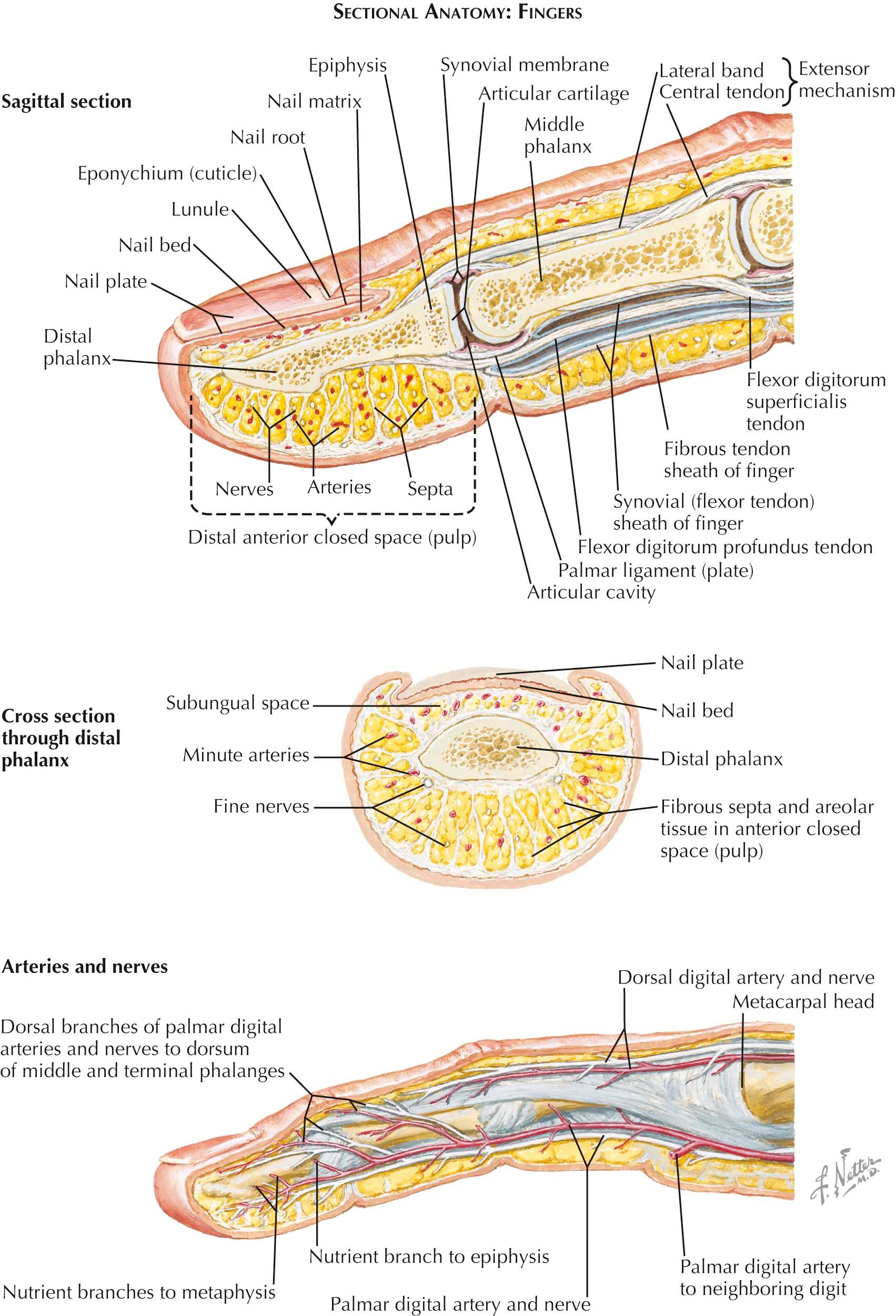
The specializations of the fingers frequently have clinical importance. The bones, joints, and tendon attachments of the fingers have already been described. It remains to add other specific items of interest or importance (see Plate 4-18 ).
The fingernail is an approximately rectangular horny plate, the nail plate, composed of closely welded, horny scales, or cornified epithelial cells. Its semitransparency allows the pink of the highly vascular nail bed to show through. The nail is partially surrounded by a fold of skin, the nail wall, and adheres to the subjacent nail bed where strong fibers pass to the periosteum of the distal phalanx, providing the firm attachment necessary for the prying and scratching functions of the nail. The nail is formed from the proximal part of the nail bed, where the epithelium is particularly thick and extends as far distally as the whitened lunula. Developing from this nail matrix, the nail moves out over the longitudinal dermal ridges of the nail bed at a growth rate of approximately 1 mm/wk. Sensory nerve endings and blood vessels are abundant in the nail bed.
To the palmar aspect of the distal phalanx lies the anterior closed space. Areolar tissue of mixed forms lies in this region. Fiber bundles surround fatty collections and support the finer arterial and nerve branching. More discrete septa of connective tissue fibers pass from the periosteum of the distal phalanx to blend with the underside of the dermis. An especially abundant collection of fibers attaches to form the distal skin crease of the finger and thus serves to bound the anterior closed space of the finger pad. More proximally at the level of the proximal and distal interphalangeal joints the palmar skin is held fast by Cleland and Grayson ligaments during flexion and extension.
The general origin and distribution of the dorsal and palmar digital arteries have been fully discussed (see Plate 4-18 ), and it has been emphasized that the palmar digital arteries are the major arteries, since they send dorsal terminal branches over the distal and middle phalanges to supply the dorsum of the fingers and thumb. The dorsal digital arteries are poorly developed, except in the thumb. The proper palmar arteries are not necessarily of equal size on the two sides of the digit, although they are essentially so for the middle and ring fingers. However, in the thumb and the index and fifth digits, the larger artery is on the median side of the digit; the more diminutive artery is on the opposite side.
These proper palmar digital arteries have cross anastomoses or transverse interconnections. There is a pair of proximal transverse digital arteries that anastomoses at the level of the neck of the proximal phalanx; a pair of distal transverse digital arteries also anastomoses at the level of the neck of the middle phalanx. These arteries run close to the bone and deep to the flexor tendons. There is a rich terminal anastomosis of the palmar digital arteries, which forms a profuse tuft of small vessels in each finger pad. The proximal edge of this tuft of vessels lies on the palmar surface of the distal phalanx at about its epiphyseal line.
The cutaneous nerves parallel the arteries in course and distribution. In their course along the fingers, the proper digital nerves are outside the arteries; that is, as the digit is viewed from the side, the arteries are within the span of the dorsal and palmar nerves. Cutaneous nerves are of two types. Included are afferent somatic fibers mediating general sensation (pain, touch, pressure, and temperature), and efferent autonomic fibers supplying the smooth muscles, sweat glands, and sebaceous glands.
Both free and encapsulated nerve endings are involved in various sensations. Of the encapsulated endings, the Meissner tactile corpuscles are richly represented in the dermal papillae, and pacinian corpuscles lie in the subcutaneous connective tissue, especially along the sides of the digits and are quickly adapting receptors responsible for moving touch (tested by moving two-point discrimination). The slowly adapting receptors (Merkel cell neurite complexes and Ruffini end organs) respond to static touch (measured by static two-point discrimination or with Semmes-Weinstein monofilament testing). The relatively large size of the proper palmar digital nerves suggests the high density of nerve endings in the fingers, especially in the finger pads. The tactile corpuscles are most numerous in the fingertips, less so on the palm, and rare on the dorsum of the fingers or hand.
The term rheumatic disease refers to any illness characterized by pain and stiffness in or around the joints. These diseases are divided into two main groups: disorders that involve the joints primarily (the different forms of arthritis) and disorders that, although not directly affecting the joints, involve connective tissue structures around the joints (the periarticular disorders, or nonarticular rheumatism). The many types of arthritis and nonarticular disorders differ from one another in etiology, pathogenesis, pathology, and clinical features.
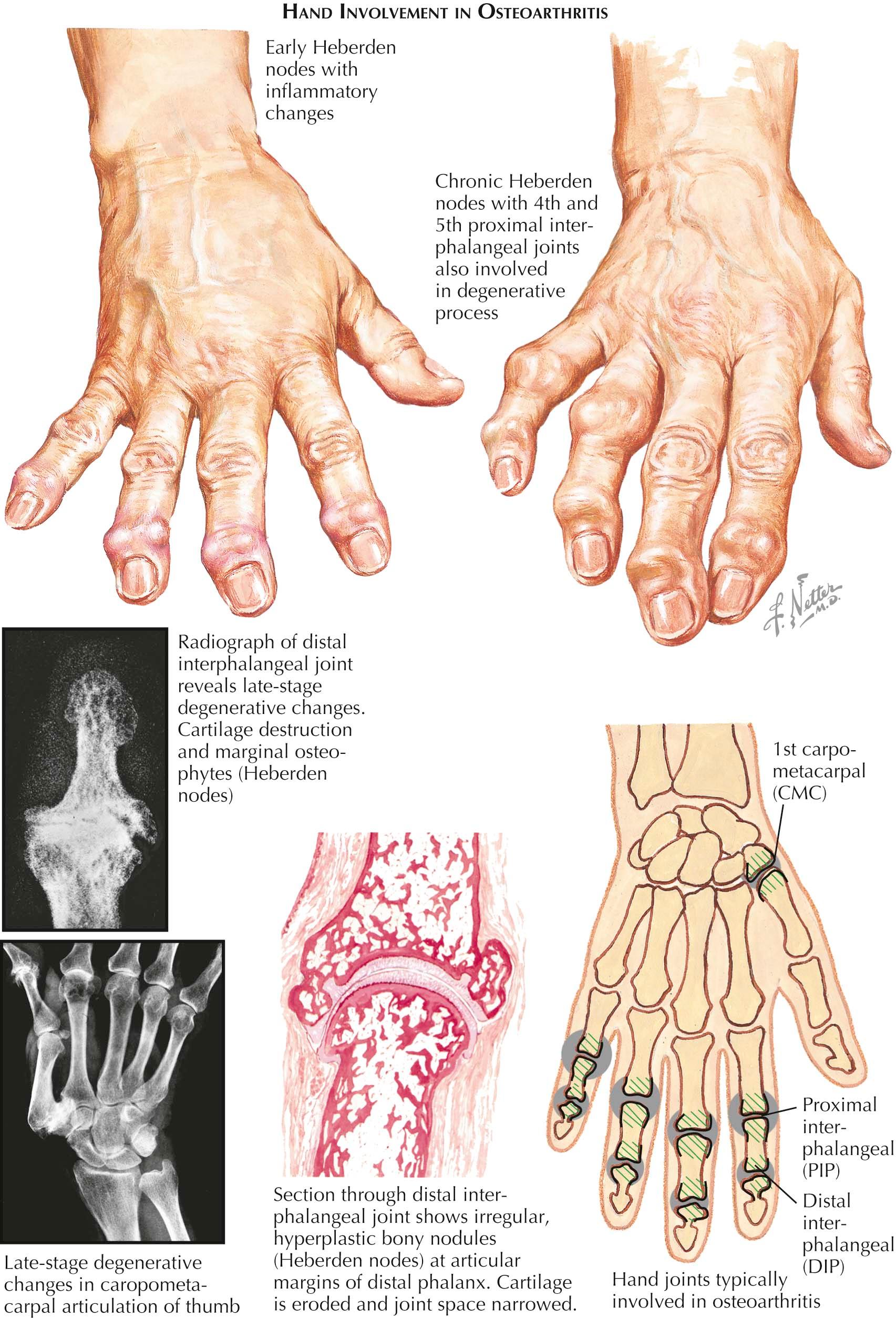
Rheumatoid arthritis and osteoarthritis (also called degenerative joint disease) are the most common forms of arthritis. Both of these chronic conditions are characterized by pain, stiffness, restricted joint motion, joint deformities, and disability, but their differences in pathogenesis, pathology, and clinical features must be distinguished because the prognosis and treatment of the two diseases differ. Other inflammatory arthritides that are of concern in the hand, especially gout, lupus, and psoriatic arthritis, are frequently seen.
Post-traumatic and postinfectious arthritis and treatment are typically specific to the joint affected by the insult, and the principles of treatment are often similar to those for the more common types of arthritis.
Some clinical manifestations are unique to particular joints. Heberden nodes, hallmarks of osteoarthritis, develop only at the terminal joints of the fingers. While the cartilage of the distal interphalangeal joint is degenerating, osteophytes grow from the dorsomedial and lateral aspects of the base of the distal phalanx to produce these nodular protuberances. Flexion or lateral deviation deformity usually results when the pathologic changes are severe. Early in their development, the nodes are tender and painful, especially when ganglion (mucoid) cysts coexist; when mature, they are asymptomatic and have only cosmetic significance. Heberden nodes are more common in women and are often familial. Bouchard nodes, similar to but less common than Heberden nodes, develop at the proximal interphalangeal finger joints.
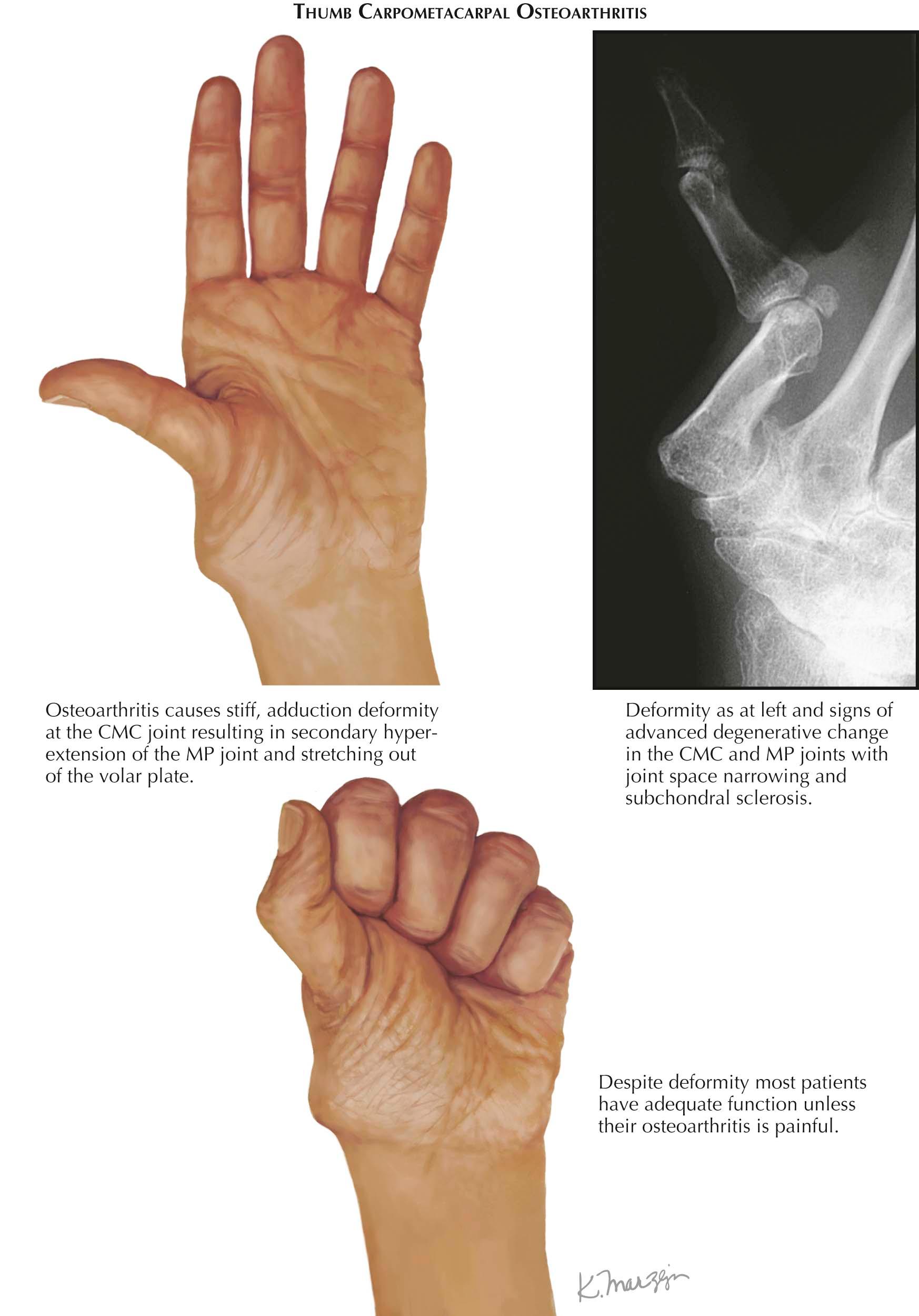
At the base of the thumb, the carpometacarpal articulation is the most common joint to undergo the degenerative changes of osteoarthritis. This joint is affected much more often in women. Local tenderness and pain, usually severe, are exacerbated by firm grasping and pinching, and progressive stiffness ensues.
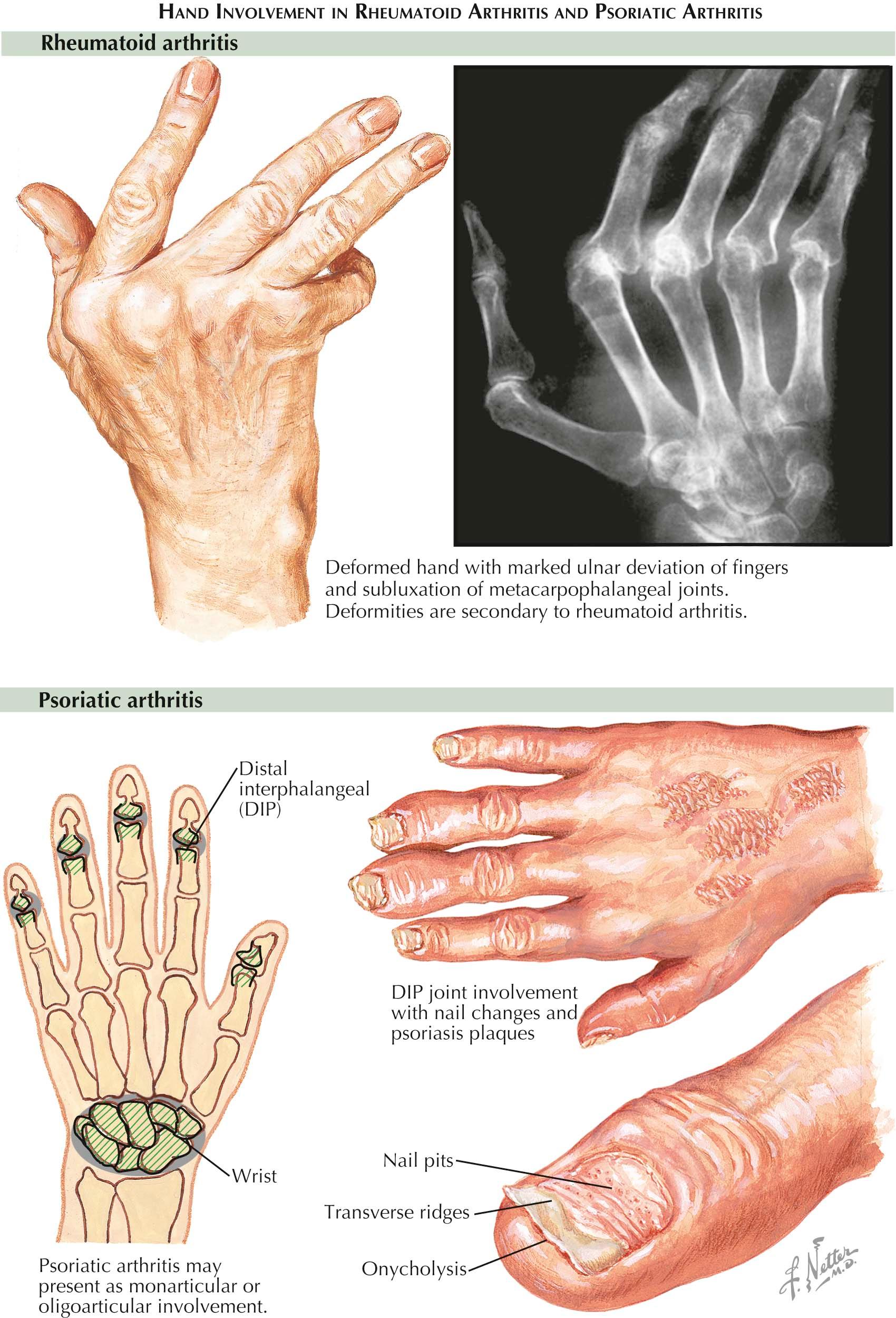
The joints of the hands and wrists are among the most frequent sites of involvement. In the fingers, some or all of the proximal interphalangeal joints are often bilaterally affected, whereas the distal interphalangeal joints are seldom involved. Because the inflammatory swelling occurs only at the middle joints, the affected fingers become fusiform in the early stages of disease. The metacarpophalangeal and wrist joints may also become inflamed. At first, there is little restriction of motion in the involved joints, but stiffness, swelling, and pain prevent the patient from making a tight fist, thus weakening grip strength. Except for soft tissue swelling, radiographs reveal no abnormalities.
As the disease progresses and the inflammation invades the joints, destroying articular cartilage and bone, joint motion becomes severely limited and joint deformities develop. Flexion deformities frequently occur at the proximal interphalangeal and metacarpophalangeal joints. The patient cannot fully extend or flex the fingers, and the grip becomes progressively weaker. Radiographs reveal cartilage thinning, bone erosions at the joint margins, and metaphyseal osteoporosis. After years of chronic inflammation, joint damage becomes severe; the joint capsule stretches; muscles atrophy and weaken; and tendons stretch, fray, and even rupture. All of these changes result in severe, incapacitating deformities.
A number of hand deformities are seen in the late stages of rheumatoid arthritis. For example, the muscles on the ulnar side of the fingers and wrist may overpower those of the radial group, causing ulnar deviation of the fingers at the metacarpophalangeal joints; the wrists may also be affected. The swan-neck deformity of the finger is common, as is the boutonniére deformity of the thumb, which is caused by hyperextension of the proximal interphalangeal joint and flexion at the metacarpophalangeal joint. The long extensor tendon may rupture near the distal interphalangeal joint, leaving the distal phalanx permanently flexed. Prolonged disease may lead to permanent subluxation or dislocation of the finger joints, and severe cartilage and bone erosion at the wrist may literally destroy the carpus. In this late stage of the disease, radiographs help to define the severity of the structural damage and deformities.
About 10% of persons with psoriasis have some form of inflammatory joint disease. Onset of the skin disease may long precede the arthropathy, but occasionally the reverse is true. The distinguishing features of psoriatic arthritis are (1) a predilection for the distal joints of the fingers and toes, frequently accompanied by psoriatic involvement of only a few other joints of the limbs; (2) destructive and mutilating changes of the phalanges adjacent to the inflamed joints, which produce the radiographic appearance of a “whittling” or “pencil point in cup” of the proximal phalanx and a “cupping” of the central portion of the base of the apposing distal phalanx, with bony proliferation of the borders; (3) shortening, angulation, and telescoping of the fingers due to extensive bone resorption in the phalanges; and (4) frequent involvement of the sacroiliac joints and spine, which simulates ankylosing spondylitis.
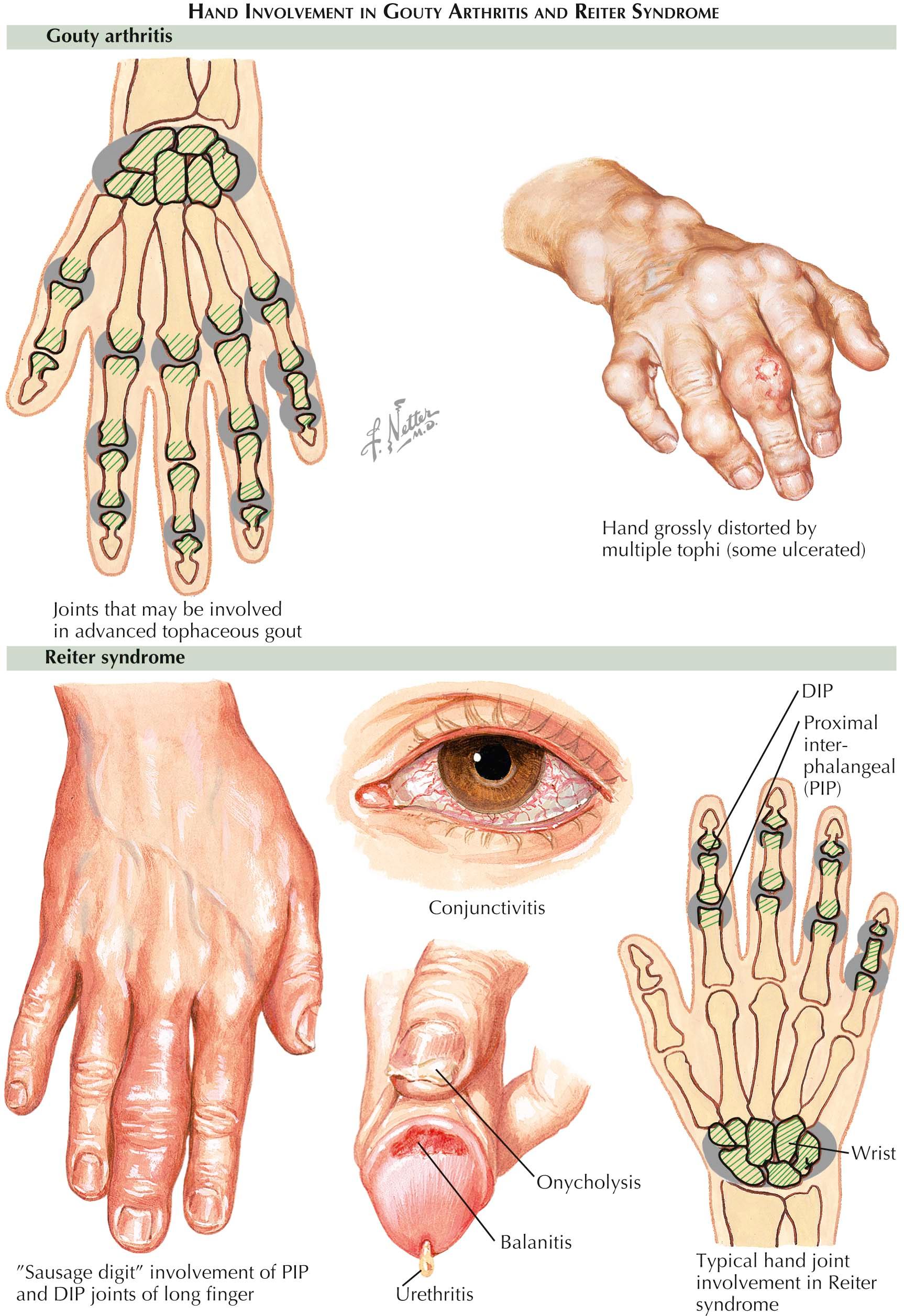
Almost always, the first clinical evidence of gout is acute arthritis in one or a few peripheral joints. A fulminant synovitis begins abruptly, typically during the night, frequently involving the first metatarsophalangeal joint. After several years of recurrent acute arthritis and persistent hyperuricemia, deposits of monosodium urate, called tophi, form in joint structures (and other tissues). Tophi are the hallmark of chronic gout, occurring in 50% of patients. They cause structural damage to articular cartilage and adjacent bone, resulting in chronic arthritis. In this late stage of the disease, known as chronic tophaceous gout, the affected joints show irregular knobby swelling and signs of chronic inflammation. Joint motion is limited and painful, deformities develop, and sinuses tend to form at the swollen joint, from which a calcific exudate drains from the underlying urate deposits.
Radiographs show marked destruction of bone and cartilage and “punched out” areas in the bone caused by the urate deposits.
Tophi often form in extra-articular structures as well, especially in the extensor tendons of the fingers and toes, the olecranon and infrapatellar bursae, the calcaneal tendon, the cartilage of the external ear, and the parenchyma of the kidney.
Reiter syndrome has been considered a clinical triad of urethritis, conjunctivitis, and arthritis. It is now accepted that a specific type of dermatitis is another characteristic of the disease, and diagnosis of complete Reiter syndrome requires the presence of at least three of these four signs: rarefaction of bone near the inflamed joints visible on radiographs (in chronic disease, articular cartilage destruction and joint deformities are also apparent); sacroiliac involvement (sometimes unilateral); vertebral syndesmophytes in skip distribution; and periosteal new bone formation at the insertion of the calcaneal tendon and calcaneal spurs.
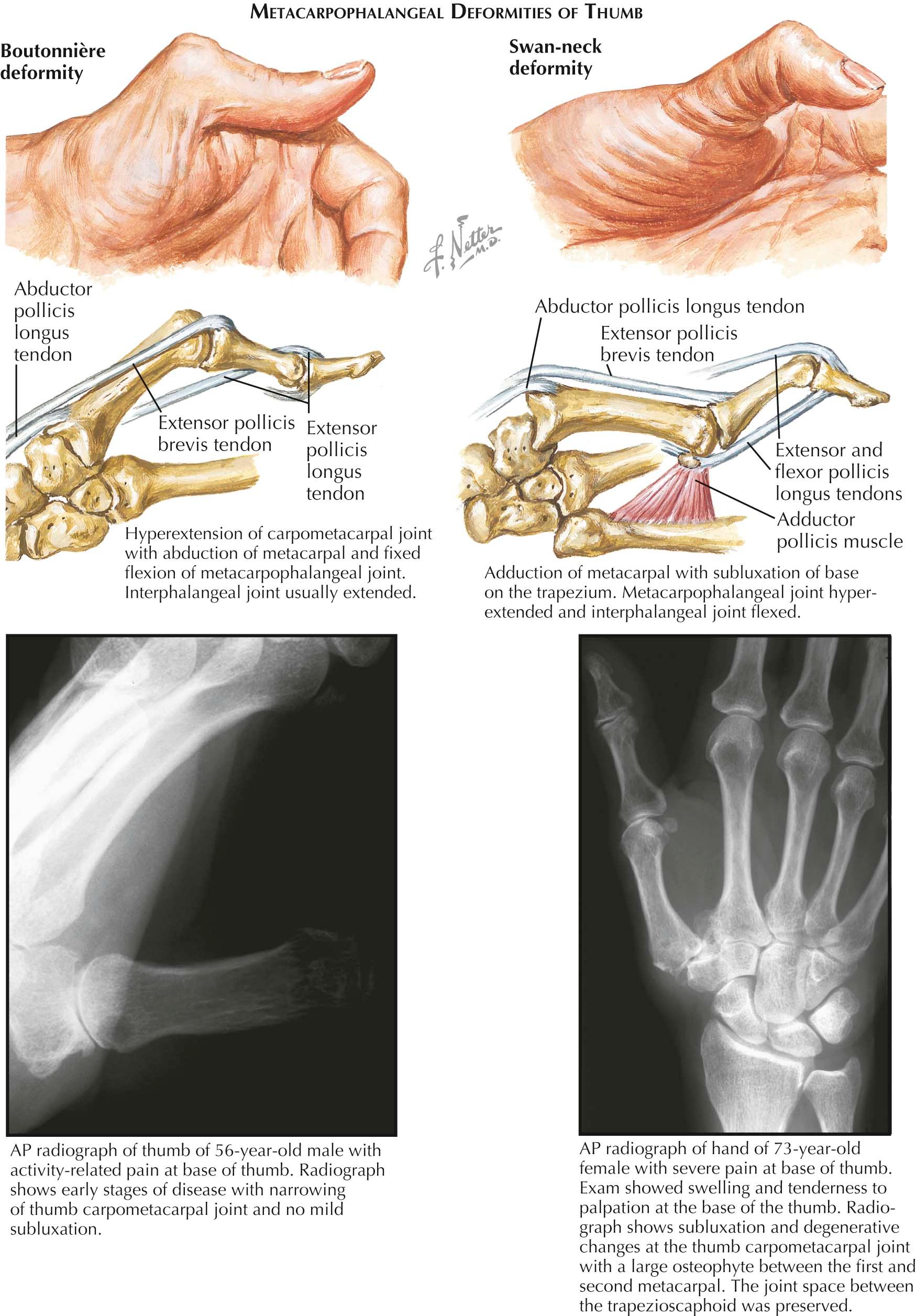
The thumb is the most important digit of the hand. All three joints of the thumb are important in functional adaptations, and each may be affected primarily or secondarily by imbalances of the other joints (e.g., boutonnière and swan-neck deformities). Thus, reconstructive surgery of the thumb must consider the entire thumb (radial) ray; the balance of its musculotendinous system; and the position, mobility, and stability of all its joints. The joints of the thumb may be impaired as a result of osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis. Thumb deformities can be classified as (1) postural, including longitudinal collapse (boutonnière, swan-neck) and fixed positional (adducted retroposed thumb) deformities; (2) unstable, stiff, or painful interphalangeal, metacarpophalangeal, or carpometacarpal joints; and (3) tendon deformities, including contracture, displacement, or rupture of the flexor pollicis longus, extensor pollicis longus or brevis, abductor pollicis longus, or intrinsic tendons.
The boutonnière deformity is caused primarily by arthritic involvement of the metacarpophalangeal joint. Although it is found in 57% of patients with hands affected by rheumatoid arthritis, boutonnière deformity does not usually occur in osteoarthritis. Initially, the capsule and extensor apparatus around the metacarpophalangeal joint are stretched by synovitis. The extensor pollicis longus tendon and adductor expansions are displaced ulnarly, and the lateral thenar expansions are displaced radially. The extensor pollicis brevis tendon attachment to the base of the proximal phalanx is lengthened, and the ability to extend the metacarpophalangeal joint is decreased, causing a flexion deformity of the proximal phalanx. The extensor pollicis longus tendon and extensor insertions of the intrinsic muscles apply all their power to the distal phalanx and produce secondary hyperextension of the interphalangeal joint. Pinch movements further aggravate the deformity. As contractures develop, the deformity becomes fixed. Destructive articular changes compound the deformity, and disorganization and subluxation of the joint may occur.
Swan-neck deformity, in contrast, is far more common in osteoarthritis than in rheumatoid arthritis. It is usually initiated by destructive changes at the carpometacarpal joint, followed by stretching of the joint capsule and radial subluxation of the base of the metacarpal. As motion at the trapeziometacarpal joint during abduction becomes painful, the patient avoids abduction, using the distal joints to compensate for lack of motion at the base of the thumb. An increasing adduction deformity with contracture of the adductor pollicis muscle develops. Effusion in the joint further loosens the capsule, permitting a proximal radial subluxation of the metacarpal. Subluxation may result in hyperextension of the interphalangeal joint, but more frequently, it causes hyperextension of the metacarpophalangeal joint and adduction of the first metacarpal. Further adduction contracture of the metacarpal aggravates the hyperextension of the metacarpophalangeal joint and permits collapse of the thumb ray. The interphalangeal joint becomes flexed, as in a swan-neck deformity of the finger.
In the adducted retroposed thumb, the first metacarpal is retropositioned, adducted, and externally rotated. The deformity is probably initiated by synovitis of the carpometacarpal joint and aggravated by awkward positioning of the thumb, as on a flat surface during acute illness. There seems to be a contracture of the extensor pollicis longus muscle, with adduction and external rotation of the metacarpal and with palmar and radial subluxation of the metacarpal base off the trapezium.
In rheumatoid arthritis, tendon deformities are related to muscle contracture, tendon displacement, adhesions, or tendon rupture. Rupture of the extensor pollicis longus tendon is most common, usually occurring within the third extensor compartment in the area of the distal tubercle of the radius. Sudden rupture of the tendon results in a sudden drop of the metacarpophalangeal joint of the thumb and, in some cases, loss of extensor power at the distal phalanx.
Rupture of the flexor pollicis longus tendon usually occurs in the carpal area and must be considered in the diagnosis of hyperextension deformity of the interphalangeal joint of the thumb. Rupture of the abductor pollicis longus and extensor pollicis brevis tendons is rare.
Synovial invasion and stretching of the dorsal hood of the metacarpophalangeal joint may result in displacement and secondary contractures of the tendons of the intrinsic muscles.
Arthrodesis is usually the preferred treatment for instability of the interphalangeal joint of the thumb; bone grafting is necessary if bone resorption is severe.
Arthrodesis is indicated in joint destruction and collapse deformities to simplify the articular system of the thumb ray, providing the distal and basal joints have adequate mobility. This can be achieved by a traditional tension band wire technique or more modern intramedullary locked-screw technology that provides a reproducible 25 degrees of flexion and more rapid return to function.
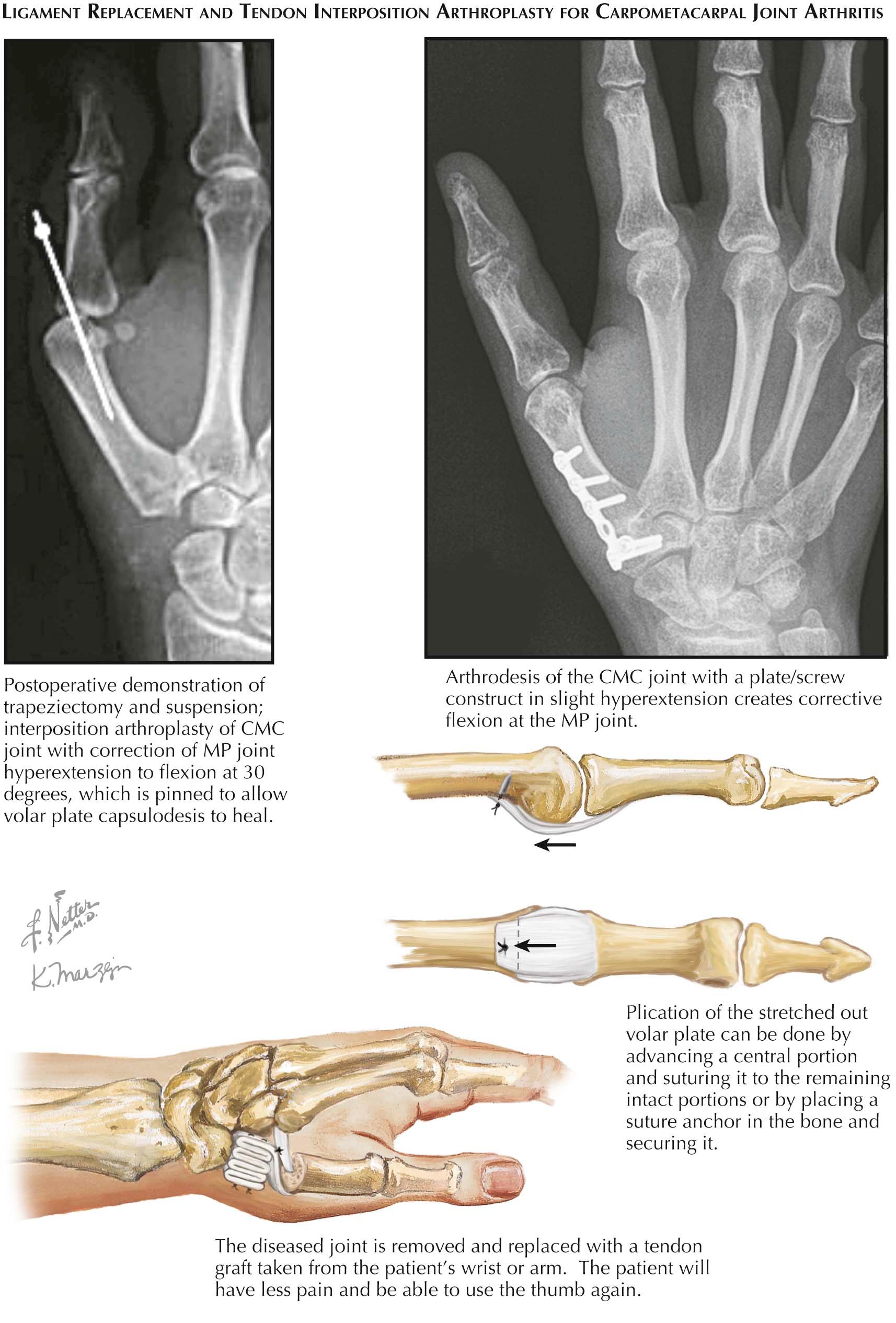
Capsulodesis is the treatment of choice in hyperextension deformities of more than 20 degrees with good flexion, lateral stability, and intact articular surfaces. The palmar aspect of the joint is exposed through a straight volar incision, and the central third of the proximal membranous insertion of the palmar plate is incised (alternatively all is incised if using a bone anchor). The sesamoids and their tendon attachments are left intact. The periosteum is stripped from the palmar aspect of the metacarpal neck and the joint is pinned at 30 degrees of flexion with a Kirschner wire, which is removed 6 weeks after surgery. The central third of the plate is sutured to the radial and ulnar thirds (or the whole plate is sewn to a bone anchor placed in the metacarpal neck).
The problems presented at the basal joints of the thumb differ in osteoarthritis and rheumatoid arthritis. Accurate diagnosis and evaluation of the location of the arthritic involvement and alignment of adjacent bones are essential in selecting the appropriate treatment. The pathologic changes may involve the trapeziometacarpal joint alone or also affect the peritrapezial or other carpal bone articulations, with or without resorption or displacement of adjacent carpal bones. Treatment must be selected from several options, including resection arthroplasty of the trapezium, with or without tendon interposition and with or without ligament reconstruction (the most typical procedure is ligament reconstruction and tendon interposition [LRTI]), arthrodesis of the carpometacarpal joint, or, less commonly, prosthetic arthroplasty. In some patients, the distal articulations of the thumb must be stabilized or fused.
Resection arthroplasty for the basal joints of the thumb helps maintain a smooth articulating joint space with improved joint mobility, pain relief, and strength. Meticulous reconstruction of the capsuloligamentous structures and correction of associated deformities of the thumb ray are essential for a good result.
In osteoarthritis, the destructive changes are usually present in all articulations around the trapezium and, in most patients, total trapeziectomy is necessary to relieve all arthritic pain. In rheumatoid arthritis, frequently the trapezium is fused to the scaphoid or the scaphoid is resorbed or shifted ulnarly. Therefore, a simple resection, with or without soft tissue interposition, can be used. In certain patients, severe resorptive changes of the metacarpal base and the trapezium produce a result not unlike a resection arthroplasty. If the joint is reasonably stable, mobile, and pain free, surgery is not indicated.
Resection arthroplasty for the trapezium is indicated for surgery when there is (1) localized pain and crepitation during passive circumduction, with axial compression of the thumb (grind test); (2) loss of motion, with decreased pinch and grip strength; (3) radiographic evidence of arthritic changes of the trapeziometacarpal, trapeziotrapezoid, trapezioscaphoid, and trapezium–second metacarpal joints; and (4) unstable, stiff, or painful distal joints of the thumb or a swan-neck deformity.
The trapezium is sectioned with an osteotome and removed piecemeal, with care not to injure the underlying flexor carpi radialis tendon. The radial artery must be carefully protected throughout the procedure. Then a tendon (typically the flexor carpi radialis longus either whole or half thickness) is passed through the base of the metacarpal and then sewn back onto itself snugly to re-create the volar beak ligament. The remaining tendon is sewn into a bundle and anchored to the floor trapezial space, thus creating an interposition arthroplasty. Thumb abduction is now restored and, if necessary, a volar capsulodesis of a hyperextended nonarthritic metacarpophalangeal joint is performed or arthrodesis in 25 degrees of flexion is done if painful arthritis is present.
After suture of the dorsal capsular flaps, the first dorsal compartment is loosely closed over the abductor pollicis longus and extensor pollicis brevis tendons. The extensor pollicis longus tendon is left subcutaneous. The incision is closed, with care to avoid the branches of the superficial radial nerve. A conforming hand dressing, including a thumb spica plaster splint, is applied. The limb is kept elevated, and a thumb spica short-arm cast or thermoplastic splint is applied after 4 to 6 days and worn for 4 to 6 weeks. Guarded motion and pinch and grasp activities using various exercise devices are then started.
Special considerations in reconstruction of the basal joints of the thumb include the following.
Hyperextension of the metacarpophalangeal joint of the thumb contributes to the adduction tendency of the metacarpal and prevents proper abduction of the metacarpal and seating of the implant. If hyperextension is less than 10 degrees, a cast is applied postoperatively so that the metacarpal, but not the proximal phalanx, is abducted. If the hyperextension ranges from 10 to 20 degrees, temporary fixation with a Kirschner wire is indicated; if it is greater than 20 degrees, stabilization with either palmar capsulodesis or arthrodesis is essential.
Adduction of the first metacarpal, if severe and untreated, unbalances the thumb and seriously affects the result of resection arthroplasty. If the angle of abduction between the first and second metacarpals is not at least 45 degrees, the origin of the adductor pollicis muscle must be released and likely the metacarpophalangeal joint arthrodesed.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here