Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The association and localization of aberrant vasculature in the facial skin, eyes, and meninges are compatible with a defect arising in a limited part of the cephalic neural crest, cells of which migrate to the supraocular dermis, choroid, and pia mater.
Performance. Seizures, paresis, intellectual disability.
Craniofacial. Port-wine capillary malformation, most commonly in a trigeminal facial distri–bution, sometimes involving the choroid of the eye with secondary buphthalmos or glaucoma as well as the conjunctiva or episcleral region; involvement usually unilateral, sometimes bilateral; overgrowth of bony maxilla secondary to the vascular anomaly.
Imaging. Capillary malformation involving arachnoid and pia mater, especially in occipital and temporal areas produces secondary cerebral cortical atrophy, sclerosis, and “double contour” convolutional calcification.
Capillary malformation in nonfacial areas; microgyria; macrocephaly; hydrocephalus; intracranial hemorrhage; colobomata of iris; retinal vasculature tortuosity; iris heterochromia; retinal detachment; strabismus; coarctation of aorta; enlargement of the ear when involved with capillary malformation; ENT infections; obstructive sleep apnea; macrodactyly; central hypothyroidism; growth hormone deficiency.
The surface capillary malformations are usually present at birth and seldom progress. Seizures most commonly begin between 2 and 7 months of age, are grand mal in type, and frequently are induced by fever. The degree of central nervous system (CNS) involvement is variable, with 30% having paresis and approximately 83% having seizures; 39% have normal intelligence. A poor prognosis for cognitive development is predicted by the number of seizures, an early age of onset, a poor response to treatment, bilateral cerebral involvement, or severe unilateral lesions. An increased risk has been reported for emotional and behavioral problems, including mood disorder, attention-deficit hyperactivity disorder, disruptive behavior disorder, and adjustment disorder.
Aggressive control of seizures is recommended. Although anticonvulsants are the most common treatment, surgery is often considered for refractory seizures. In a recent study of 32 affected children who had hemispherectomy, 81% were seizure-free. Stroke-like episodes are common, particularly in toddlers and young children, often following falls with seemingly minor head injuries. Low-dose aspirin has been proposed to improve long-term cognitive function and overall quality of life.
Glaucoma presents before 2 years of age if tissues destined to form the anterior chamber angle are affected. If only conjunctival and episcleral vascular tissues are involved, glaucoma frequently does not occur until after 5 years of age. Heterochromia iridis with darker iris on the glaucomatous side appears to be a marker for cases that will develop glaucoma.
Cerebral calcification is usually not evident by radiography until later infancy. Vascular magnetic resonance imaging (MRI) or computed tomography (CT) scan often does not detect lesions before 1 year of age. Although pulsed dye laser therapy is the treatment of choice, complete clearance of the port-wine stain rarely occurs.
A recurrent somatic activating mutation in GNAQ (c.548G>A, p.ARG183Gln) has been identified in affected tissue from 88% of evaluated individuals. Mutations have also been found in affected tissue from individuals with nonsyndromic port-wine stains, suggesting that the extent of the phenotype is determined by the developmental time point at which the mutation occurs.
Port-wine facial nevi occur frequently without eye or brain abnormalities. Only patients with lesions involving the ophthalmic distribution of the trigeminal nerve (dermatome V1, including the upper eyelid) are at risk for neuroocular complications. In rare cases, the leptomeninges are involved without the face or choroid. With respect to screening, if the child is developing normally, has a normal neurologic examination, no history of seizures, and a normal MRI, that child probably does not have Sturge-Weber sequence brain involvement.

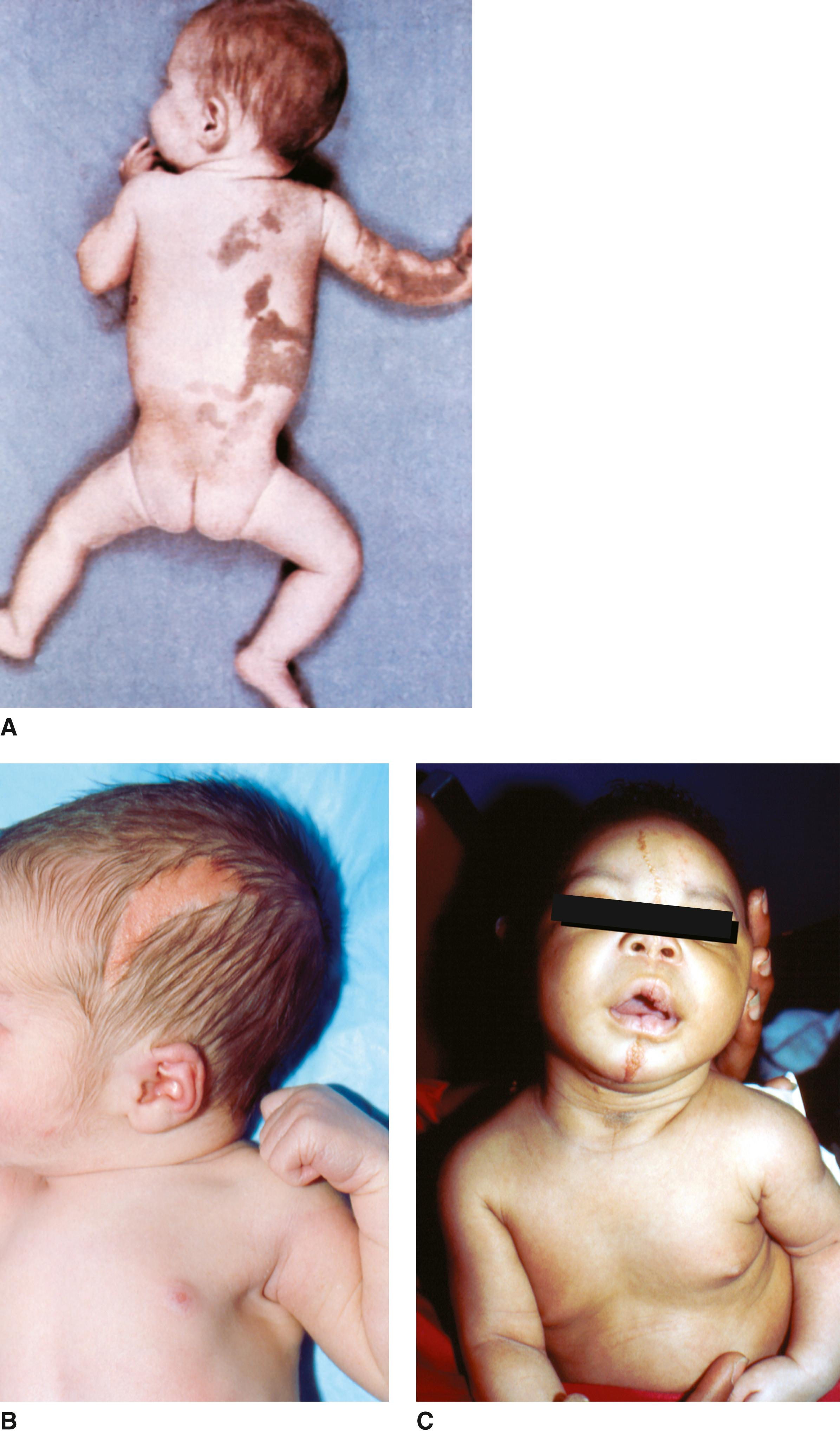
This melanocytic hamartomatosis of the skin and pia-arachnoid was first described in 1861. More than 100 cases have been reported.
Performance. Liable to development of seizures and deterioration of CNS function; cranial nerve palsies, particularly VI and VII.
Skin. Giant pigmented nevi (66%) usually in a “bathing trunk” or lumbosacral distribution, less frequently in the occipital region or upper back; numerous congenital nevi (at least three) without a prominent large lesion (34%); associated small or medium-sized congenital melanocytic nevi on the scalp, face, or neck occur in association with the larger lesions.
Visceral. Thick and pigmented with nests and sheets of melanotic cells, 88% with cranial involvement and 88% with spinal involvement.
Imaging. Hydrocephalus secondary to blockage of cisternal pathways or obliteration of arachnoid villi by the tumor; involvement of spinal cord and its coverings.
Syringomyelia; Dandy-Walker malformation; psychosis; Meckel diverticulum; urinary tract anomalies, including renal pelvis and ureteral malformations, unilateral renal cysts, rhabdomyosarcoma; leptomeningeal melanoma; extracranial melanoma, probably representing metastases from meningeal melanoma; liposarcoma; malignant peripheral nerve sheath tumor.
The cutaneous melanosis is grossly evident at birth. CNS function may be normal initially, but seizures and other signs of increased intracranial pressure often develop before the age of 2 years. Mental deterioration may begin before 1 year of age, apparently related to the melanoblastic involvement of the pia-arachnoid and spinal cord compression. Leptomeningeal melanoma occurs in 40% to 62% of patients with CNS infiltration, and intracranial melanomas are found frequently.
The CNS consequences of the disorder often result in early demise. Three of the initially described patients were stillborn; the majority died before 2 years of age, and only 10% of the patients are known to have survived past the age of 25 years. The interval between the age at initial presentation and death ranges from immediate to 21 years, with more than one-half occurring within 3 years of initial diagnosis.
In 23% to 30% of patients with neurologically asymptomatic, large congenital melanocytic nevi, focal magnetic resonance signals are present in the leptomeninges or adjacent brain parenchyma. The most common locations for melanosis are the amygdala, followed by the brainstem, cerebellum, cerebral cortex, and thalamus. Although the prognosis for these patients is unknown, the majority followed for 5 years have not developed symptomatic neurocutaneous melanosis. MRI scans of the brain are recommended in all infants with congenital nevi with a diameter more than 2 cm in the cranial area or over the spine as well as in infants with more than 20 satellite nevi so that involvement of the brain is detected early. Imaging should be repeated at regular intervals to detect progress of intracerebral melanosis or development of hydrocephalus. Patients with satellite nevi are of greatest risk for development of neurocutaneous melanosis. Patients without nevi on the head or neck or the posterior midline rarely develop neurologic complications.
The risk of malignant melanoma degeneration of the cutaneous melanosis is reported as 5% to 15%, with half becoming evident by 5 years of age. Thus, surgery to reduce the skin lesions is indicated in patients in whom careful evaluation has documented a lack of leptomeningeal involvement.
Somatic mutations in codon 61 of NRAS have been documented in most studies of patients to date. Moreover, loss of heterozygosity of this gene has been demonstrated in two cases that progressed to melanoma. The sex incidence of this disorder is equal.

Nevus sebaceous of Jadassohn is most commonly found in an otherwise normal individual. However, the association of this type of lesion in the midfacial area with seizures and intellectual disability has been reported in at least 100 cases.
Growth. Asymmetric overgrowth, advanced bone age.
Performance. Seizures of major motor, focal, or minor motor types; intellectual disability.
Skin. Nevus sebaceous with hyperpigmentation and hyperkeratosis; lesions most commonly in the midfacial area, from the forehead down into the nasal area, tending to be linear in distribution; may also affect trunk and limbs.
Skeletal. Cranial asymmetry or hemimacrocephaly; premature closure of sphenoid frontal sutures, sphenoid bone malformation, and abnormalities of sella turcica; scoliosis, kyphosis, abnormalities of ulna, radius head, humerus, and fibula; polydactyly, syndactyly; vitamin D–resistant rickets.
Eyes. Esotropia, lipodermoid of conjunctiva, cloudy cornea, cataract, colobomata of eyelid, coloboma of iris and choroid, atrophy of optic nerve, subretinal neovascularization, microphthalmia.
Central Nervous System. Micro- and/or macrocephaly, cerebral and cerebellar hypoplasia, arachnoid cysts, hydrocephalus, hemiparesis, cranial nerve palsy, cortical blindness, hypertonia, cerebral vascular changes, intracerebral calcifications, cerebral neoplasia/hamartoma.
Other. Short palpebral fissures, pigmented nevi; spotty alopecia; coarctation of aorta, patent ductus arteriosus, hypoplastic left heart, ventricular septal defect; cardiac arrhythmias; hypoplasia of aortic branches, renal or pulmonary artery; cleft palate; hypoplastic teeth; renal hamartomata, nephroblastoma, double urinary collecting system, horseshoe kidneys; rhabdomyosarcoma; enlarged clitoris; undescended testes; cystic biliary adenoma of liver; lymphatic malformations; dental anomalies; hemihypertrophy.
The nevus sebaceous is usually present at birth as a slightly yellow to orange to tan waxy-appearing lesion containing deficiencies or papillomatous excesses of epidermal elements, especially sebaceous glands and immature hair follicles. Pubertal expansion of the lesion commonly involves rapid growth with hormonally driven development of sebaceous glands and maturation of apocrine glands. The lesions tend to become verrucous and unsightly. Tumors can occur in infancy, but are more frequent in adult life. Although the risk was initially reported to be 15% to 20%, recent studies suggest 2% to 3% risk for tumor and less than 1% risk for malignancies. Trichoblastomas and other benign tumors may account for 90% of the associated tumors. In rare cases basal cell carcinomas (the most common malignant lesion), sebaceous carcinomas, squamous cell carcinomas, and keratoacanthomas occur. Early surgical removal should be considered. In the cases with associated CNS features, the onset of seizures has been from 2 months to 2 years, and they are difficult to control. The intellectual disability has been moderate to severe, although an occasional patient may have normal intelligence. The vitamin D–resistant rickets that sometimes occurs is a variant of tumor-induced osteomalacia. The associated ricketic lesions, muscle weakness, and bone pain, as well as the biochemical abnormalities, reverse following surgical removal of the skin lesions.
The linear sebaceous nevus sequence and isolated epidermal nevi are caused by somatic activating mutations in HRAS or KRAS . A very specific HRAS mutation, c.37G>C (p.Gly13Arg), has been detected in most cases. A mutation in the adjacent paralogous residue of KRAS (p.Gly12Asp or p.Gly12Val) accounts for some cases. The HRAS c.37G>C mutation causes constitutive activation of the MAPK and PI3K-Akt signaling pathways. Other mutations in these genes are rarely identified. Mutations were not found in fibroblasts underlying the nevus sebaceous, but were found in the keratinocytes from the lesions, confirming that the mutation is solely in the ectodermally derived cells.
Two unique conditions have recently been described in a few patients with nevus sebaceous : (1) aplasia cutis congenita and nevus sebaceous and (2) SCALP (nevus s ebaceous, C NS malformation, a plasia cutis congenita, l imbal dermoid, p igmented nevus) syndrome. Although the cooccurrence of two pur–portedly disparate skin lesions gave rise in the literature to the twin spot hypothesis implicating two homozygous recessive mutations as causal, the recent finding of heterozygous HRAS and KRAS mutations in phacomatosis pigmentokeratotica (another such disorder) has disproven this theory.
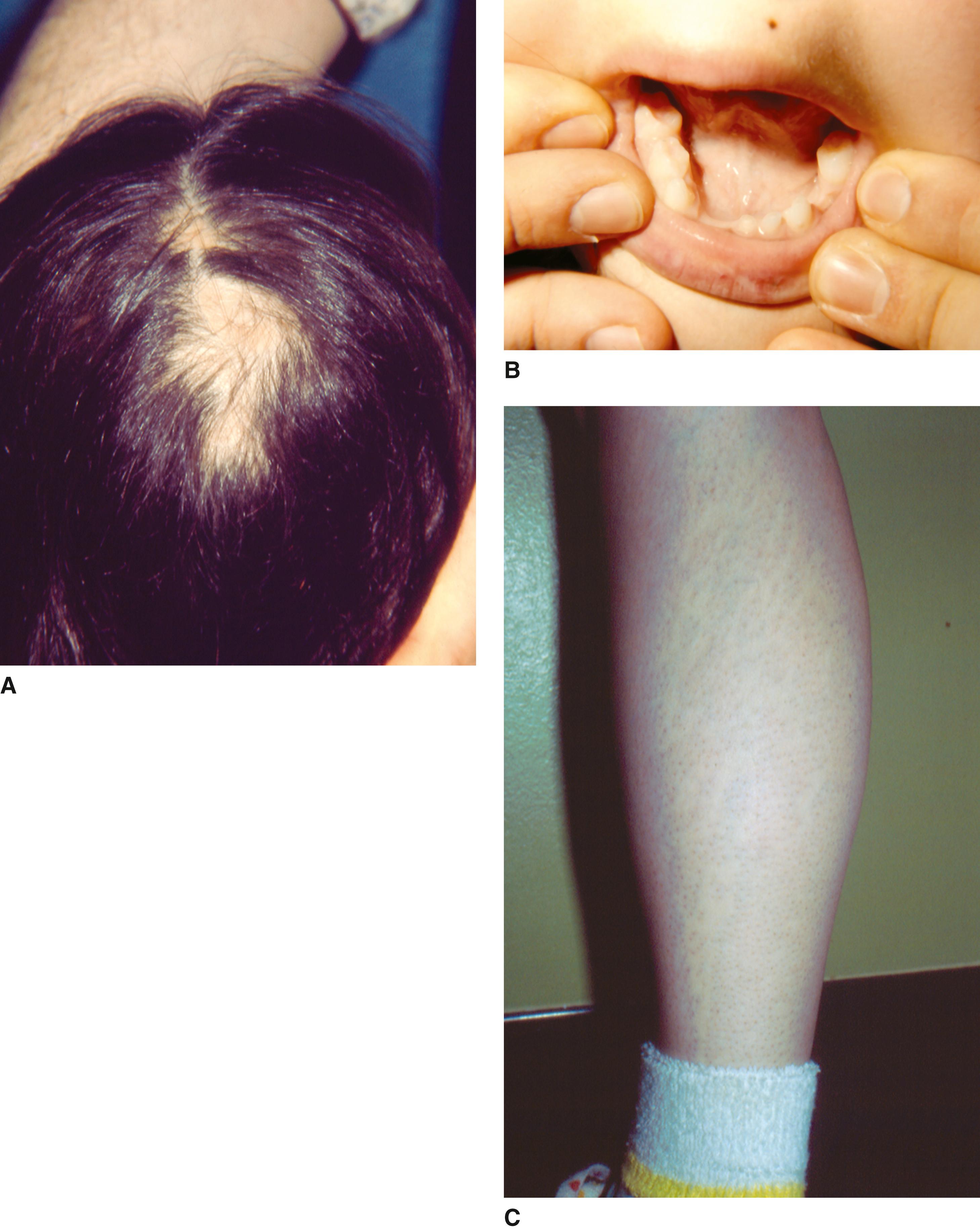
Bardach originally described the condition in twin sisters in 1925, and soon thereafter Bloch set forth the term incontinentia pigmenti to depict the unusual skin lesions. The preponderance of cases occurs in females.
Performance. Seizures (20%), motor impairment, infantile encephalopathy, acute disseminated encephalomyelitis, and ischemic stroke. One-third have significant intellectual disability.
Craniofacial. Approximately 30% have strabismus, often with refractive errors; abnormalities of the retinal vessels and underlying pigment cells in 40%, leading to retinal ischemia, new vessel proliferation, bleeding, and fibrosis; retinal detachment, uveitis, keratitis, cataract, microphthalmos, and optic atrophy occur infrequently; hypodontia (> 50%), delayed eruption, or conical form.
Skin. Blisters, preceded by erythema, develop typically in a linear distribution along the limbs and around the trunk within the first 4 months (bullous stage); as the blisters begin to heal, hyperkeratotic lesions develop on the distal limbs and scalp and rarely on the trunk or face for several months (verrucous stage); hyperpigmentation, most apparent on the trunk distributed along lines of Blaschko, occur in streaks and whorls, usually developing after the blisters have disappeared (hyperpigmentation stage); pale, hairless patches or streaks most evident on the lower legs develop usually at the time the hyperpigmentation disappears (atretic stage).
Hair and Nails. Atrophic patchy alopecia, especially on the posterior scalp at the vertex; lusterless, wiry, coarse hair as well as thin, sparse hair in early childhood; mild ridging or pitting to severe nail dystrophy with onset from 3 to 45 years of age, usually after puberty.
Skeletal. Approximately 20% have hemivertebrae, kyphoscoliosis, extra rib, syndactyly, hemiatrophy, or short arms and legs.
Microcephaly, high arched palate, cleft of the lip and palate (1.5%), breast hypoplasia, supernumerary nipple, nipple hypoplasia, dacryostenosis, eczema, short stature, hydrocephalus, subungual keratotic tumors.
Bullous skin lesions are generally present in early infancy and tend to progress from inflammatory or vesicular to pigmented and may fade in childhood. General eosinophilia is often present in infancy and the vesicles contain eosinophils. Verrucous lichenoid lesions develop during infancy in approximately one-third of cases, especially over the dorsum of the hands and feet. During the period when the blisters are present, the lesions should be kept dry and protected from trauma. The development of the irregular marble cake-like pigmentation may or may not coincide with the sites of bullous or verrucous lesions. The pigmented areas gradually fade in the second to third decades, and the adult may show only slightly atrophic depigmented “achromic stains,” especially over the lower legs. Because the retinal vascular changes sometimes progress during the neonatal period, monthly ophthalmologic evaluations are recommended during the first 2 to 3 months of life. In approximately 10% of cases, this process progresses to severe scarring with significant visual loss. The greatest risk for retinal detachment is in infancy and childhood; it almost never occurs after age 6 years. Approximately one-half of the patients show other features, the most serious being the CNS abnormalities. Seizures in the neonatal period are reported in 20%, seem to correlate with the degree of cerebrovascular damage, and thus represent an ominous sign relative to future neurologic development. In their absence, prognosis, in most cases, is good. No patients have developed new neurologic symptoms during adolescence or at adult age. In a recent study of 14 girls from 1 to 12 years of age, 5 had severe to mild intellectual disability; the remaining had normal IQ scores. Two of 4 school-age girls in that study showed normal intelligence, but had specific disabilities in calculation and math reasoning.
This disorder has an X-linked dominant inheritance pattern with male lethality in the vast majority of cases. IKBKG , previously the nuclear factor-kappa B (NF-κB) essential modulator ( NEMO ) gene located at Xq28, is the only gene known to be associated with incontinentia pigmenti (IP). A deletion that removes exons 4 through 10 of IKBKG mediated through recombination of direct tandem repeats is present in about 80% of affected individuals. The product of this gene protects against apoptosis. In females with IP the functionally aberrant cell clone is eliminated by apoptosis, resulting in eradication of defective cells and healing of skin lesions soon after birth as well as detectable skewing of X-inactivation that occurs in 98% of females with IP. Cases of males with IP have been reported. Survival in a male is mediated through one of three mechanisms: a less deleterious mutation, mainly in exon 10; a 47XXY karyotype; or somatic mosaicism. A female with IP may have inherited the IKBKG mutation from her mother or have a de novo mutation (65%). In familial cases parents may either be clinically affected or unaffected, but have germline mosaicism. Molecular testing of the mother is warranted because of the widely variable expressivity of the phenotype in adult women. Affected women have a 50% chance of transmitting the mutant IKBKG allele at conception; however, male conceptuses with a loss-of-function mutation of IKBKG do not survive.
Three other conditions are caused by mutations in IKBKG : X-linked hypohidrotic ectodermal dysplasia and immunodeficiency (HED-ID), HED-ID with osteopetrosis and lymphedema, and X-linked atypical mycobacteriosis, all affecting males exclusively, caused by missense mutations that result in impaired but not absent signaling.

Initially described by Ito in 1952, numerous affected individuals subsequently have been reported. The characteristic skin lesions involve streaked, whorled, or mottled areas of hypopigmentation on limbs or trunk, usually evident in infancy. It is now clear that hypomelanosis of Ito is not a specific disorder, but rather an etiologically heterogeneous physical finding that is frequently indicative of chromosomal or genetic mosaicism, also named pigmentary mosaicism of the Ito type. Approximately 70% of reported cases have associated anomalies. With the exception of intellectual disability, seizures, and cerebral atrophy, all other associated abnormalities have occurred in a small number of patients.
Performance. Variable intellectual disability in 30% to 50%; autistic behavior; seizures, including generalized tonic-clonic seizures, partial seizures, myoclonic seizures, and infantile spasms.
Craniofacial . Macrocephaly, coarse facies, hypertelorism, epicanthal folds, thick lips, cleft lip/palate, malformed auricles, iridial heterochromia, coloboma of iris, abnormal retinal pigmentation (most often hypopigmented), strabismus, nystagmus, myopia, dacryostenosis, corneal asymmetry, pannus, cataract and pinpoint pupils, microphthalmia, small optic nerve, optic atrophy.
Other. Central precocious puberty; café au lait spots; cutis marmorata; angiomatous nevi; nevus of Ota; mongolian blue spots; abnormal sweating; ichthyosis; morphea; hypertrichosis; diffuse alopecia; variations in hair color and texture; ridging, dystrophy, or occasional absence of nails; dysplasia of teeth, abnormal number and shape, enamel defects, irregularly spaced teeth; clinodactyly, syndactyly, ectrodactyly, polydactyly, triphalangeal thumb, genu valga; asymmetry of length or size of limbs and body parts, joint contractures, particularly talipes; kyphoscoliosis/lordosis, pectus excavatum, and carinatum; short stature.
The skin lesions, which are best appreciated by a Wood’s lamp examination, do not go through a prodrome phase as in incontinentia pigmenti. The skin lesions are often not detected in the newborn period, but become apparent within the first months of life (80%). In some cases they may remain unrecognized until some other symptoms appear or until the child is first exposed to the sun. Seizures commonly appear early, within the first years of life. Autistic behavior, severe intellectual disability, and drug-resistant epilepsy may occur. Of patients, 7% have hemihypertrophy. Of those there is an increased risk for abdominal tumors, most frequently Wilms tumor
Hypomelanosis of Ito is etiologically heterogeneous. Karyotyping of characteristic skin findings to rule out chromosomal mosaicism when developmental delay or structural anomalies are also present is indicated. Although only a small number of cases of smaller chromosomal rearrangements detected by chromosomal arrays have been reported in association with hypomelanosis of Ito, it is likely that new cases will be identified. Recurrence risk is low, except in those chromosomally abnormal individuals in whom a balanced parental translocation is present. A single-gene basis for hypomelanosis of Ito probably does not exist.

Von Recklinghausen is said to have described this disease, but Bourneville is usually given credit for its recognition in 1880. Hamartomatous lesions develop in many tissues, especially the skin and brain. Diagnostic criteria, as well as guidelines regarding assessment, surveillance, and treatment of tuberous sclerosis syndrome, were published in 2013 by the International Tuberous Sclerosis Complex Consensus Group. The incidence of tuberous sclerosis complex (TSC) has been estimated to be 1 in 5800 live births.
Performance. Seizures (80%), intellectual disability (50%), autism spectrum disorder (40%).
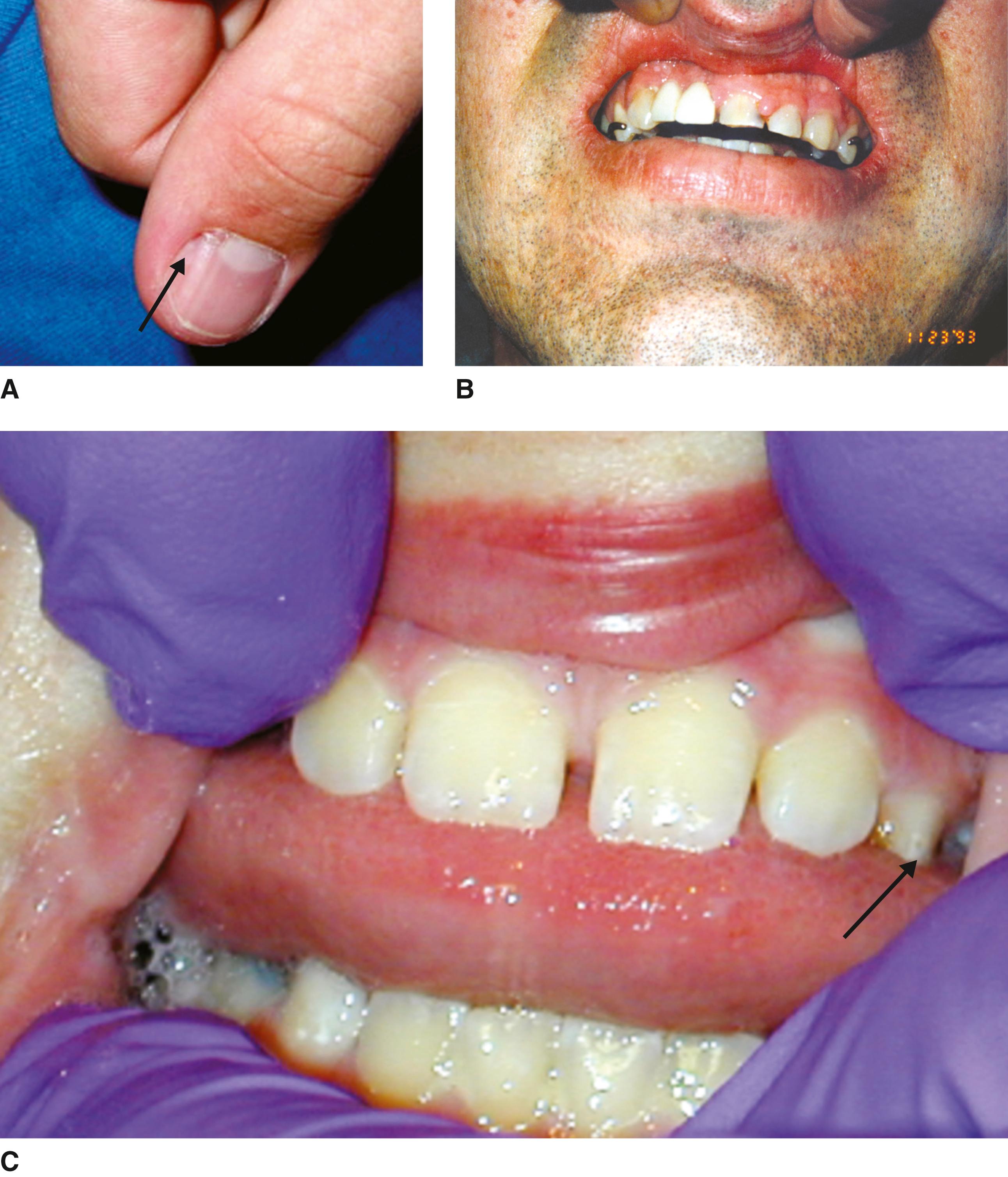
Craniofacial. Multiple retinal nodular hamartomas, most often bilateral; retinal achromic patches; multiple randomly distributed pits in dental enamel, most evident by close inspection of labial premolar surfaces; gingival fibroma.
Skin. Facial angiofibromas (varying in color from flesh to pink to yellow to brown in the nasolabial fold, cheeks, and elsewhere), nontraumatic ungual or periungual fibromas, shagreen patch (connective tissue nevus with a goose flesh-like appearance), hypomelanotic macules (three or more may be “thumb-print” macules, “lance-ovate” macules [one end rounded, the other with a sharp tip] or ash leaf macule); minor confetti macules (tiny 1- to 3-mm macules). Some type of hypomelanotic macules can be found in virtually all patients. The other skin lesions occur in approximately half the cases.
Imaging. Subependymal nodules, cortical tubers (both in > 70% of cases), subependymal giant cell astrocytoma; cerebral white matter radial migration lines; bone cysts occurring mainly in phalanges (66%) with areas of periosteal thickening yielding radiologic evidence of “sclerosis.”
Visceral. Multiple renal angiomyolipomas (> 50%), usually benign; renal epithelial cysts, including tubular enlargement and cyst formation with hyperplasia of tubular cells; pulmonary lymphangiomyomatosis (40% of women of childbearing age); arrhythmias; single or multiple cardiac rhabdomyomas.
Other. Hamartomatous rectal polyps, nonrenal hamartoma (liver and pancreas and other).
Other hamartomas, lipomas, angiomas, nevi, angiomas of heart, hepatic angiomyolipomas, hypothyroidism; thyroid adenomas; sexual precocity; lymphedema; hypertension; neuroendocrine tumors, including pituitary adenomas, parathyroid adenomas and hyperplasia, and pancreatic adenomas (insulinoma and islet cell neoplasm); oncocytoma (benign adenomatous hamartoma); malignant angiomyolipoma; renal cell carcinoma.
Hamartomatous lesions usually become evident in early childhood and may increase at adolescence. However, prenatally, cardiac rhabdomyomas are present in 30% to 50% of fetuses with TSC. When rhabdomyomas are identified on fetal ultrasound examination the risk of TSC is 50% to 80%, and much greater if the lesions are multiple. Postnatally these tumors usually involute. Facial nodular lesions are present in 50% of children by 5 years, whereas white macules are present at birth or in early infancy in almost all patients, and are visualized easily with a Wood’s lamp. Brain tumors develop in approximately 10% of patients. These giant cell astrocytomas may enlarge, causing pressure and obstruction and resulting in significant morbidity and mortality. However, malignant transformation of the periventricular nodules is rare. The seizures, which tend to develop in early childhood, may initially be myoclonic and later grand mal in type and are difficult to control. Electroencephalographic abnormality is found in 87% of patients and may be of the grossly disorganized hypsarrhythmic pattern. The seizures, the severity of intellectual disability, and autistic behavior seem to be related to the extent of hamartomatous change in the brain. Mental deterioration is unusual, except in relation to frequent seizures of status epilepticus. None of the skin lesions results in serious medical problems, but facial angiofibromas can be a cosmetic problem. Eye lesions are usually asymptomatic, but retinal astrocytic hamartomas can cause retinal detachment and neovascular glaucoma. At least 80% of children will have some renal finding by age 10 years.
Renal angiomyolipomas can cause pain from hemorrhage into the tumor. Those larger than 3.5 to 4.0 cm should be considered for prophylactic renal arterial embolization or renal sparing surgery.
An unknown percentage of patients die before 20 years of age as the consequence of status epi lepticus, general debility, pneumonia, or tumor. However, there is marked variability. Seizures and/or mental deficiency do not develop in all patients with skin lesions, and the above noted pattern of abnormality is biased toward the more severe cases. It is not infrequent to diagnose an asymptomatic parent of a severely affected child. Females tend to have milder disease than males.
This disorder has an autosomal dominant inheritance pattern. Approximately two-thirds of cases represent fresh mutations. Mutations in TSC1, located at 9q34, and of TSC2, located at 16p13, encoding proteins referred to as hamartin and tuberin, respectively, are responsible. Both are tumor suppressor genes. Molecular genetic testing of TSC1 and TSC2 will identify a mutation in approximately 85% of individuals. The frequency of somatic mosaicism for large deletions and duplications of TSC1 and TSC2 in patients with normal sequencing analysis may be as high as 5%. Thus, careful parental evaluation is strongly recommended before genetic counseling. TSC1 mutations have milder disease manifested by fewer seizures and less severe intellectual disability and autism, fewer subependymal nodules and cortical tubers, less severe kidney involvement, no retinal hamartomas, and less severe facial angiofibromas. Individuals with large deletions of TSC2 , which also include PKD1, are at risk of developing the complications of autosomal dominant polycystic kidney disease,
Haploinsufficiency of TSC1 and TSC2 dysregulates mechanistic target of rapamycin (mTOR) activity which, in association with other proteins in the mTOR signaling pathway, result in aberrant brain development and many of the manifestations of this disorder. The use of mTOR inhibitors is providing an encouraging treatment option for some of the features of tuberous sclerosis syndrome, particularly for subependymal giant cell astrocytomas and renal angiomyolipomas.

Von Recklinghausen described this disease in 1882. Diagnostic criteria were set forth at the National Institutes of Health in 1988. It is estimated to affect 1 in 3000 individuals.
Growth. Mild short stature; macrocephaly of postnatal onset.
Performance. Mean IQ of 88. Seizures, speech and learning disorders.
Skin. Café au lait macules over 5 mm in greatest diameter before puberty and over 15 mm following onset of puberty. Inguinal or axillary freckling (90% by 7 years). Ninety-nine percent have six or more macules greater than 5 mm in diameter by 1 year of age.
Tumors. Neurofibromas (a heterogeneous benign peripheral neural sheath tumor) occurring as discrete dermal masses, focal cutaneous or subcutaneous growths, dumbbell-shaped intraforaminal spinal tumors, or diffuse plexiform neurofibromas.
Other. Lisch nodules or pigmented iris hamartomata (70% by 10 years), unidentified bright objects of high signal density on T2-weighted MRI of the brain (60%).
Tumors, including optic pathway gliomas (1.5% to 7.5%, with median age of development 4.9 years) and other astrocytomas, neurilemomas, meningiomas, malignant pheochromocytomas, duodenal carcinoids, rhabdomyosarcomas, and neurofibromas. Seizures or electroencephalographic abnormalities in approximately 20%; intellectual disability in 2% to 5%, with learning disability, hyperactivity, or speech problems in 50%; cerebral vascular compromise; headaches; hydrocephalus; enlarged corpus callosum; scoliosis, occasionally early, severe, and progressive; pectus excavatum; hypoplastic bowing of lower legs, with pseudoarthrosis at birth; osseous lesions with localized osteosclerosis, rib fusion, spina bifida, absence of patella, dislocation of radius and ulna, local overgrowth, and scalloping of vertebral bodies with deformed pedicles; sphenoid wing dysplasia; osteopenia and osteoporosis; cutaneous nevi, lipomata, angiomata, neurofibroma in kidney, stomach, heart, tongue, and bladder; syndactyly; glaucoma, ptosis, corneal opacity, potentially malignant melanoma of iris; malignant peripheral nerve sheath tumors; precocious puberty; verrucous nevus; pruritus; pulmonic stenosis; vascular hyperplasia of the intima and media leading to Moyamoya progressive cerebral vascular disease, peripheral vascular disease, midaortic syndrome, stenosis, and aneurysms of aortic branches and coronary arteries; essential hypertension, pulmonary hypertension, interstitial lung disease, and lung cancer.
At least two of the following criteria are sufficient for a firm clinical diagnosis of neurofibromatosis type 1 (NF1): (1) six or more café au lait macules over 5 mm in greatest diameter in prepubertal individuals and over 15 mm in greatest diameter in postpubertal individuals; (2) two or more neurofibromas of any type or one plexiform neurofibroma; (3) freckling in the axillary or inguinal regions; (4) optic glioma; (5) two or more Lisch nodules (iris hamartomas); (6) a distinctive osseous lesion, such as sphenoid dysplasia or tibial pseudarthrosis; or (7) first-degree relative (parent, sibling, or offspring) with NF1.
The majority of cases in affected individuals have a benign course. Nearly all patients have enough features to allow diagnosis by 6 years of age. Neurofibromas rarely develop in children younger than 6 years of age, but are present in 48% of 10-year-olds and 84% of 20-year-olds. They may increase in size and number at puberty, during pregnancy, and between 50 and 70 years of age. The complications of neurofibromatosis can be divided into those that are structural (macrocephaly, segmental hypertrophy, scoliosis, pseudoarthrosis, cardiac defects, vascular stenosis, and aneurisms), those that relate to neoplasia, and those that are functional (problems with executive function, visuospatial processing, attention deficit, hyperactivity, and autism spectrum disorder are common, and there exists an increased risk for developing other psychiatric conditions such as anxiety and depression). Screening for structural and functional complications can be done effectively through comprehensive physical evaluation every 6 months. Routine screening for CNS tumors is not warranted in the majority of cases. Rather, clinicians following affected individuals should maintain a high index of suspicion and evaluate specific signs and symptoms as they develop. Normal growth charts for affected children have been established. All newly diagnosed patients should have an ophthalmologic examination and then be followed yearly through 6 years of age to rule out an optic pathway glioma; thereafter, their occurrence is rare. Of children with an optic pathway glioma involving the optic chiasm, 39% develop precocious puberty. Most optic gliomas are stable and do not need specific treatment. Malignant peripheral nerve sheath tumors, which arise almost exclusively in preexisting plexiform neurofibromas, develop in approximately 10% of patients with NF1. There is a five-fold increased risk for breast cancer and a high risk for myeloid leukemia. The rapidly progressive (dysplastic) form of scoliosis almost always develops between ages 6 and 10 years. Survival is shortened, with a mean age of 61.1 years at death.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here