Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Sarcoidosis (Gr. sarkos , flesh; eidos , form), so named because its histologic features were originally thought to resemble a sarcoma (Boeck), is a common systemic disease of unknown etiology. It is characterized and defined by the presence of noncaseating granulomata, usually (but not invariably) affecting multiple organ systems. Manifestations are variable. Patients may present with:
an acute and usually self-limiting variant,
a chronic form exclusively affecting the skin (up to between 20% and 40% of patients with cutaneous sarcoidosis do not have systemic involvement),
a serious systemic chronic variant with widespread lesions, which affects multiple systems, is associated with high morbidity, and may occasionally be fatal.
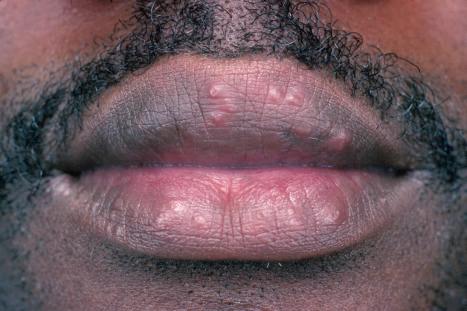
Sarcoidosis is more commonly encountered in industrialized countries and shows particularly high incidences in northern Europe (including the UK), the USA, and New Zealand, where as many as 20/100 000 of the population may be affected. It presents particularly in people in their third and fourth decades and shows a female predominance. In the USA, sarcoidosis is common among blacks, and there is a similar tendency in the UK ( Figs 9.1 and 9.2 ). An epidemiological study of sarcoidosis in the Detroit, Michigan, area found that African-Americans living there had a 3.8 times greater risk of developing the disease compared with Caucasians. The disease is rare in Asians. First- and second-degree relatives of patients with sarcoidosis seem to have a significant risk of developing the disease compared to the normal population. The disease is rare in children, presents mainly in teenagers, and although the manifestations are usually similar to those seen in adults, infants may present with symptoms simulating juvenile rheumatoid arthritis ( Fig. 9.3 ). Two forms of sarcoidosis have been identified in children. A variant affecting older children and occurring mainly during teenage years presents with a multisystemic disease similar to that seen in adults. Younger children under the age of 4 present with a cutaneous rash, arthritis, and uveitis. Infantile sarcoidosis should not be confused with Blau syndrome. This disease is inherited in an autosomal dominant fashion and is characterized by sarcoidal granulomata in the skin, uveal tract, and joints but with no pulmonary involvement. Despite the similarities between both diseases, no genetic linkage has been identified.


Rarely, sarcoidosis presents in monozygotic twins. Coexistence with common variable immune deficiency is also a rare occurrence.
Cutaneous lesions occur in 20–35% of patients with systemic sarcoidosis and may be classified into non-specific (erythema nodosum) and specific (granulomatous) subtypes. Cutaneous sarcoidal granulomata appear to be associated with a poorer prognosis and an increased incidence of pulmonary fibrosis and uveitis. Chronic facial lesions have been shown to be more commonly associated with involvement of the lungs, sinuses, and eyes. Erythema nodosum occurs quite commonly in sarcoidosis, with reported incidences varying from 11% to 31%. There is a significant female predominance (3 : 1). Interestingly, erythema nodosum appears to be relatively uncommon in both African-Americans and Caucasians in the USA. It presents as erythematous, tender, subcutaneous nodules, usually on the anterior tibial regions. Erythema nodosum may be associated with pyrexia, polyarthralgia (wrists, knees, and ankles), a very high erythrocyte sedimentation rate (ESR), and bilateral hilar lymphadenopathy (Lofgren syndrome). This acute form of sarcoidosis is associated with a good prognosis, with most patients experiencing resolution within 6 months of onset of symptoms. In one study, however, 16% of patients who presented with erythema nodosum developed chronic disease.
A not uncommon mode of presentation is the development of a widespread, usually asymptomatic, maculopapular eruption. Individual lesions are erythematous or violaceous, 3–6 mm in diameter, and most commonly seen on the face (particularly in a periorbital distribution), the trunk, the extensor aspects of the extremities, and the neck ( Figs 9.4 and 9.5 ). In this variant, the patient may also develop acute lymphadenopathy and uveitis, and a chest X-ray examination can reveal features of early respiratory involvement. Spontaneous resolution sometimes occurs. Occasionally, micropapular lesions are seen, particularly on the face and limbs ( Fig. 9.6 ). Rarely, patients develop sheets of pinhead-sized lichenoid papules on the trunk and limbs. The onset is abrupt, and lesions may appear in crops. Some patients develop nodules and plaques, which may occur anywhere on the body, but most often affect the face, extremities, buttocks, and shoulders ( Figs 9.7–9.11 ). Annular or serpiginous lesions are also encountered, and sometimes there is a prominent telangiectatic component (angiolupoid sarcoid) ( Figs 9.12 and 9.13 ). Rarely, epidermal changes result in a psoriasiform or even ichthyosiform appearance. An exceptional case mimicking lipodermatosclerosis has been described. Chronic skin lesions are associated with pulmonary fibrosis, ocular, and bone involvement.










Most characteristic of sarcoidosis, however, is lupus pernio. This chronic violaceous plaque most often affects the nose, cheek, and ears, but lesions also sometimes affect the fingers and knees ( Fig. 9.14 ). It is a particularly disfiguring variant, and resolution is especially complicated by marked scarring. Lupus pernio is often associated with lesions in the upper respiratory tract and can be followed by nasal obstruction and septal perforation. Patients also have severe pulmonary fibrosis, bone cysts, and ocular lesions. This variant has an insidious onset and is associated with a prolonged course and poor prognosis.

Patients with sarcoidosis not uncommonly develop lesions in scar tissue and also in relation to trauma at the sites of desensitizing injections, tattoos, venipuncture, surgery, laser, cosmetic fillers, and BCG ( Fig. 9.15 ). A single case attributed to copper-containing earrings has been described. Sarcoidal granulomata in association with foreign bodies do not necessarily imply a diagnosis of sarcoidosis. However, a small number of patients with sarcoidal granulomata in association with silica and tattoo pigment may have systemic sarcoidosis or the latter may develop subsequently. Awareness of this problem is important as such cutaneous granulomata may be the first manifestation of the disease. Sarcoidosis has also been documented presenting in a tattoo in association with interferon-alpha (IFN-α) treatment for chronic hepatitis C. Interestingly, sarcoidosis has also been reported rarely in patients receiving interferon and ribavirin for chronic hepatitis C, and in rare patients on interferon-alpha or interferon-B therapy for melanoma. Sarcoidosis in patients with chronic hepatitis C may present concomitantly with the disease and unrelated to medication, or more often triggered by treatment, mainly ribavirin and interferon-alpha.

Sarcoidosis has rarely been described in patients on Vemurafenib for metastatic melanoma. An association has also been occasionally reported in patients on infliximab, etanercept, adalimumab, ipilimumab, and natalizumab. Sarcoidal granulomas occurred in a patient on nivolumab for desmoplastic melanoma. The association of the disease with antitumor necrosis factor agents is paradoxical as these agents are used to treat the disease.
Hypopigmented lesions may be seen in black patients. Unusual cutaneous manifestations include subcutaneous nodules, ichthyosiform lesions, erythroderma, scarring and nonscarring alopecia, lymphedema, nail dystrophy in the absence of underlying bone changes, verrucous lesions, generalized atrophy, leonine facies, palmar erythema, and leg ulcers with or without granulomatous vasculitis. Lesions of scarring alopecia may clinically mimic discoid lupus erythematosus. Subcutaneous nodules are rare and present as persistent, freely mobile, often painful lesions measuring 5–15 mm in diameter. It has been suggested that subcutaneous lesions are more often associated with systemic disease. In further studies however, subcutaneous involvement does not seem to be associated with increased incidence of systemic disease or worse prognosis. Oral and genital involvement is rare, but disease restricted to the vulva has been documented. Sarcoidosis has also been described presenting as a testicular mass. A very rare variant of seasonal photoinduced cutaneous sarcoidosis may occur.
Ninety percent of patients with sarcoidosis have pulmonary involvement. Bilateral hilar lymphadenopathy is the most common intrathoracic manifestation of sarcoidosis and, together with pulmonary involvement, forms the most frequent lesion. Intrathoracic manifestations in sarcoidosis are classified into five subgroups:
Stage 0: normal chest X-ray,
Stage I: bilateral hilar and/or paratracheal lymphadenopathy with no pulmonary involvement,
Stage II: lymphadenopathy with pulmonary infiltrates,
Stage III: pulmonary infiltrates, but no lymphadenopathy,
Stage IV: irreversible fibrosis and bullae, cysts, emphysema.
Stage I disease is frequently associated with spontaneous resolution; progression to stage II disease is uncommon. Severe pulmonary involvement as seen in stage III patients correlates with deep chronic plaque lesions and lupus pernio. Patients have interstitial fibrosis and eventual cor pulmonale, which may prove fatal.
Systemic vasculitis involving small- to large-caliber vessels has been found in some adults and children with sarcoidosis. This manifestation tends to be more common in African-American and Asian patients.
Ocular lesions develop in about 20% of patients with sarcoidosis. Acute anterior uveitis is the most common manifestation; it is frequently bilateral and shows a predilection for females. It correlates with a benign outcome and erythema nodosum. Chronic uveitis also affects the anterior chamber and if untreated may progress to glaucoma and blindness. Other lesions include retinal vein perivasculitis, disc edema, and neovascularization. Conjunctival granulomata may be present in up to 30% of patients; therefore, biopsy can be a useful and relatively safe method of establishing the diagnosis. The lacrimal gland is also sometimes affected.
Neurological involvement occurs in 5–15% of patients with systemic sarcoidosis. Clinical manifestations include small fiber neuropathy, facial nerve palsy, Guillain-Barré syndrome, optic nerve disease, meningitis, seizure, and encephalopathy. In one study, neurosarcoidosis was the presenting symptom in 31% of patients. The combination of uveitis, facial nerve palsy, fever, and swelling of the parotid gland is known as uveoparotid fever (Heerfordt syndrome). This condition is often associated with central nervous system involvement. Hypothalamic and pituitary lesions are rare and may manifest as diabetes insipidus or panhypopituitarism.
Peripheral lymphadenopathy develops in about 30% of patients. However, histologic examination of peripheral lymph nodes will reveal granulomata in about 75% of patients with sarcoidosis. Although splenomegaly is only present in 10–25% of patients, granulomata are present in about 50% of cases. Splenic disease is usually asymptomatic, but patients may have abdominal pain, hypersplenism, and, very rarely, splenic rupture. Splenic disease correlates positively with a high frequency of intrathoracic sarcoidosis. Liver function test abnormalities are quite common, and about 20% of patients have hepatomegaly; 60% of patients have hepatic granulomata on histologic examination.
Cardiac lesions are uncommon, but are of particular importance due to the associated mortality. In an autopsy series, 50% of all deaths were due to cardiac disease. This same study found that the clinician often does not appreciate the presence of cardiac involvement – the antemortem diagnosis of cardiac lesions was made in only 29% of patients. Granulomata may occur at any site, but appear to show a predilection for the conduction system. Clinical manifestations include ventricular tachycardia, complete heart block, congestive cardiac failure, pericardial effusion, and myocardial infarction. Sarcoidal granulomata may affect small and large blood vessels, in particular the pulmonary vasculature.
Muscle involvement is usually asymptomatic. Histologic examination of random muscle biopsies reveals granulomata in as many as 50% of patients. Rare features include asymptomatic palpable nodules and a polymyositis-like syndrome.
Although a rare complication, patients with sarcoidosis appear to be more prone to develop cryptococcosis than other infections.
Radiologically demonstrable bone lesions occur in about 15% of patients. Early lesions consist of osteoporosis, cortical thinning, and mottled rarefaction. Established lesions are cystic and are sometimes associated with pathological fractures. The hands and feet are predominantly affected ( Fig. 9.16 ). Destruction of the nasal bones can result from direct infiltration in patients with lupus pernio.

Hypercalcemia and, particularly, hypercalcuria are important complications of sarcoidosis. This is possibly due to increased intestinal absorption of calcium and abnormal production of 1,25-dihydroxyvitamin D. It is more often transitory, but in a small proportion of patients it is persistent and sometimes complicated by the development of renal failure due to nephrocalcinosis. Granulomata are found on histologic examination of the kidney in up to 40% of patients.
Laboratory investigations reveal a wide variety of abnormalities of the immune system (see below). Patients may demonstrate elevated levels of serum angiotensin-converting enzyme (ACE). Unfortunately, this finding is not specific for sarcoidosis, increased values also being found in patients with diabetes mellitus, alcoholic liver disease, and leprosy. It is sometimes of value in monitoring the level of disease activity in patients known to have sarcoidosis. Patients may also display increased levels of serum and urinary lysozyme, serum beta-2-microglobulin, and collagenase.
Although sarcoidosis is associated with a high morbidity, the mortality rate is low, being of the order of 3–6%. Causes of death include cardiac involvement and respiratory or renal failure. The prognosis is better in females and appears to be improved in those with a positive purified protein derivative (PPD) skin test and normal serum immunoglobulin levels. The severity of disease is greater in blacks and Asians compared with Caucasians. Of interest, despite the very marked upset in immunological phenomena, patients do not seem to have an associated greatly increased risk of opportunistic infections except as a consequence of therapy (e.g., corticosteroids).
The association between sarcoidosis and a number of systemic diseases is probably coincidental. Sarcoidosis has been documented in association with vitiligo, pernicious anemia, autoimmune thyroiditis, Graves disease, chronic hepatitis, Addison disease, Sjögren syndrome, diabetes mellitus and ulcerative colitis, lymphoma, human immunodeficiency virus (HIV) infection, and primary biliary chirrosis. Interestingly, patients with acquired immunodeficiency syndrome (AIDS) usually develop manifestations of sarcoidosis after antiretroviral therapy is started. This phenomenon is the result of the immune restoration syndrome. Associations with cutaneous autoimmune disease include dermatitis herpetiformis and linear IgA disease. A single case of trachyonychia associated with sarcoidosis has been reported.
The pathogenesis of sarcoidosis is poorly understood. The demonstration of familial clustering suggests hereditary susceptibility to sarcoidosis in at least a subset of patients.
Despite intensive studies, the etiology and pathogenesis of sarcoidosis remains elusive. It is likely, however, that sarcoidosis represents a reaction pattern that may develop in a predisposed patient on exposure to one or more infective agents or other antigens.
The role of mycobacteria in the pathogenesis of sarcoidosis is a controversial topic. Attempts at detection of mycobacterial DNA by polymerase chain reaction (PCR) have produced conflicting results. While some authors have failed to detect mycobacterial DNA, others have identified DNA of various strains of tuberculous and nontuberculous mycobacteria. In one study, although amplified mycobacterial DNA was detected by PCR in 38% of sarcoidosis patients, mycobacterial DNA was also detected in tissue in 44% of control patients. Furthermore, most studies published in the literature fail to report more than 6% positivity for Mycobacterium tuberculosis DNA in patients with sarcoidosis. In another interesting study, cell wall deficient acid-fast bacteria (L forms) were cultured from the blood of 19 of 20 patients with sarcoidosis but not from controls. In summary, these mixed results between laboratories have not clarified the role of mycobacteria in the pathogenesis of sarcoidosis. It seems, however, that mycobacteria may be of etiological importance in at least a subset of cases.
Propionibacterium acnes DNA has also been identified in tissues of patients with sarcoidosis, including involved lymph nodes. The significance of this finding remains uncertain. Human herpesvirus 8 DNA has not been demonstrated in tissues of patients with sarcoidosis.
The occasional association with known autoimmune diseases, such as progressive systemic sclerosis and systemic lupus erythematosus (SLE), has inevitably led to the proposal of an autoimmune pathogenesis. Although many familial cases have been reported in the literature, no consistent pattern of inheritance has emerged. The results of human leukocyte antigen (HLA) typing have shown associations with particular features of the disease; for example, HLA-A1 and HLA-B8 are associated with arthritis, HLA-A1 is also associated with uveitis, and HLA-B13 may be associated with a chronic refractory variant. Patients with HLA-DR17 have a better prognosis. One study has shown that patients with sarcoidosis have an increased frequency of a glutamine residue at position 69 of the B1 chain of the HLA-DPB molecule compared with a control population. This is particularly interesting since a similar polymorphism has been documented in patients with chronic beryllium disease, a disorder also characterized by granulomata and which shares some pathological features in common with sarcoidosis.
Immunological investigations in patients with sarcoidosis have produced an immense wealth of data, which reveal that there is clearly an associated state of abnormal immunological hyperactivity. There are alterations of both cell-mediated and humoral immunity. Despite great efforts to clarify the immunobiology of sarcoidosis, particularly with regard to the precise antigens that may facilitate the disease, we still do not have a clear understanding of the disease process. Sarcoidosis, at least in part, appears to be due to a hyperactive T-helper cell proliferation with lymphokine production. Increased T-helper (Th1, Th2) cells are present in the alveolar lung parenchyma. Several studies have demonstrated selective activation of certain oligoclonal T-cell subsets. In one study, there was a correlation between the particular oligoclonal T-cell subsets and disease activity. Th1 lymphocytes (T cells expressing interleukin [IL]-2 and IFN-γ) preferentially accumulate in pulmonary parenchyma and the alveolar space compared with Th2 lymphocytes (T cells expressing IL-4 and IL-5). Compared with T cells in peripheral blood, T cells obtained by bronchoalveolar lavage show greater expression of IFN-γ and tumor necrosis factor-alpha (TNF-α). Of interest, patients with HLA-DR17 show a muted cytokine response, a finding that is perhaps related to the better prognosis observed in this subset of patients.
T lymphocytes, in turn, stimulate B cells. Abnormalities of humoral immunity include a non-specific polyclonal hypergammaglobulinemia and circulating immune complexes in acute forms of the disease, particularly in association with erythema nodosum.
The paramount puzzle in unraveling the pathogenesis of sarcoidosis is identifying the initial event(s) that lead to the disease. Despite our increasing knowledge of the immunobiology of sarcoidosis, we seem no closer to answering this key question. It seems clear, however, that the disease is the result of a complex interaction between many different external antigens, genetic predisposition, and the immune responses.
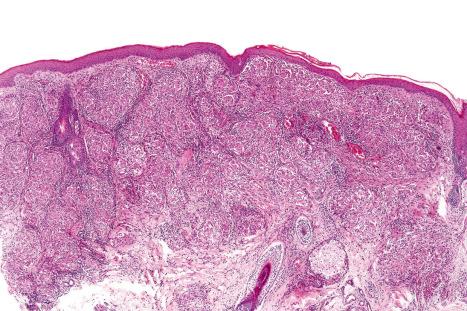
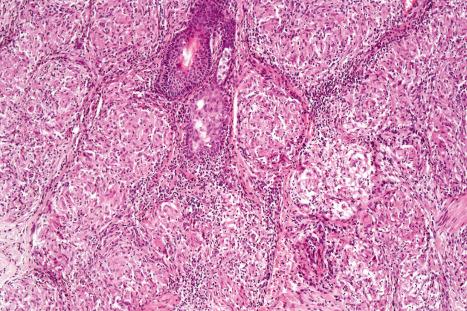
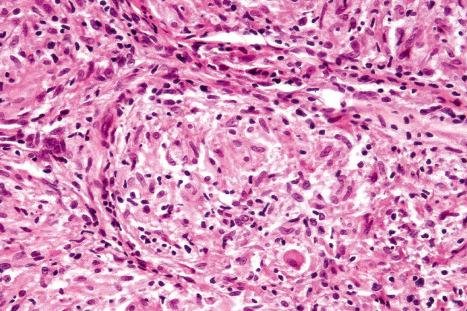
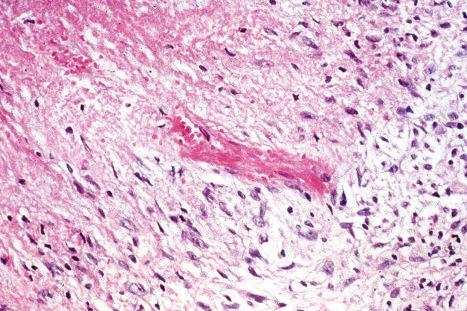
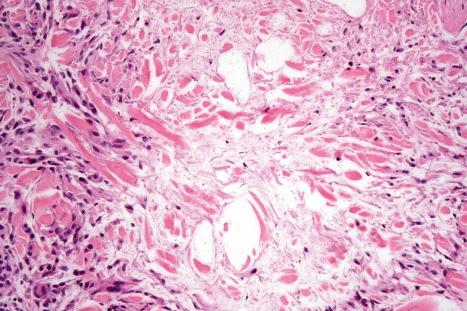
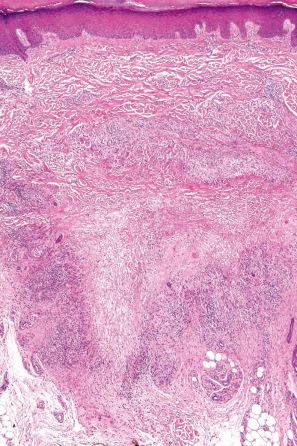
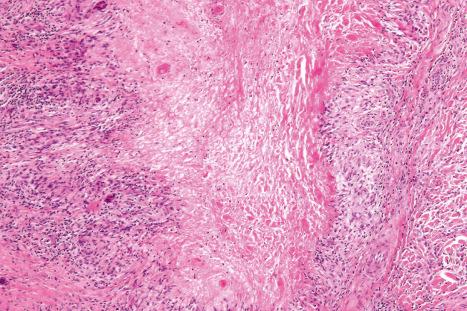
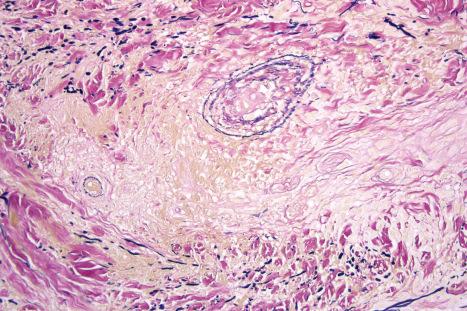
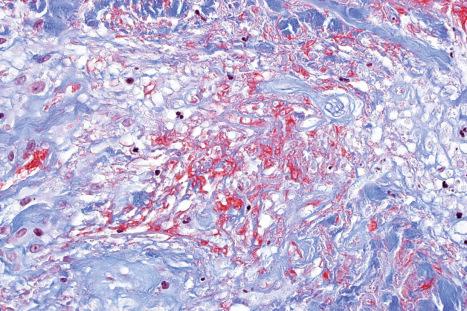
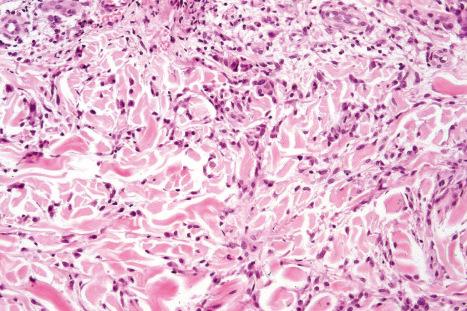
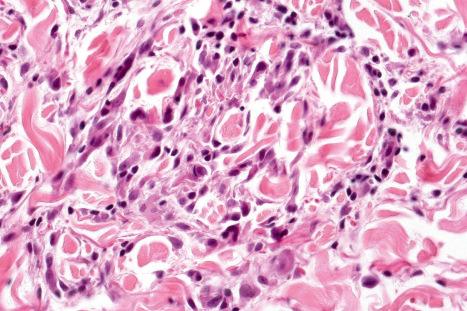
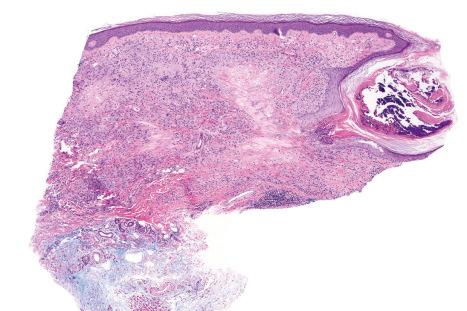
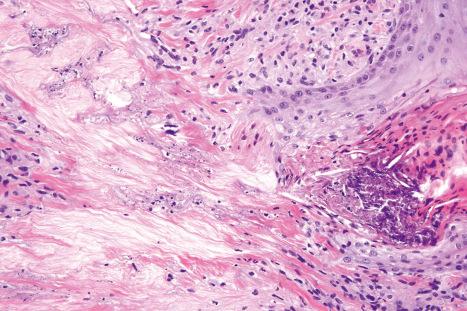
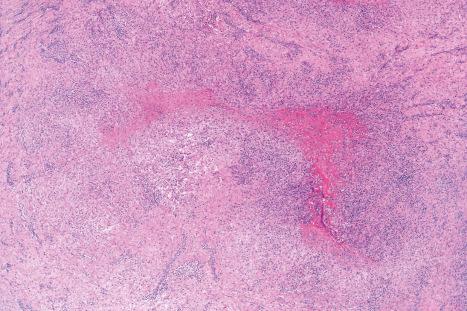
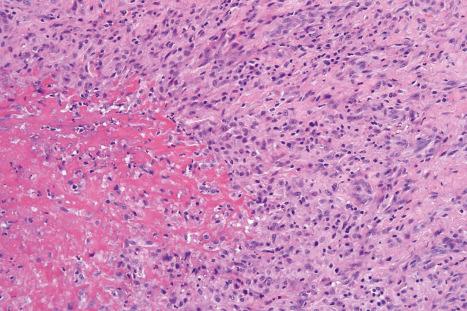
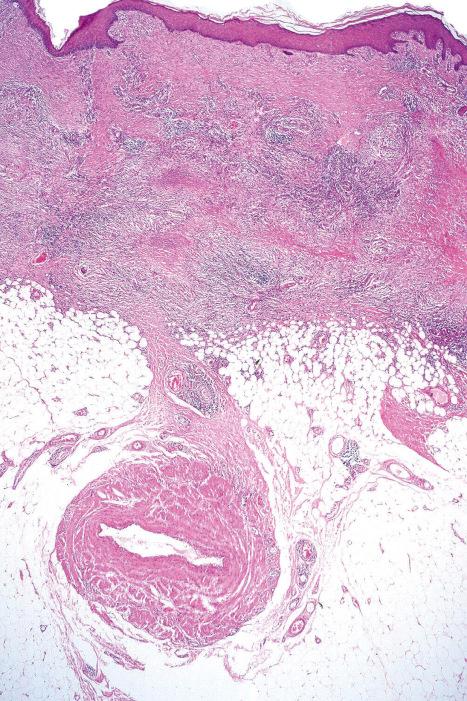
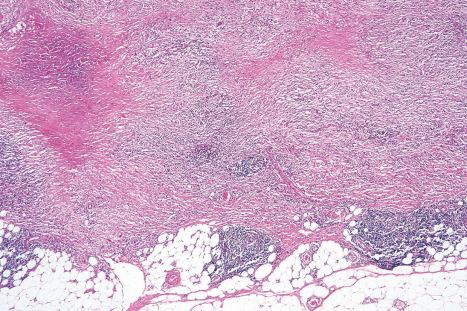
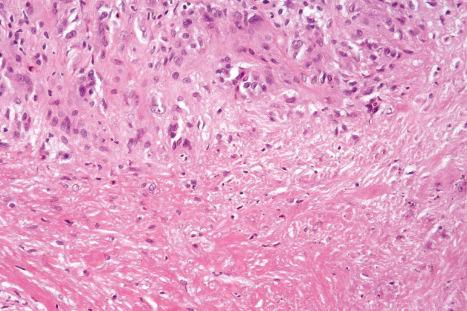
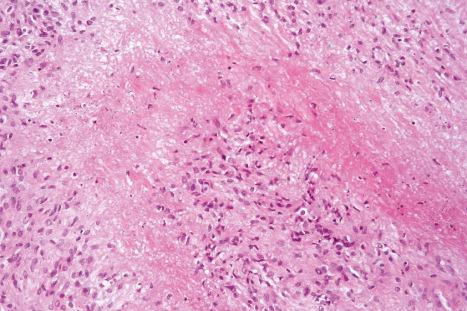
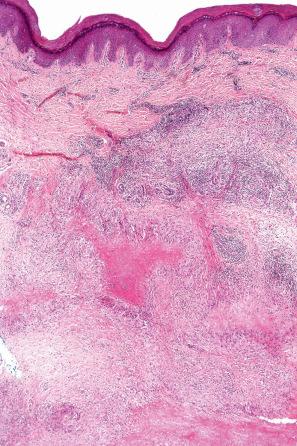
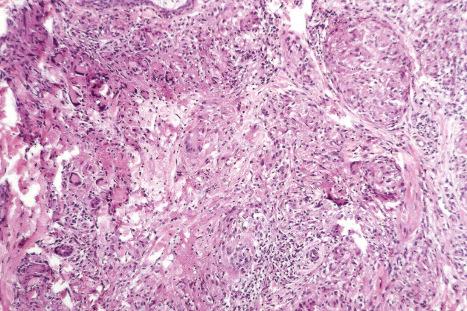
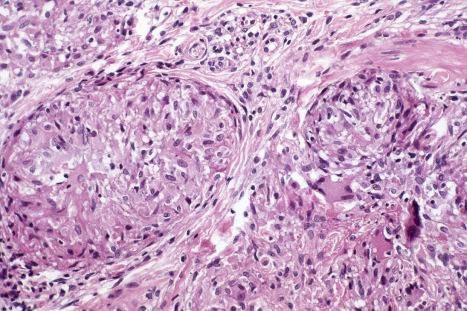
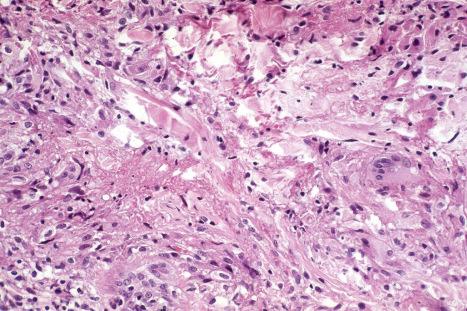
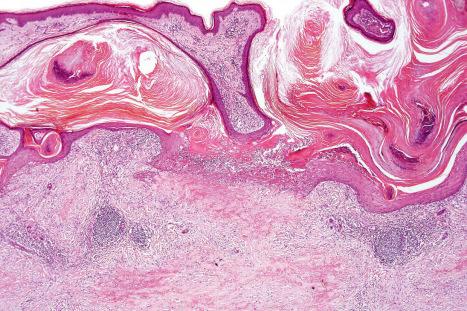
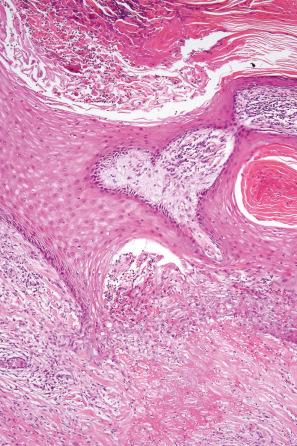
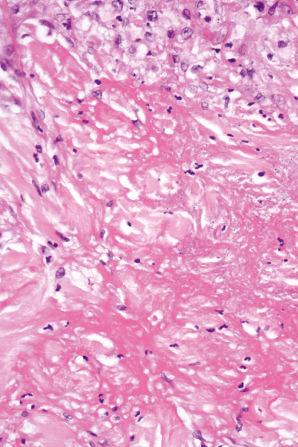
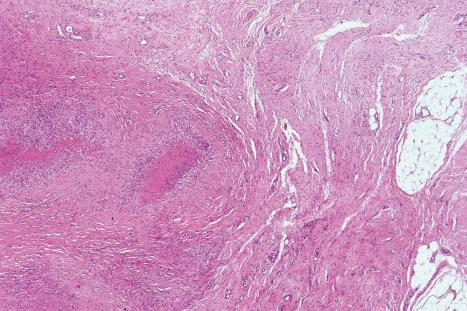
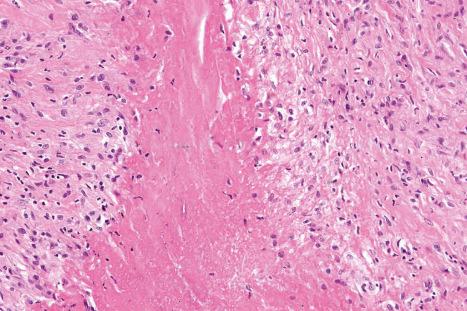
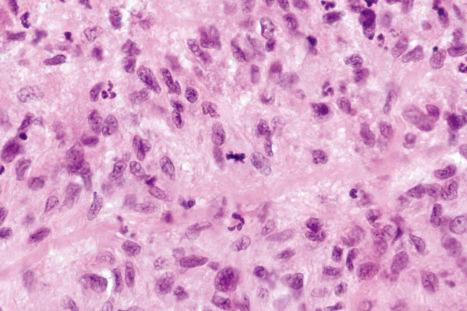
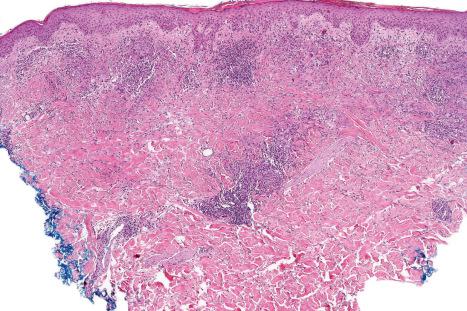
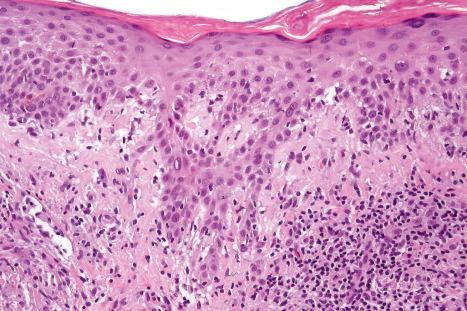
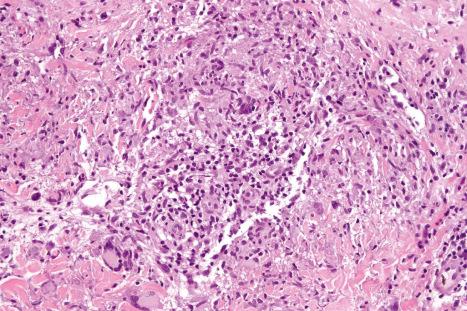
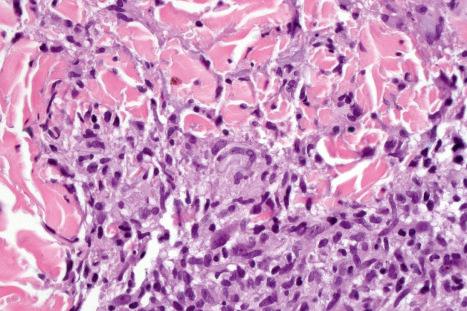
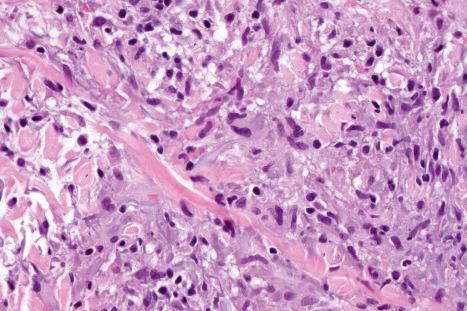
Histologically, sarcoidosis is characterized by a dense, noncaseating granulomatous infiltrate in the dermis ( Figs 9.17 and 9.18 ), which sometimes extends into the subcutaneous fat. The granulomata are discrete and strikingly uniform in size and shape. They are composed of epithelioid histiocytes with abundant eosinophilic cytoplasm and oval or twisted vesicular nuclei often containing a small central nucleolus ( Fig. 9.19 ). Variable numbers of Langhans giant cells are present, and sometimes a scattering of lymphocytes is seen at the peripheral margin of the granuloma ( Fig. 9.20 ). Discrete small central foci of fibrinoid necrosis are sometimes present but caseation necrosis is rare ( Fig. 9.21 ). Transepidermal elimination may be seen and seems more common than previously reported. The epidermis is usually normal although occasional cases display acanthosis and sometimes the granulomata are focally lichenoid. A predominantly lichenoid pattern may exceptionally be seen. A rare syringotropic variant with decreased sweating has been described. Exceptional cases of sarcoidosis may display histologic findings that focally overlap with granuloma annulare palisading neutrophilic and granulomatous dermatitis. Further histologic findings described include elastophagocytosis, perineural granulomas resembling leprosy, mucin deposition, and an infiltrate rich in plasma cells.
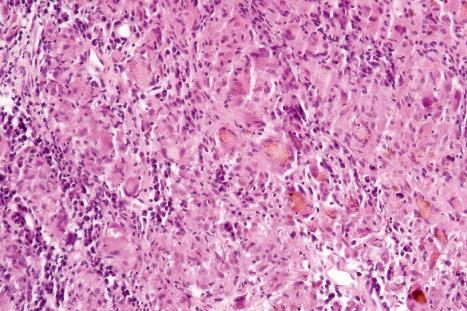
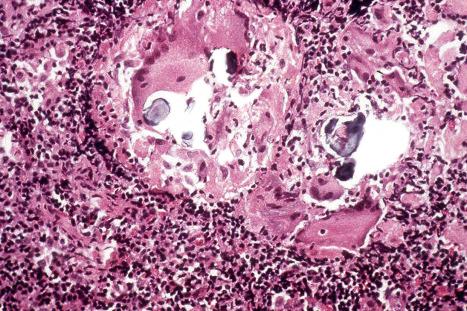
In some cutaneous lesions, inclusion bodies are present, although much less frequently than in lymph nodes. The Schaumann body, a basophilic, laminated, rounded, conchoidal structure composed of calcium carbonate, calcium oxalate, phosphate, iron, and dolomite, is not specific for sarcoidosis and is seen in a number of other granulomatous conditions including tuberculosis and berylliosis ( Fig. 9.22 ). The asteroid body is a small intracytoplasmic eosinophilic star-shaped structure; it is not specific for sarcoidosis, being seen also, for example, in tuberculosis, tuberculoid leprosy, berylliosis, and atypical facial necrobiosis. It is also commonly found in necrobiotic xanthogranuloma. Initial studies suggested that the asteroid body was composed of collagen, but more recent reports, using immunohistochemistry, suggest that it is a product of the microtubular system. The presence of foreign material in sarcoidal granulomata does not exclude the diagnosis of sarcoidosis. In fact, polarizable material has been found in up to 5% of cases.
It has been shown that the gli-1 oncogene is consistently and abnormally expressed in the cells forming the granulomata not only in sarcoidosis but also in granuloma annulare and necrobiosis lipoidica. This observation raises the possibility of trials using inhibitors of gli-1 signaling to treat this group of granulomatous disorders.
The visceral lesions are characterized by an identical histology of noncaseating granulomata, which may be accompanied by significant scarring, for example, in the lung, where advanced cases are characterized by interstitial fibrosis and sometimes honeycomb lung formation. In the liver, granulomata are most commonly found in the portal tracts or in relation to central veins. Splenic lesions are randomly distributed and are not usually associated with significant fibrosis.
Sarcoidosis must be approached as a diagnosis of exclusion and has to be distinguished from the numerous conditions that may be associated with a noncaseating granulomatous histology, including some forms of tuberculosis, tuberculoid leprosy, berylliosis, fungal infections, Crohn disease, and foreign body granulomatous reactions. Therefore, the use of special stains, including the Ziehl-Neelsen preparation for mycobacteria and the periodic acid-Schiff (PAS) and methenamine silver reactions for fungi, is mandatory before diagnosing sarcoidosis. Depending on the clinical context, cultures may also be required to exclude an infective etiology. Tuberculoid leprosy is characterized by nerve involvement, a feature that is usually absent in sarcoidosis.
Some of the granulomata seen in a variety of primary immunodeficiency syndromes closely mimic those found in sarcoidosis, and histologic distinction may be impossible. A study comparing granulomata in sarcoidosis to those seen in primary immunodefiencies found a much lower rate of CD4+/CD8+ cells in the former as opposed to the latter.
Labial and gingival involvement may be histologically mistaken for Crohn disease and granulomatous cheilitis (Miescher). It is worth noting that in rare cases oral involvement in Crohn disease may precede systemic manifestations by several years. Metastatic Crohn disease may be difficult to distinguish from sarcoidosis. The former often shows nonsuppurative granulomata in a diffuse pattern and surrounded by a thin cuff of lymphocytes. Further frequent findings include the presence of numerous eosinophils and ulceration, findings not often seen in sarcoidosis.
Granulomatous lesions that have been described in exogenous ochronosis appear to be related to sarcoidosis. However, similar lesions have also been described as showing changes mimicking actinic granuloma.
Granuloma annulare is a common, usually asymptomatic, dermatosis of unknown etiology. It may be divided into six clinical subsets:
localized,
generalized,
perforating,
subcutaneous,
papular,
linear.
Unusual clinical variants include pustular follicular lesions and presentation with patches. A single case presenting as contact dermatitis has been reported. Granuloma annulare (often with widespread disseminated lesions) has been described in patients with HIV infection and sometimes may be the presenting sign. Granuloma annulare, mainly the generalized variant (see below), has also been reported in association with both Hodgkin and non-Hodgkin lymphoma. Exceptionally, anterior uveitis and concomitant skin lesions have been described. A case of oral granuloma annulare has been described.
Other documented associations of granuloma annulare include morphea, chronic hepatitis C infection, autoimmune thyroiditis, secondary hyperparathyroidism, sarcoidosis, Plummer disease, myelodysplastic syndrome, metastatic carcinoma, and a bee sting. Granuloma annulare has also been described after vaccination for tetanus and diphtheria, hepatitis B, and tuberculosis (BCG), and after mesotherapy. It may also develop in the scars of herpes zoster. It is important to highlight that most patients with the condition heal after variable periods of time, and long follow-up has not revealed consistent associations with any systemic diseases. A further study has found no consistent relationship between malignant neoplasms and granuloma annulare. However, it has been suggested that elderly patients with lesions that do not have typical features of granuloma annulare but display microscopic findings resembling granuloma annulare should be investigated for an underlying malignancy, especially lymphoma.
Granuloma annulare has developed during treatment with allopurinol, amlodipine, daclizumab, antitumor necrosis factor agents, thalidomide, vemurafenib, pegylated interferon alpha and topiramate. Interferon-alpha has been associated with generalized interstitial granuloma annulare. It is most likely, however, that granuloma annulare-like eruptions secondary to drug administration often represent interstitial granulomatous drug eruptions.
The localized variant is the most common type. It usually presents in the first three decades and is associated with a female preponderance (2.25 : 1). Lesions consist of one or several papules, which may be skin-colored, red, or violaceous, and are typically distributed to form an annular or arcuate lesion 1–5 cm in diameter ( Figs 9.23–9.27 ). About 50% of patients have solitary lesions. The acral sites are most commonly affected, in particular, the knuckles and dorsum of the fingers. In a small proportion of patients, lesions are present on both the upper and lower limbs, and occasionally the trunk is affected. Lesions on the palms are exceptional. Facial involvement appears to be uncommon. In a reported case, lesions were restricted to the area involved by a Becker nevus. Although lesions may be persistent, approximately 50% of patients can anticipate resolution by about 2 years from onset. However, recurrences are, unfortunately, quite common. Patients in which the disease arises earlier in life appear to have earlier resolution of lesions. Interestingly, on occasion lesions regress spontaneously after biopsy. Spontaneous resolution may rarely result in mid-dermal elastolysis. Rarely, granuloma annulare has been reported in families and in monozygotic twins. A case has been documented in which the lesions recurred seasonally with sun-exposed areas. There has only been a single case report of cutaneous granuloma annulare with similar lesions in an intra-abdominal location. In one case, granuloma annulare was the first sign of adult T-cell leukemia/lymphoma, in another patient it was associated with angioimmunoblastic T-cell lymphoma, and in a further patient it was associated with cutaneous marginal zone lymphoma. Very rarely, acral, localized granuloma annulare may present as an acute and painful eruption. An association with penile lichen sclerosus is exceptional.





Generalized lesions occur in approximately 15% of patients with granuloma annulare. As with the localized form, there is an increased incidence in females; however, the median age differs, the majority of cases occurring in patients in the fourth to seventh decades, with the rest appearing during the first decade. Patients with generalized granuloma annulare have an increased incidence of HLA-Bw35. Generalized granuloma annulare is defined as lesions occurring on at least the trunk and either upper or lower extremities, or both. Most lesions are papules, which may be distributed in an annular pattern, but maculopapules and nodules also occur. They vary in hue from flesh-colored or red, to tan, brown, or yellow. Numbers vary from several dozens to hundreds ( Figs 9.28–9.30 ). A single patient has been documented with generalized disease accompanied by marked swelling of the hands, and another patient developed the disease following erythema multiforme. A further case developed after varicella zoster infection. Lesions may be asymptomatic or pruritic. As with the localized form, the disease is persistent, but some patients experience resolution within 4 years. Anetoderma has been exceptionally reported as a complication of generalized granuloma annulare. A remarkable association with giant cell arteritis, gastrointestinal stromal tumor, and other internal malignancies including ovarian and gastric cancer has been reported. Tuberculous lymphadenits was an association in one case. In two instances, the condition was the initial manifestation of chronic myelomonocytic leukemia. An association with lymphoma, including Hodgkin disease, has also been described. A patient with hepatitis B developed generalized granuloma annulare, and viral DNA was detected in the skin lesions by PCR. A further case presented in a photosensitive distribution and healed with scarring and milia formation. Other rare associations include hyperlipidemia and scabies.



Perforating granuloma annulare is distinguished by the presence of transepidermal elimination of necrobiotic collagen. Clinically, the lesion presents as a group of papules with an umbilicated crust usually located on the extremities, often the dorsum of the hands ( Fig. 9.31 ). Presentation of lesions on the ears has exceptionally been described, as has a generalized variant. It may affect both children and adults, and both localized and generalized forms exist. Spontaneous resolution sometimes occurs within months or years of onset. Exceptionally, perforating granuloma annulare develops following tattooing.

The subcutaneous variant is synonymous with the pseudorheumatoid nodule of childhood and deep granuloma annulare. Lesions may present de novo or arise in association with typical cutaneous papules. In about a quarter of patients, there is coexistence with dermal granuloma annulare. It occurs in childhood, often affecting the underlying periosteum and involving predominantly the lower legs (particularly the tibia), feet, buttocks, hands, and head. Lesions may also present on the penis or eyelid. An exceptional case of numerous lesions limited to the scalp of a child which regressed spontaneously has been reported. A further patient presented with a periorbital subperiostal lesion, and in another patient the lesion was congenital. In one study of 47 patients, the mean age was 4.3 years. In some instances, there is a history of trauma. By definition, such children do not have rheumatoid arthritis or rheumatic fever. The lesion usually regresses after several years. However, recurrences appear in 19% of patients.
Papular granuloma annulare presents as flesh-colored or hypopigmented, 1–3-mm-diameter papules on the dorsal aspect of the hands, usually in male children. Involvement of the palms and soles may be seen, and rarely lesions are painful. Occasional lesions may be umbilicated or generalized ( Figs 9.32 and 9.33 ).


The linear variant is very rare and may have a bilateral distribution. Rarely, it may follow Blaschko lines. This variant overlaps and may in some cases be the same as the condition described as palisading neutrophilic and granulomatous dermatitid.
The cause of granuloma annulare is unknown. The original concept that it represented a tuberculid has long since been discounted. Although it has been reported at the site of previous herpes zoster infection and verruca vulgaris, it is unlikely that an infectious pathogenesis exists. Borrelia has been demonstrated by focus-floating microscopy in a number of biopsies of patients with granuloma annulare, raising the possibility of a pathogenetic role for the organism in some cases of the disease. However, a study based on PCR found no association between granuloma annulare and Borrelia infection. There is a wide variety of currently possible pathogenetic mechanisms, most of which have some merit, but none of which satisfactorily clarifies the precise mechanism by which the lesions of granuloma annulare develop. Particularly popular are an immune complex vasculitic process and a cell-mediated delayed hypersensitivity reaction. Evidence in favor of the former has been the detection, by direct immunofluorescence, of immunoreactants (IgM and complement) in blood vessel walls in some patients. Elevated levels of circulating immune complexes have also been recorded. The histology may reveal features suggestive of a vasculitic process, including endothelial swelling, vessel wall thickening (due to the deposition of PAS-positive material), vascular occlusion, and necrosis ( Fig. 9.34 ). All of the latter changes may, of course, develop as a consequence of the inflammatory process rather than cause it. A study of serial sections of 38 biopsies in 35 patients found no evidence of a vasculitic process in any of the cases.
In favor of a cell-mediated delayed hypersensitivity reaction are:
the finding of activated T lymphocytes in lesions of granuloma annulare on electron microscopic examination,
the predominance of T-helper inducer cells in the infiltrate,
the histopathological resemblance of the infiltrate to that of conditions of known delayed hypersensitivity pathogenesis, including sarcoidosis and tuberculosis.
It has been suggested that Th1 lymphocytes expressing interferon-gamma induce a delayed hypersensitivity reaction leading to macrophages becoming aggressive effector cells that express tumor necrosis factor-alpha and matrix metalloproteinases. If tumor necrosis factor alpha plays a role in the induction of the disease, then agents that block this cytokine may be useful in treating the condition. Although some patients respond to these agents, others do not, and the reason for this is not clear. Monozygotic twins with generalized granuloma annulare and the 8.1 ancestral haplotype, a genotype that leads to increased production of tumor necrosis alpha, have responded well to adalimumab.
Patients with granuloma annulare may have raised serum migration inhibition factor activity. Defective neutrophil migration has also been reported. Other proposed pathogenetic mechanisms include collagen damage by macrophage lysosomal hydrolytic enzymes as the initial event, or a primary disorder of collagen leading to an allergic or nonallergic tissue reaction. The increased incidences of diabetes mellitus and HLA-B8 may also be of pathogenetic significance (compare with necrobiosis lipoidica). In a study of a group of pediatric patients with multiple lesions of granuloma annulare, it was found that they had significantly lower serum insulin values than the control group and showed mild impairment of glucose tolerance. However, these children often had a family history of diabetes mellitus.
Although there are reports of generalized granuloma being associated with sunlight, this appears to be of doubtful significance.
It has been shown that the glioma-associated oncogene homologue gli-1, a member of the vertebrate zinc finger transcription factor genes of the gli superfamily, is highly expressed in a number of granulomatous disorders including granuloma annulare. The relevance of this in the pathogenesis of granuloma annulare is not clear, but it raises the possibility of using inhibitors of gli-1 signaling in the treatment of granulomatous noninfectious diseases.
The most characteristic histologic lesion seen in granuloma annulare is the palisading granuloma ( Figs 9.35–9.38 ). This consists of a central core of degenerate (necrobiotic) collagen, surrounded by an often radially arranged infiltrate of lymphocytes, histiocytes, and fibroblasts. Elastic tissue may be absent within these foci and there can be phagocytosis of elastic fibers by giant cells at the periphery of the granuloma ( Fig. 9.39 ). However, altered elastic fibers are not a constant finding. Solar elastosis is not a feature of granuloma annulare. In some lesions, the altered collagen has a somewhat basophilic appearance due to the presence of acid mucopolysaccharides, but more commonly there is eosinophilia, due in part to fibrin deposition ( Fig. 9.40 ). Heparin sulfate is an important component of the mucin in granuloma annulare but not of other cutaneous diseases associated with mucin deposition ( Fig. 9.41 ).

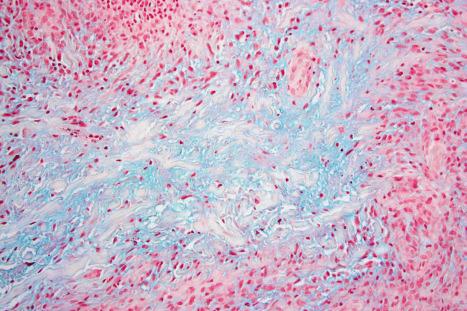
Occasionally, sparse karyorrhectic debris is present in the center of the lesion and sometimes the necrobiotic foci contain lipid droplets. More often, however, the collagenous degeneration is not organized into a nodular pattern, but affects isolated fibers in a random pattern, an appearance often best appreciated on low-power examination ( Fig. 9.42 ). In this so-called diffuse or interstitial form of granuloma annulare, affected fibers, which are swollen and intensely eosinophilic, alternate with apparently normal fibers to give a rather disorganized appearance ( Figs 9.43 and 9.44 ). Necrobiosis is minimal or absent. Characteristically, the collagen fibers are separated by mucin, which stains positively with Alcian blue at pH 2.5. Histiocytes are often seen infiltrating around and between affected fibers, and this feature may be a helpful clue to the diagnosis in early cases when the collagen changes are inconspicuous and should, therefore, encourage examination of additional sections to detect more typical features ( Fig. 9.45 ).
An almost inevitable feature of granuloma annulare is the presence of a perivascular chronic inflammatory cell infiltrate, both within the lesion and in the adjacent tissue. Well-formed sarcoidal granulomata with associated giant cells are seen in some cases. Significant numbers of eosinophils may be encountered. In one study, eosinophils were present in 66% of biopsies, of which 14% showed more than 10 eosinophils per high-power field. Plasma cells are rare, and this is useful in the differential diagnosis with necrobiosis lipoidica (see below). Neutrophils are a rare finding and when present, particularly in association with changes of vasculitis, it is likely that there is an association with systemic disease. Rarely, an associated prominent lymphocytic infiltrate mimicking a lymphoma may be encountered.
Although the relationship with Borrelia infection is debatable, it has been suggested that formation of pseudorosettes in granuloma annulare may suggest infection with the organism.
In perforating granuloma annulare, the necrobiotic debris is present in close proximity to the epidermis and may be seen to be engulfed by the latter to form a perforating channel by which the necrotic material is extruded to the surface ( Figs 9.46 and 9.47 ). If serial sections are performed, the perforation is often shown to occur through a hair follicle.
The subcutaneous lesions are much larger than the superficial ones ( Figs 9.48 and 9.49 ) and are frequently composed of multiple nodules. There is usually massive necrobiosis and abundant mucin; on occasions, lipid droplets are evident. Mucin, however, may be minimal or not apparent and if fibrin deposition is present, distinction from rheumatoid nodule is impossible. A dense rim of lymphocytes, histiocytes, and fibroblasts surrounds the necrobiotic center. Multinucleate giant cells are common and eosinophils are often present. The latter appear to be more common in this variant than in ordinary granuloma annulare. Fibrosis of the surrounding tissue may be marked. In up to 25% of cases of subcutaneous granuloma annulare, changes of classic granuloma annulare may be seen in the dermis.
Papular and linear variants show histologic features similar to those described for typical granuloma annulare.
Granuloma annulare must be distinguished from necrobiosis lipoidica, rheumatoid nodule, actinic granuloma, and granuloma multiforme. Points of distinction are summarized in Table 9.1 .
| Granuloma annulare (GA) | Subcutaneous GA | Perforating GA | Necrobiosis lipoidica (NL) | Atypical NL | Rheumatoid nodule | Actinic granuloma | Granuloma multiforme | |
|---|---|---|---|---|---|---|---|---|
| Epidermis | Normal | Normal | Transepidermal elimination | Normal or atrophic or acanthotic | Normal | Normal | Normal or atrophic | Normal |
| Location of lesion | Superficial dermis | Deep dermis and subcutis | Superficial dermis | Deep dermis and subcutis | Upper and mid dermis | Deep dermis and subcutis | Upper and mid dermis | Upper and mid dermis |
| Necrobiosis | Circumscribed or ill defined | Massive sharp border | Circumscribed | Diffuse and marked | Rarely present | Massive sharp margin | Absent | Focal |
| Mucin | Common | Abundant | Common | Variable | Absent | Common | Absent | Present |
| Lipid | Occasional | Variable | Variable | Common | Absent | Variable | Absent | Absent |
| Fibrosis | Absent | Marked | Absent | Common; may be marked | Absent | Common | Usually absent | Slight |
| Loss of elastic | Yes | Yes | Yes | Yes | Yes | Yes | Very marked | Yes |
| Vascular thickening | Common | Variable | Minimal | Common | Absent | Variable | Absent | Absent |
| Capillary hyperplasia | Absent | Common | Absent | Variable | Absent | Common | Absent | Absent |
| Giant cells | Relatively few | Common | Relatively few | Common | Common | Relatively few | Abundant; contain elastica | Common |
| Asteroid bodies | Absent | Absent | Absent | Absent | Present | Absent | Not uncommon | Absent |
| Palisading of histiocytes | Common | Common | Common | Variable degree in | Absent | Common | Infrequent | Inconspicuous |
The pattern of adipophilin expression has been reported as useful in the histiological distinction between granuloma annulare, necrobiosis lipoidica, and sarcoidosis. In granuloma annulare, adipophilin staining pattern is both intra- and extracellular in relationship with the histiocytes in the infiltrate. In necrobiosis lipoidica the staining pattern tends to be exclusively extracellular in areas of abnormal collagen, and in sarcoidosis the staining pattern is usually exclusively intracellular within histiocytes.
Occasionally, granuloma annulare may display epithelioid cell granulomas mimicking sarcoidosis. However, the presence of mucin in the background along with other more typical changes of granuloma annulare allows distinction in challenging cases.
Granuloma annulare-like lesions with the added features of vasculitis and a significant component of acute inflammatory cells may be encountered in the setting of systemic disease. This pattern of disease is discussed in detail in the section on palisaded neutrophilic and granulomatous dermatitis and related disorders.
Granuloma annulare-like drug eruptions have been reported. The presence of associated interface changes favors a drug eruption.
Very rarely, scleromyxedema may focally mimic interstitial granuloma annulare histologically. However, the changes simulating granuloma annulare are focal, and elsewhere in the biopsy there are more typical features of scleromyxedema including fibrosis and increase in fibroblasts.
Occasionally, infection by Mycobacterium marinum may mimic interstitial granuloma annulare. The microscopic features may be so similar that the diagnosis can only be made by special stains and culture.
Although epithelioid sarcoma, with its associated geographic necrosis, may bear a superficial resemblance at low-power examination to granuloma annulare, the degree of nuclear atypia and pleomorphism in the former condition should afford their distinction in the majority of cases. In addition, epithelioid sarcoma often shows perineural tumor infiltration. It should be noted, however, that mitotic activity may be encountered in granuloma annulare. In difficult cases, keratin, epithelial membrane, in up to 60% of cases, CD34 antigen immunoreactivity and loss of INI1 expression in epithelioid sarcoma should assist in this differential diagnosis.
Rare cases of mycosis fungoides may be associated with a tissue reaction resembling granuloma annulare. Although interstitial mycosis fungoides may show histiocytes between collagen bundles, the predominance of interstitial lymphocytes with nuclear atypia and epidermotropism, a feature not seen in granuloma annulare, should resolve this differential diagnosis. Most patients with interstitial mycosis fungoides have other classical clinical features of the disease. Of interest, interstitial tumor cells in cutaneous T cell lymphoma often have a cytotoxic phenotype.
Acrodermatitis chronica atrophicans can rarely display histologic changes resembling granuloma annulare. However, clinicopathological correlation and the presence plasma cells in the former usually allows distinction to be made.
Necrobiosis lipoidica is a disease of unknown etiology which shows a strong association with diabetes mellitus. Although the affiliation is likely to have pathogenic implications, the precise mechanism by which the lesions of necrobiosis lipoidica develop is, nevertheless, unknown, and the nature of the relationship between the two diseases is unclear. Therefore, although the diagnosis of diabetes is most often established before the onset of the skin lesions (in up to 62% of cases), in a number of cases, typical plaques present simultaneously (in up to 24% of cases) or may precede (in up to 14% of cases) the apparent onset of diabetes mellitus by several years. The course of the cutaneous disease does not appear to be related to the hyperglycemia, and treatment of diabetes does not affect the outcome of the cutaneous lesions. In one study, proteinuria, retinopathy, and smoking were more common in patients with necrobiosis lipoidica compared with patients with diabetes but no skin disease. In another study, patients with diabetes type I and necrobiosis lipoidica tended to have higher levels of glycemia, and the duration of the diabetes was longer compared to patients without necrobiosis lipoidica. Interestingly, however, only a minority of patients with necrobiosis lipoidica has diabetes mellitus. It has been shown that 11% of patients with necrobiosis lipoidica have diabetes mellitus and a further 11% develop the disease or altered glucose tolerance on follow-up.
Necrobiosis lipoidica may develop in both juvenile (type I) and maturity-onset (type II) diabetes. Interestingly, the condition improves or even resolves in diabetic patients after pancreatic transplant. Necrobiosis lipoidica has been documented in patients with endocrine disorders other than diabetes such as hypo- and hyperthyroidism, and also in association with inflammatory bowel disease and vasculitis. One nondiabetic patient with necrobiosis lipoidica and ataxia telangiectasia has been reported. Exceptionally, necrobiosis lipoidica and granuloma annulare have presented simultaneously. The disease has also been documented in association with sarcoidosis.
Necrobiosis lipoidica shows a marked female preponderance (3.3 : 1), and although a wide age range may be affected, patients present most often in the fourth decade (those associated with diabetes mellitus) or fifth decade (those not associated with diabetes mellitus). The condition is rare in childhood and is often associated with diabetes mellitus. It also appears to be related to underlying renal and retinal disease. Familial cases may also occur, with or without diabetes. A case of monozygotic twins with diabetes mellitus type II and necrobiosis lipoidica has been reported.
The characteristic lesion, sometimes referred to as a sclerodermatous plaque, is round or oval, circumscribed, and often has a slightly elevated rim. It is typically a few millimeters to several centimeters in diameter. Newly acquired lesions are often red-brown in color, but with progression the center of the lesion becomes yellowish and the peripheral border may acquire a violaceous hue. Larger plaques are usually irregular and more variably shaped. Scaling and telangiectasia may become evident. Dermoscopy shows elongated serpentine telangiectasias with a whitish structureless background. Ulceration appears to be relatively frequent and has been reported in up to 13% of patients. It is more common in males and in those with diabetes mellitus. Perforating necrobiosis lipoidica is very rare and may be seen very exceptionally in children. In perforating cases, the clinical appearance may consist of a focal scaly depression or comedone-like lesions. Atypical forms may also be found: patients sometimes manifest papules and nodular lesions, and occasionally plaques resembling granuloma annulare are seen. (It should be noted, however, that rarely these two conditions appear to coexist.) Clinical presentations with papulonecrotic and noduloulcerative lesions mimicking gummata or erythema induratum have been documented, albeit exceptionally. The lesions may be solitary or multiple, often symmetrical, and show a predilection for the lower extremities, in particular, the pretibial area ( Figs 9.50–9.53 ). They can also occur on the arms, hands, fingers, abdomen, nipples, and back; rarely, the face or scalp is affected, in which case diabetes is seldom present. Generalized lesions may exceptionally occur.




The so-called atypical necrobiosis lipoidica of the face and scalp does not represent a variant of necrobiosis lipoidica, and it is more likely to represent a variant of elastolytic granuloma (see page 329 ). The name was chosen because of the coexistence of typical lesions of necrobiosis lipoidica on the shins of one of the patients in the original series. However, most patients do not present with classic lesions of necrobiosis lipoidica elsewhere and the microscopic findings do not resemble the latter entity.
Involvement of the penis with lesions resembling chronic balanitis has been described. Exceptional involvement of the scrotum has also been described. Rarely, lesions are associated with Koebner phenomenon. Necrobiotic and silicotic granulomata developing within phlebectomy scars have also been reported. The condition may also occur in association with surgical scars after appendicectomy and breast reconstruction surgery, exceptionally at the site of a burn and in association with a tattoo.
The disease tends to chronicity. It is of interest that necrobiosis lipoidica has been reported to be associated with cutaneous hypo- or complete anesthesia in both diabetic and nondiabetic patients. One study found loss of nerves within lesions and, based on this finding, the authors postulated that destruction of nerves might explain the sensory loss that is observed in some patients. Hypohidrosis and partial alopecia have also been reported.
Rarely, squamous carcinoma may arise in long-standing lesions. One such case developed in association with perforating necrobiosis lipoidica.
The precise pathogenesis of necrobiosis lipoidica is unknown. Of primary importance is the temporal relationship between collagen degeneration and the inflammatory infiltrate. The close association of necrobiosis lipoidica and diabetes mellitus suggests a causal relationship, but the exact mechanism is uncertain. In the past, some 60% of patients with necrobiosis lipoidica were reported as having coexistent diabetes mellitus. However, its reported prevalence in diabetes is only of the order of 3/1000. Furthermore, a recent study has found that only a minority of patients with necrobiosis lipoidica have diabetes.
It has been suggested that the lesions develop as a consequence of diabetic microangiopathy: the vessel walls in lesions of necrobiosis lipoidica are typically thickened by a diastase-resistant PAS-positive material. This does not explain the development of necrobiosis lipoidica in nondiabetic patients or the absence of the disease in patients with established microvascular lesions. An association with venous insufficiency and hypercholesterolemia has been suggested in a very small group of patients. The significance of this finding is therefore unclear. Study of microcirculation by Doppler flowmetry and oxygen partial pressure in necrobiosis lipoidica lesions in nondiabetics has demonstrated an altered microcirculation. Low oxygen and high carbon dioxide pressures, presumably reflecting ischemia, characterize necrobiotic plaques. Such vascular changes, although possibly causal, could equally well develop as a consequence of the necrobiotic changes. Aberrant platelet aggregation may also play a role in pathogenesis. Platelet survival times are markedly reduced in patients with necrobiosis lipoidica. Whether this is of pathogenic importance is uncertain.
Autoantibodies against cytoskeleton proteins have been observed in sera from patients with necrobiosis lipoidica. These autoantibodies (IgG antitroponin, antidesmin, antikeratin, anti-insulin, antitrinitrophenol, and IgA and IgM antikeratin) were found to be elevated in patients with necrobiosis lipoidica compared with diabetic patients without evidence of necrobiosis lipoidica. What role, if any, these autoantibodies play in the pathogenesis of necrobiosis lipoidica is unclear. Synthesis of collagen by fibroblasts cultured from lesions is decreased compared with fibroblasts from normal skin.
Also of uncertain significance is the reported detection, by immunofluorescence, of immunoreactants (IgM and C3) in blood vessel walls in some cases of necrobiosis lipoidica. Epidermal dendritic S100-positive cells are increased in number. Whether this reflects an immunological aspect to the development of necrobiosis lipoidica has yet to be determined.
Glut-1 (the human erythrocyte glucose transporter) is expressed by the fibroblasts in areas of sclerotic collagen from biopsies of patients with necrobiosis lipoidica. This raises the possibility of an altered transport of glucose in the affected areas contributing to the histopathological features seen in this disease.
Gli-1, the glioma-associated oncogene homologue, has been found to be expressed in a number of granulomatous skin disorders including necrobiosis lipoidica. The explanation for this is not clear, but it suggests that inhibitors of gli-1 may be used in the treatment of the disease.
Recently, spirochetal microorganisms, likely to be Borrelia , have been identified in lesions of necrobiosis lipoidica in patients from central Europe. The significance of this finding is unclear.
The histopathological features are variable, depending to some extent on the presence or absence of coexistent diabetes mellitus. The palisading granuloma with necrobiosis is more typical of the diabetes-related variant, whereas a granulomatous sarcoidal type of reaction is more often a feature of nondiabetes-related necrobiosis. Nevertheless, there is very considerable overlap and in the majority of cases one cannot predict, on histologic grounds alone, which cases are, and which are not, diabetes-related.
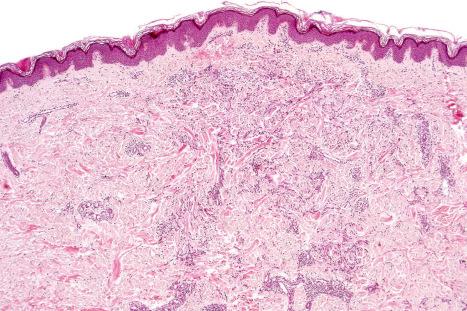
The epidermal changes are usually inconspicuous or absent. There may, however, be acanthosis or atrophy, and hyperkeratosis is not uncommon.
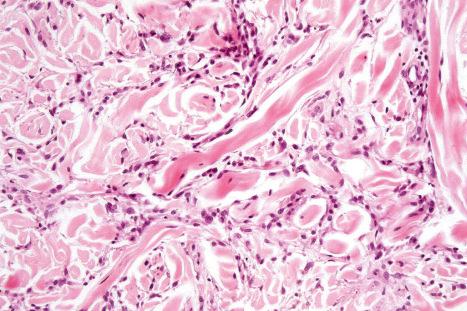
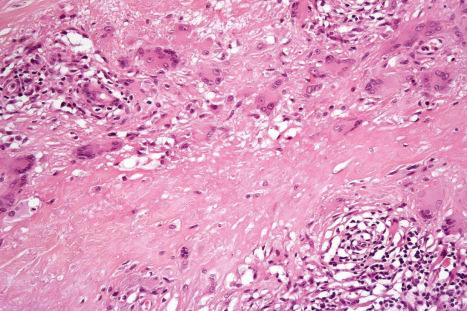
The hallmark of necrobiosis lipoidica is the palisading necrobiotic granuloma. Large, often confluent areas of necrobiosis are present, usually centered in the lower dermis, although the superficial dermis and subcutaneous fat may also be affected ( Figs 9.54–9.56 ). When the subcutaneous fat is involved, the changes are seen mainly in the septa. The foci of necrobiosis consist of eosinophilic, swollen or degenerate collagen, often appearing hyalinized with a surrounding infiltrate of variable numbers of lymphocytes and histiocytes ( Fig. 9.57 ). Aggregates of lymphoid cells, with or without germinal center formation, are frequently found. Plasma cells are almost invariably present. In a single case, the plasma cell infiltrate was monoclonal, and further investigations revealed an underlying monoclonal gammopathy. The necrobiotic foci sometimes contain mucin. Palisading is variable, being more conspicuous in those instances associated with a heavy inflammatory cell infiltrate. The areas of necrobiosis are associated with loss of elastic tissue ( Fig. 9.58 ). Usually, epithelioid histiocytes and giant cells are evident and sometimes there are well-formed granulomata resembling the sarcoidal type of necrobiotic histologic reaction (see below) ( Fig. 9.59 ). Very rarely, asteroid bodies are identified. Lipid droplets, best seen with oil red O or Sudan IV staining on frozen tissue, are almost invariably present in the necrobiotic foci. Usually, a mild to moderate perivascular lymphocytic infiltrate is seen in the adjacent dermis. Cholesterol clefts are rare and only exceptionally may be prominent.
A careful search often reveals vascular changes in necrobiosis lipoidica. These consist of blood vessel wall thickening, with intimal proliferation and narrowing of the lumen. Occasionally, thrombi are noted. Sometimes increased numbers of vessels are a feature. The vascular changes are more obvious in patients with associated diabetes mellitus or other systemic disease. These changes are particularly severe in those cases where necrobiosis is very marked. One study also showed that neutrophilic and granulomatous vasculopathies correlated with systemic disease. In addition, telangiectatic superficial venules are a common feature. Cases with necrobiosis-like features and significant vasculitis and neutrophilic infiltrates in the setting of systemic disease are discussed in detail in the section on palisaded neutrophilic and granulomatous dermatitis associated with systemic disease ( p. 334 ). In lesions with anesthesia, S100 shows destruction of nerve fibers in the areas of necrobiosis.
In the diffuse variant, there is very widespread necrobiosis with a minimal inflammatory cell response; such cases are usually associated with diabetes ( Fig. 9.60 ). Sometimes linear infiltrates of histiocytes between collagen fibers are a feature, as in granuloma annulare. Lipomembranous fat necrosis is noted in occasional cases.
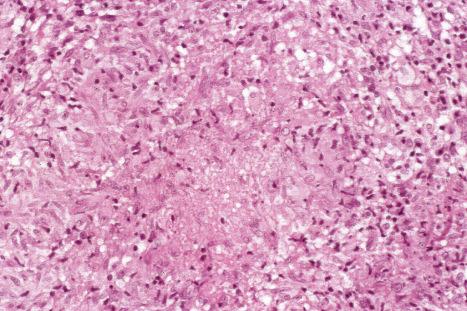
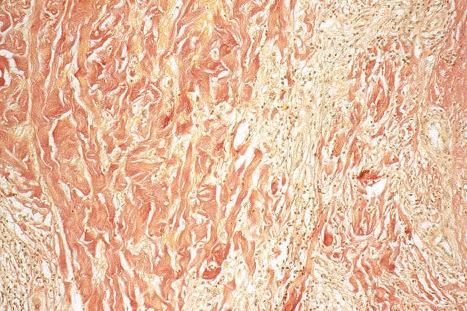
In the sarcoidal type of necrobiosis lipoidica, which is more often noted with the nondiabetes mellitus-associated variant, the appearances are those of naked epithelioid cell granulomata, particularly in the lower dermis ( Fig. 9.61 ). Langhans and foreign body giant cells are usually conspicuous, and a lymphocytic and plasma cell infiltrate may be evident ( Fig. 9.62 ). Necrobiosis is usually minimal; multiple levels may have to be examined before its presence is confirmed ( Fig. 9.63 ). The sarcoidal type of necrobiosis lipoidica in patients without diabetes mellitus has in the past been described as Miescher granuloma.
Perforating necrobiosis lipoidica is associated with transepidermal elimination of necrobiotic collagen and also degenerated elastotic material ( Figs 9.64–9.66 ).
Exceptionally, skin changes at the sites of intravenous drug abuse and leishmaniasis may mimic necrobiosis lipoidica. Histologic changes of both necrobiosis lipoidica and granuloma annulare may exceptionally coexist in a tattoo reaction. A small number of patients reported in a series presented with pretibial lesions suggestive of necrobiosis lipoidica, but on histology, only features of venous insufficiency were observed. The name of pretibial angioplasia has been proposed for this entity.
Necrobiosis lipoidica must be distinguished from granuloma annulare, rheumatoid nodule, actinic granuloma, and granuloma multiforme. Points of distinction are summarized in Table 9.1 . The presence of massive necrobiosis associated with numerous cholesterol clefts, bizarre multinucleated giant cells, and Touton-type giant cells distinguishes necrobiotic xanthogranuloma from necrobiosis lipoidica. As noted above, prominent cholesterol cleft formation, which is a feature that usually suggests necrobiotic xanthogranuloma, may rarely be seen in necrobiosis lipoidica. Small punch biopsies may not be adequate for definitive evaluation, and sampling bias may be misleading. Clinical correlation should be taken into consideration before making a final diagnosis. It has been proposed that the pattern of immunostaining with adipophilin may be of use in the differential diagnosis of granulomatous dermatitis. In necrobiosis lipoidica adipophilin staining is usually limited to extracellular areas in zones of damaged collagen, whereas in granuloma annulare there is extracellular and intracellular staining and in sarcoidosis the staining tends to be intracellular.
Rheumatoid nodules are subcutaneous lesions that develop at sites of trauma or at pressure points in approximately 30% of adults with rheumatoid arthritis. They are most commonly found on the extensor aspect of the forearms and elbows (particularly the olecranon process), the feet, knees, knuckles, buttocks, scalp, and back ( Figs 9.67 and 9.68 ). They have also been described involving a wide variety of other sites, including the abdominal wall, heart (pericardium, myocardium, and valves), larynx, lungs, pleura, splenic capsule, peritoneum, mesenterium, eye, bridge of nose, pinna, ischial tuberosity, thyrohyoid membrane, Achilles tendon, oral mucosa, leptomeninges, lymph nodes, vagina, breast, and conjunctiva. Lesions are often fixed to the underlying periosteum or deep fascia. They present as firm, asymptomatic, dome-shaped masses in the subcutaneous fat or deeper tissues and measure from several millimeters to 5 cm in diameter. Numbers may vary from one to over a hundred. Ulceration sometimes occurs. Intrapulmonary rheumatoid nodules have been exceptionally associated with leflunomide in a patient with rheumatoid arthritis. A rare association with anti-tumor necrosis factor alpha treatment for rheumatoid arthritis has been described. A case of large cavitary pulmonary lesions in a patient with HIV has been reported.


Rheumatoid nodules are more commonly found in patients with severe rheumatoid arthritis and are associated with a high titer of rheumatoid factor, joint erosions, and an increased incidence of rheumatoid vasculitis. They are not, however, specific for rheumatoid arthritis, being found in approximately 5–7% of patients with SLE (although in this condition they tend to be localized about the hands) and occasionally in seronegative ankylosing spondylitis. Clinically similar lesions have also been reported in patients with scleroderma. Presentation of multiple rheumatoid nodules on the fingers in association with little or no arthritis has been described as rheumatoid nodulosis. This, however, can be associated with destructive arthritis. A similar name (cutaneous nodulosis) has been given to the development of multiple small nodules at different sites during methotrexate therapy for rheumatoid arthritis. Etanercept has been linked to the exceptional development of extensive pulmonary nodulosis, while infliximab and the aromatase inhibitor letrozole are associated with accelerated cutaneous nodulosis.
Although these lesions develop at sites of pressure and trauma (implying pathogenetic significance), there is some evidence in support of an immune complex-mediated pathogenesis, as both IgG and IgM have been detected by immunofluorescence in the walls of blood vessels adjacent to rheumatoid nodules. Similarly, both rheumatoid factor and complement have been demonstrated within the substance of rheumatoid nodules. Localization of IgM rheumatoid factor and terminal complement complexes C5b-9 has been demonstrated on the luminal surface of endothelial cells in rheumatoid nodules. C4d has been shown in association with palisading macrophages and in areas of fibrinoid necrosis, further supporting the role of complement activation in the pathogenesis of the lesions. Proinflammatory cytokines and cell adhesion molecules (TNF-α, IL-1β, IL-Ra RNA, E-selectin) have been shown in rheumatoid nodules and are likely to play a role in mediating injury. The expression of cytokines in the rheumatoid nodule is very similar to that in the synovial lining in rheumatoid joints and suggests that the pathogenesis of both is very similar and driven by Th1 lymphocytes. The cytokines involved include IFN-γ, IL-1beta, TNF-α, IL-12, IL-18, IL-15, and IL-10. Although massive central necrosis is predominant, apoptosis has been demonstrated throughout the nodule.
Rheumatoid nodules are typically located in the subcutaneous fat or soft tissues although they may extend into the deeper reticular dermis. This is in contrast to the more superficial location of both granuloma annulare and necrobiosis lipoidica. They are multinodular and associated with very extensive necrobiosis ( Figs 9.69 and 9.70 ). Fibrin deposition is often seen in the center of the nodule. Immunoglobulin, lipid, glycosaminoglycans, and nucleoproteins may also be present. Old lesions are sometimes associated with cyst formation due to liquefactive degeneration of the contents of the nodules. A well-developed palisade of histiocytes and occasional giant cells characteristically surrounds necrobiotic foci and fibrinoid material ( Fig. 9.71 ). Asteroid inclusions are not a feature. The outer layer is composed of vascular granulation tissue, and in older lesions marked fibrosis is a frequent accompaniment. An inflammatory cell infiltrate of lymphocytes, plasma cells, and eosinophils is often present. Leukocytoclastic vasculitis has occasionally been reported to affect the blood vessels in and around early nodules. A rare case with perforation of the epidermis has been documented.

In some cases of deep granuloma annulare, the histologic changes are similar to rheumatoid nodule. Deep granuloma annulare (‘pseudorheumatoid nodule’) tends to have more mucin deposition and less fibrin than typical rheumatoid nodules. Therefore, the latter are referred to as ‘red’ granulomas and the former as ‘blue’ granulomas. However, some rheumatoid nodules do contain mucin. Clinicopathological and serological correlation is advised before establishing a definitive diagnosis.
Compared to rheumatoid fever nodule, rheumatoid arthritis nodules tend to be better circumscribed and surrounded by a well-defined palisade of histiocytes. In addition, the fine fibrinoid strands that form the center of a rheumatic fever nodule contrast with the more dense sheetlike areas of necrobiosis and fibrin deposition in the rheumatoid arthritis nodule.
Patients combining the features of severe rheumatoid arthritis with palisading granulomata accompanied by a neutrophilic infiltrate and leukocytoclastic vasculitis have been described. These lesions are discussed under the rubric of palisaded neutrophilic and granulomatous dermatitis with vasculitis. In short, lesions showing these features may be associated with a number of systemic diseases, including rheumatoid arthritis.
Although epithelioid sarcoma, with its associated geographic necrosis, may bear a superficial resemblance at low power to rheumatoid nodule, the degree of nuclear atypia and pleomorphism in the former should allow easy distinction between these conditions ( Fig. 9.72 ). However, in difficult cases, expression of keratin and epithelial membrane antigen and loss of INI-1 expression in epithelioid sarcoma should assist in the differential diagnosis.
This is a controversial group of diseases, the prototype of which is the actinic granuloma. Other entities that very likely belong to this group include atypical facial necrobiosis lipoidica, Miescher facial granuloma, and granuloma multiforme (see below). It has been suggested that all these conditions represent examples of granuloma annulare occurring in different clinical settings. However, the clinicopathological features are distinctive and the pathological process clearly relates to the primary destruction of elastic fibers by a granulomatous infiltrate. In granuloma annulare, as in diseases such as sarcoidosis, destruction of elastic fibers does not always occur and when it does, it tends to occur focally, developing as a secondary phenomenon.
The term ‘annular elastolytic giant cell granuloma’ has been used to describe not only cases of actinic granuloma but also lesions in which destruction of elastic fibers occurs in the absence of solar elastosis. In fact, some cases present at sites with little sun exposure and the disease may also occur in children. Thus, although the terms actinic granuloma, elastolytic giant cell granuloma, and even elastolytic actinic giant cell granuloma have been used interchangeably in the literature, the latter term should be reserved for elastolytic granulomata occurring in skin without solar elastosis but not restricted to covered skin.
Lesions usually present on the trunk and neck and rarely on proximal limbs. They vary in size but tend to be large. Despite the name annular, some cases present with papules or reticular erythema. In those that are annular, there is an advancing raised border which may be papular. Rarely, lesions are generalized and in one of such cases, the lesions spared the striae distensae. Spontaneous resolution is rare. A reported case describes a lesion that developed at the site of an old burn scar and spread after trauma. In a single report, repigmentation of the gray hairs within the affected area of the scalp has been described, and in a further case the granulomas developed on lesions of vitiligo.
Elastolytic granulomata have rarely been described in association with adult T-cell leukemia lymphoma, primary cutaneous CD4-positive small/medium-sized pleomorphic T-cell lymphoma, acute myelogenous leukemia, monoclonal gammopathy, Hashimoto thyroiditis, temporal arteritis in one case following herpes zoster infection, squamous cell carcinoma of the tonsil, late-onset X-linked dominant protoporphyria, diabetes mellitus, and prostatic cancer. A unilateral lesion developing in a hemiplegic stroke patient has been reported, and in a further patient the lesion developed after the implantation of a pacemaker. Elastolytic granulomata have also been documented in internal organs. The latter, however, probably represents sarcoidosis with prominent elastolysis.
Elastic fibers become altered through an unknown mechanism and appear to induce factor XIIIa-positive cells and CD68-positive macrophages to form granulomata.
Histologic features may be identical to those of actinic granuloma (see below) except for the absence of solar elastosis. Ideally, in annular lesions the biopsy should be a wedge including the center, the advancing edge, and normal skin for comparison purposes. This is not always possible, particularly in lesions that do not have an annular configuration. The center of the lesion is completely devoid of elastic fibers, and there is usually no inflammation. The loss of elastic fibers appears to be irreversible. In the advancing margin, there is a granulomatous reaction with fragmentation and phagocytosis of elastic fibers. In one case, histology showed features of mid-dermal elastolysis leading the authors to suggest that annular elastolytic giant cell granuloma may possibly represent a prodromal or inflammatory stage of the disease. Rarely, sarcoidal granulomas may be a prominent feature.
Many granulomatous reactions, including infections, often display elastophagocytosis. However, in these conditions the change is mild and focal. In granuloma annulare, there is usually very little or no elastophagocytosis, while in annular elastolytic giant cell granuloma there is no necrobiosis, mucin, or palisading granuloma. Although a necrobiotic variant of the condition has been described, it is likely that these represent variants of necrobiotic disorders rather than true elastolytic granulomas.
Actinic granuloma develops on the sun-damaged skin of the neck, face, upper chest, or arms of middle-aged patients. It may also affect the conjunctiva, and a single case affecting the upper lip has been reported. Lesions restricted to the conjunctiva of young women are exceptional. A further case presented as alopecia. The incidence is equal in men and women, and individuals with blond hair and freckled skin are predisposed, particularly those living in sunny climates. An association with the long-standing use of sunbeds and with doxycycline phototoxicity has also been described.
Lesions present as one or more skin-colored or pink papules, which enlarge to form annular or arcuate plaques up to 1 cm in diameter. The edge of the lesion is somewhat raised, forming a border 0.2–0.5 cm in width. These annular plaques enlarge slowly, and the center may gradually clear to appear relatively normal or slightly atrophic with variable depigmentation. Lesions are asymptomatic and there is no evidence of anesthesia. However, there is usually clinical exacerbation associated with sun exposure. They do not develop on non-sun-damaged skin. Spontaneous resolution may take place after months or years.
Bilateral periocular actinic granulomata have been documented in a patient with renal failure. Other rare associations likely to be coincidental include relapsing polychondritis, cutaneous amyloidosis, giant molluscum contagiosum, chronic lymphocytic leukemia, and erythema nodosum.
The pathogenesis of actinic granuloma is poorly understood. It has been suggested that the antigenic stimulus for the formation of granulomata in both actinic granuloma and temporal arteritis is actinically degenerated elastic tissue. Interestingly, phototesting in a single case failed to reproduce the lesions of actinic granuloma.
The features are best appreciated by examination of a radial biopsy through the edge of a lesion and including uninvolved skin. The epidermis may be normal or atrophic. The peripheral unaffected skin shows gross solar (actinic) elastosis ( Figs 9.73–9.75 ). Within the rim of the lesion there is a foreign body giant cell reaction in association with, and engulfing, fragmented elastotic material (elastoclasis) ( Figs 9.76 and 9.77 ). The granulomatous reaction is centered in the zone of solar elastosis and, accordingly, tends to be confined to the superficial dermis. The giant cells may contain asteroid bodies. There is an accompanying chronic inflammatory cell infiltrate composed of histiocytes, lymphocytes, and plasma cells. Necrobiosis is not a feature of this condition. Palisading of histiocytes is either absent or minimal and, if present, is related to the elastotic debris. Dermal mucin does not appear to be increased. Fibroblasts are scant and fibrosis is minimal. In the actinic granuloma, blood vessels appear normal. Within the central zone the collagen appears relatively normal, although it is more obviously horizontally aligned and may appear more closely packed than normal. Slight scarring is present in the central area where elastic tissue is absent.
The facial location, presence of elastophagocytosis, and absence of necrobiosis aid in distinguishing actinic granuloma from other granulomatous lesions. The absence of dermal mucin, necrobiosis, and palisading granuloma and the presence of marked elastoclasis and mild scarring help to distinguish actinic granuloma from granuloma annulare, the disorder that it most resembles.
Despite its name, this is not a variant of necrobiosis lipoidica and deserves separate mention because of its unusual clinical features and distinctive histology. Atypical facial necrobiosis lipoidica, which predominantly affects females (9 : 1), usually develops in the absence of diabetes mellitus, and manifests most often in the fourth decade. Patients present with one or more annular, nonscaling plaques on the upper face and scalp, which typically have slightly raised, relatively uniform borders and measure 1–5 cm in diameter ( Fig. 9.78 ). Although early lesions are erythematous with a brown border, older lesions are characterized by central depigmentation. Atrophy, however, is minimal or absent. Patients may, in addition, show involvement of other sites, including the arms, hands, and trunk. Very rarely, patients have concomitant typical necrobiosis lipoidica on the shins. It is for this reason that the name was originally coined. We now believe, however, that the condition probably has no relationship whatsoever to necrobiosis lipoidica. It is much more likely that it represents a variant of an annular elastolytic granuloma.

The condition is characterized by a dense granulomatous infiltrate, with conspicuous giant cells, involving the dermis ( Figs 9.79 and 9.80 ). The infiltrate has a rather irregular distribution, being dispersed between individual collagen bundles. Occasional circumscribed granulomata may sometimes be a feature. Asteroid bodies are often found in the cytoplasm of giant cells. Typically, there is loss of elastic tissue in the areas of granulomatous inflammation. Rarely, ill-defined foci of necrobiosis are noted ( Fig. 9.81 ), but well-defined palisading granulomata are not present. In cases with coexistent necrobiosis lipoidica, biopsies from the affected areas on the shins show the typical histologic features of this condition.
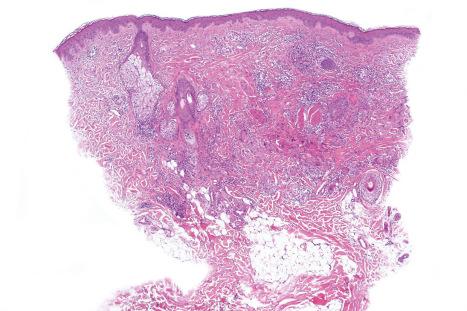
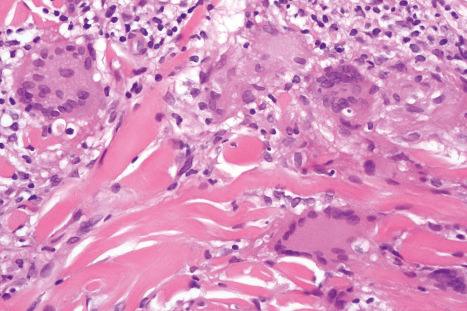
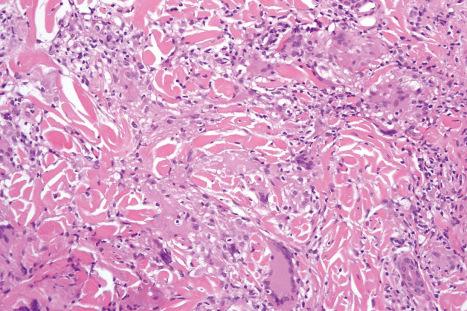
In contrast to actinic granuloma with which this condition is often confused, the surrounding skin does not show evidence of significant solar elastosis and elastoclasis.
This dermatosis of unknown etiology is of particular importance because clinically it can be confused with leprosy; however, it is not associated with cutaneous anesthesia. Granuloma multiforme, which shows a marked female predominance, is seen most often in Central Africa, especially eastern Nigeria. It has also been documented in the Congo, Uganda, India, and Tunisia. The disease is very common in some villages. It particularly affects patients over 40 years of age. Lesions, which tend to chronicity, are found on the upper and exposed parts of the body. They commence as small, flesh-colored, indurated, pruritic papulonodules, 1–8 mm in diameter and raised 1–3 mm above the skin surface, which extend peripherally and coalesce to form annular lesions and plaques ( Figs 9.82 and 9.83 ). Very large lesions become irregular and develop scalloped or gyrate borders. Central healing may be associated with residual hypopigmentation.


The epidermis is normal. Situated within the dermis is an ill-defined, irregular, necrobiotic lesion ( Fig. 9.84 ). In general, this affects individual collagen fibers, producing a rather haphazard picture of abnormal fibers interspersed with unaffected ones and associated with a histiocytic infiltrate ( Fig. 9.85 ). Only rarely is a well-defined palisading granuloma seen. In addition to histiocytes, giant cells are commonly found and the tissues show a perivascular lymphocytic infiltrate with variable numbers of plasma cells and eosinophils. The giant cells do not contain asteroid bodies. Perineural involvement is not a feature. The adjacent vasculature is normal. Loss of elastic tissue is typical in relation to the inflammatory infiltrate, and healed areas are characterized by absence of elastic tissue and mild superficial scarring ( Fig. 9.86 ).
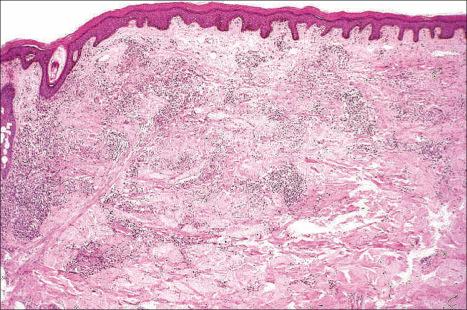
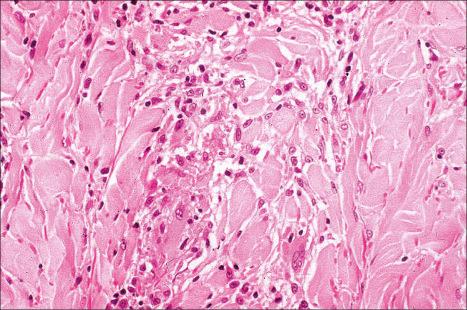
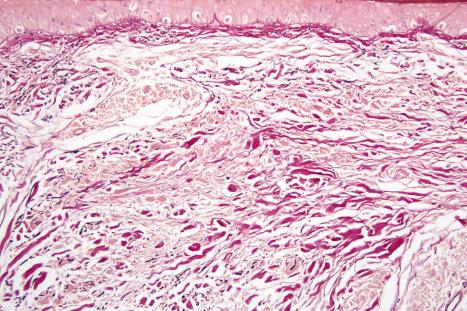
The exact nosological position of granuloma multiforme is unknown. It is probably a clinicopathological variant of elastolytic granuloma. An association with sun exposure has been suggested. The granulomata do not show a perineural distribution, thus helping to distinguish granuloma multiforme from leprosy. Nevertheless, since infection must be excluded before giving a definitive diagnosis, stains for organisms (especially mycobacteria and fungi) must be performed to exclude this possibility. Culture should also be performed when clinically appropriate.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here