Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Surgical management of athletic injuries of the elbow necessitates a detailed understanding of the intricate anatomy and the complex range of functions of the elbow. This chapter provides a detailed, technical anatomic overview. Following surgical intervention, return to function of the elbow is dependent on successful rehabilitation; an understanding of these principles is requisite of surgeons.
The flexion crease of the elbow is in line with the medial and lateral epicondyles and reflects the axis of the elbow joint
The articular surface of the distal humerus is rotated approximately 30 degrees anteriorly with respect to the long axis of the humerus.
The radial head has 240 degrees of articular cartilage that articulates with the ulna at the lesser sigmoid notch, leaving 120 degrees that is non-articular and amenable to instrumentation; this is often termed as the “safe zone.”
In the aspiration and injection of olecranon bursitis with corticosteroid, it is key that the needle enter the skin in a separate location from the bursa to avoid a continuous soft tissue tract to prevent chronic drainage.
The initial diagnosis, severity, and patient postoperative functional goals must be taken into consideration for rehabilitation prior to surgical intervention.
Fundamental principles for elbow rehabilitation include establishing consistent regulation of pain and inflammation, implementation of early atraumatic motion, restoration of neuromuscular control, and integration into the kinetic chain.
Surgical management of athletic injuries of the elbow necessitates a detailed understanding of the intricate anatomy and the complex range of functions of the elbow. The ability to comprehensively diagnose and accurately treat all forms of elbow pathology is incumbent on the clinician. Ranging from arthroscopic management to mini-open and extensile exposures, there are a variety of orthopedic procedures that can be performed pertaining to the elbow joint. This chapter will focus on initially outlining the detailed anatomy of the elbow with an emphasis on surgical pearls. This will be followed by an overview of the principles of elbow rehabilitation, an understanding of which is requisite for the surgeon prior to operative intervention.
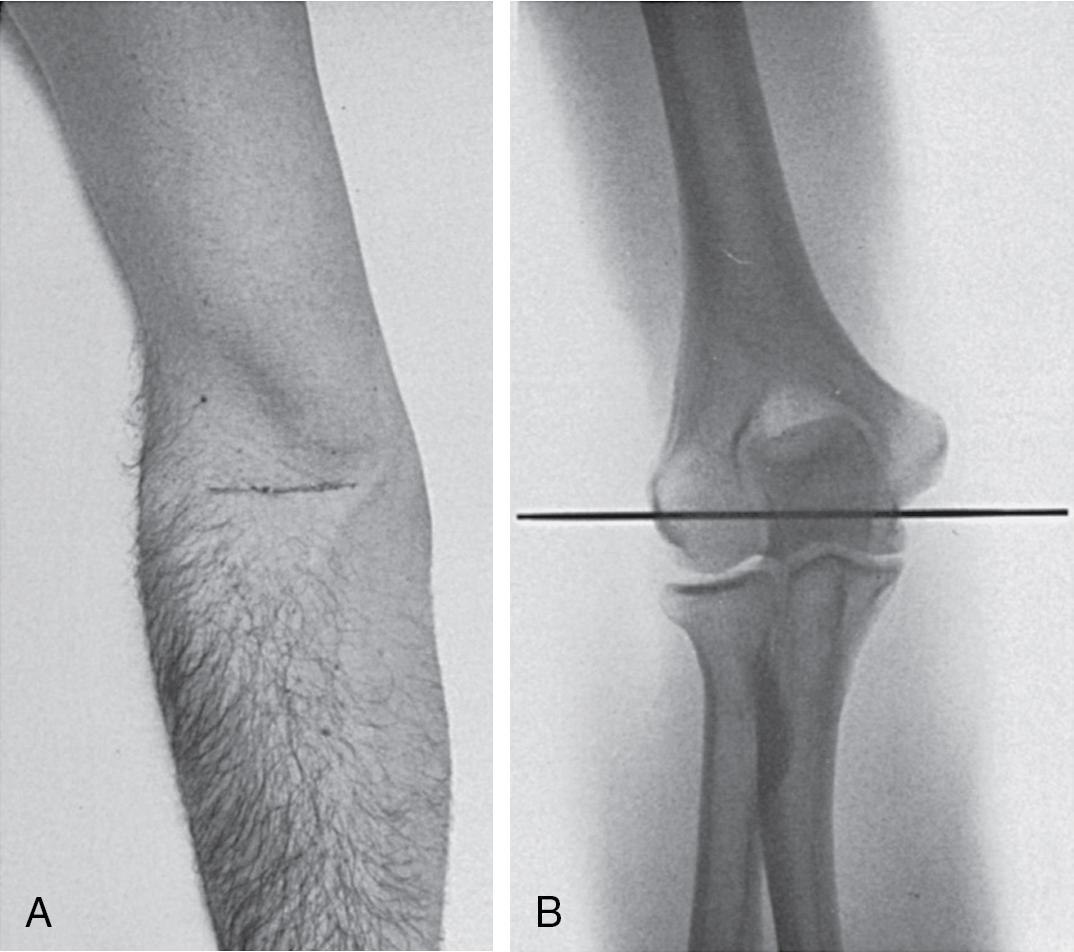
The visual anatomy of the elbow surface merits understanding to guide intervention. The lateral aspect of the elbow is an avascular interval between the brachioradialis and the triceps, delineating the lateral column; a key palpable landmark for surgical exposure. Laterally, the proximal olecranon, the lateral epicondyle, and radial head generate an equilateral triangle which is an important landmark for joint aspiration and elbow arthroscopy. It is important to note that the flexion crease of the elbow is in line with the medial and lateral epicondyles and reflects the axis of the elbow joint. Notably, with the elbow in terminal extension the elbow flexion crease is 1 to 2 cm proximal to the ulnohumeral articulation ( Fig. 42.1 ). ,
Elbow stability is comprised of static and dynamic constraints which are a combination of osseous and capsuloligamentous structures. The primary static constraints of the elbow include the ulnohumeral articulation, the anterior bundle of the ulnar collateral ligament (UCL), and the lateral collateral ligament (LCL) complex. , The secondary static constraints include the common extensor and flexor pronator tendon origins, the joint capsule, and the radiocapitellar articulation. Dynamic elbow stability is a consequence of the surrounding musculature, which includes the brachialis, biceps brachii, triceps, flexor-pronator mass, brachioradialis, extensor carpi radialis brevis (ECRB), and longus.
The distal humerus ( Fig. 42.2 ) is composed of two condyles that form an arch which supports the articular elements of the trochlea and capitellum. The trochlea is a pulley-shaped surface that articulates with the semilunar notch of the ulna and is covered with articular cartilage through an arc of 300 degrees. The medial contour of the trochlea is larger and projects more distally than the lateral portion of the trochlea. The capitellum is a spheroidal structure covered by articular cartilage. There is a groove intervening the capitellum and the trochlea with which the radial head articulates through the arc of flexion as well as pronation and supination. In the sagittal plane, the articular surface of the distal humerus is rotated approximately 30 degrees anteriorly with respect to the long axis of the humerus. In the axial plane the articular surface and axis of rotation are rotated outwards at approximately 5 degrees. The humerus is tilted in approximately 6 degrees of valgus in the coronal plane.
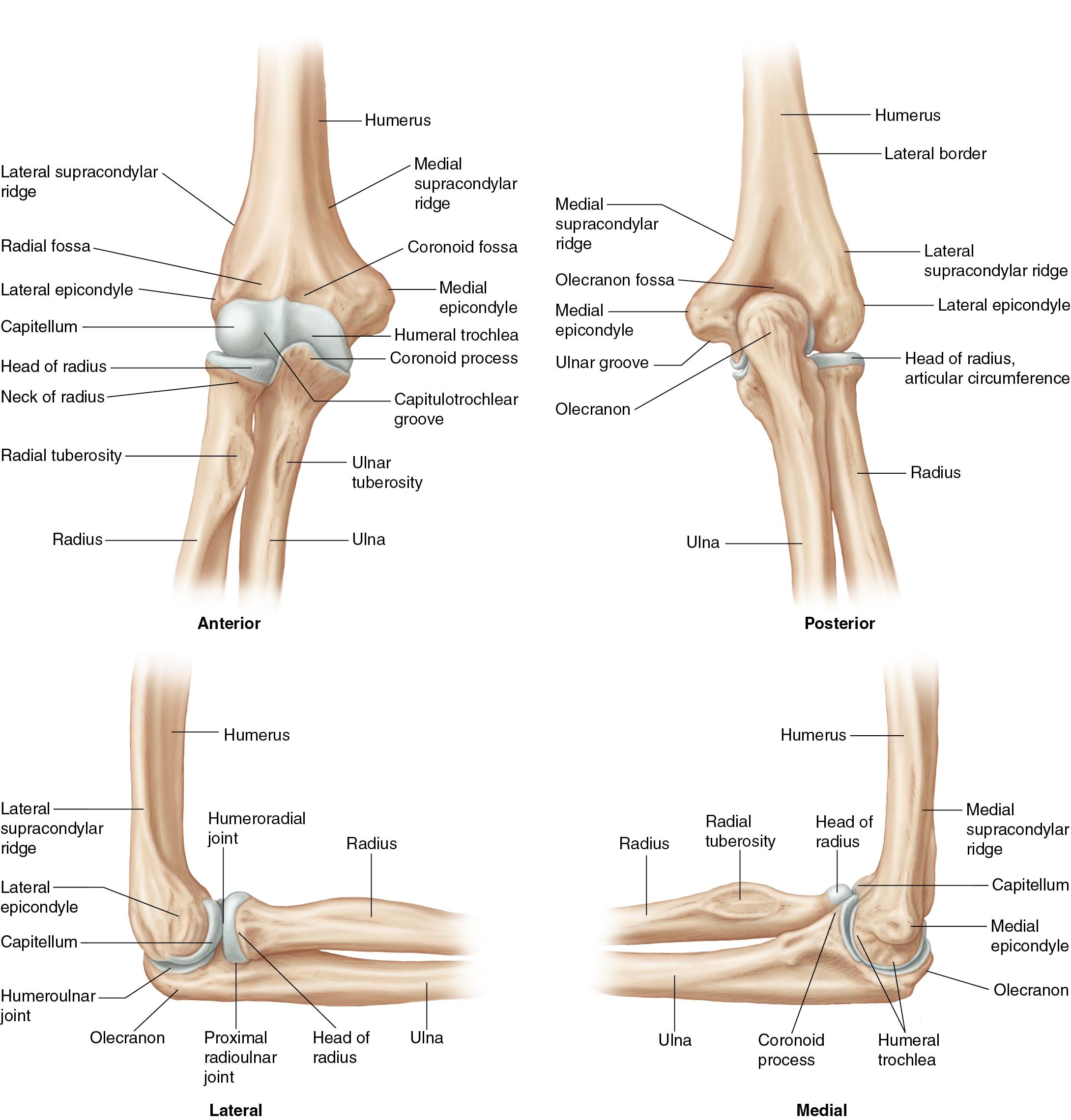
The medial epicondyle protrudes as an attachment site for the medial collateral ligament and the flexor pronator muscle mass. On the lateral aspect, the flatter lateral epicondyle is proximal to the capitellum and serves as the attachment site for the lateral ulnar collateral ligament (LUCL) and the supinator-extensor muscle group. The posterior aspect of the humerus contains the olecranon fossa which serves to articulate with the olecranon tip in terminal elbow extension. Anteriorly, the radial and coronoid fossae accommodate the radial head and coronoid process during flexion.
The elliptical radial head articulates with the capitellum via a cylindrical and symmetric concavity which is covered in entirety with articular cartilage. The radial head also has 240 degrees of articular cartilage that articulates with the ulna at the lesser sigmoid notch, leaving approximately 120 degrees that is non-articular and amenable to instrumentation for open reduction internal fixation (ORIF) of a fracture; this is often termed the “safe zone.” The lesser sigmoid fossa forms an arc of approximately 60 to 80 degrees, leaving a 180 degrees range for pronation and supination. The radial head and neck form a 15 degrees angle in reference to the radial shaft, directed away from the radial tuberosity. ,
Distally, the radius tapers to form the radial neck and culminates in the radial tuberosity at the distal neck. The anterior surface of the radius is covered by a bicipitoradial bursa protecting the biceps tendon during full pronation. The biceps tendon attaches to the roughened surface of the posterior aspect of the radial tuberosity. During full pronation, the tuberosity becomes a dorsal structure which facilitates a posterior approach for repair.
The proximal ulna provides the greater sigmoid notch (incisura semilunaris) which constitutes the major articulation of the elbow for inherent stability. The cortical surface of the coronoid serves as the site of insertion of the brachialis muscle. Medially the sublime tubercle serves as the insertion site of the medial ulnar collateral ligament (MUCL). The triceps tendon attaches along the posterior aspect of the olecranon process. Laterally, as noted previously the lesser sigmoid notch articulates with the radial head and is oriented perpendicular to the long axis of the bone. Distal progression yields the supinator crest, along which the supinator muscle attaches. There is additionally a tuberosity on the supinator crest that serves as the insertion site for the LUCL.
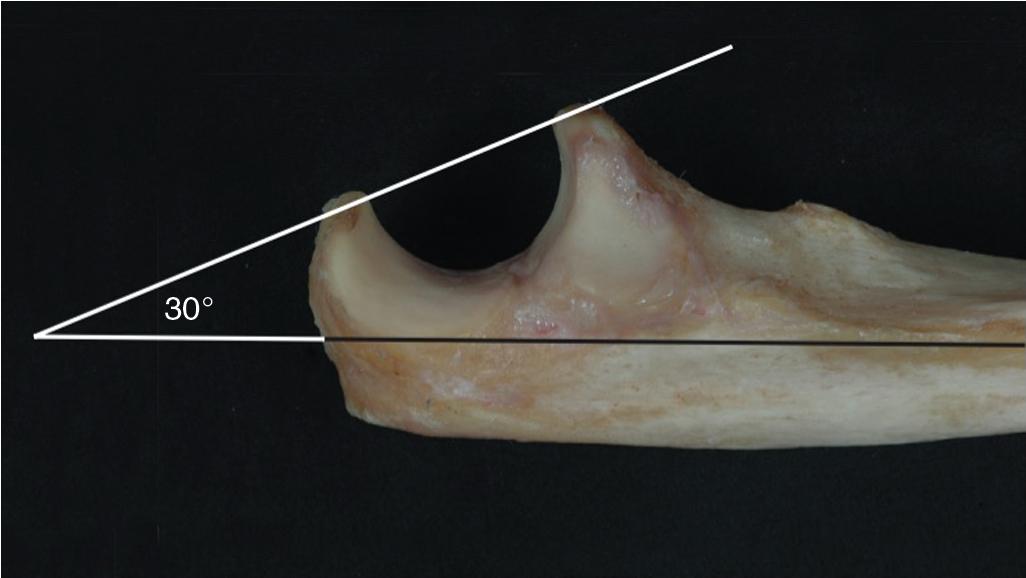
The congruency of the bony articulations of the distal humerus, proximal radius, and proximal ulna is key for an overall stability of the elbow. The proximal ulna is unique in shape with a transverse portion of non-articular cartilage that divides the greater sigmoid notch into the coronoid (anterior) and olecranon (posterior). ( Fig. 42.3 ) In the sagittal plane, the sigmoid notch generates a 190-degree arc that is ellipsoid in shape, facilitating elbow flexion and extension. The greater sigmoid notch has a30-degree posterior tilt in reference to the long axis of the ulna ( Fig. 42.4 ), this matches the 30 degrees anterior angulation of the distal humerus, facilitating terminal extension. In the coronal plane, the carrying angle of the arm is determined in part to a 1 to 6 degrees lateral angulation of the ulnar shaft. , The long axis of the humerus additionally contributes to the carrying angle which is 11 to 14 degrees in men and 13 to 16 degrees in women, typically the dominant arm has a 1 degree greater carrying angle than the non-dominant side.

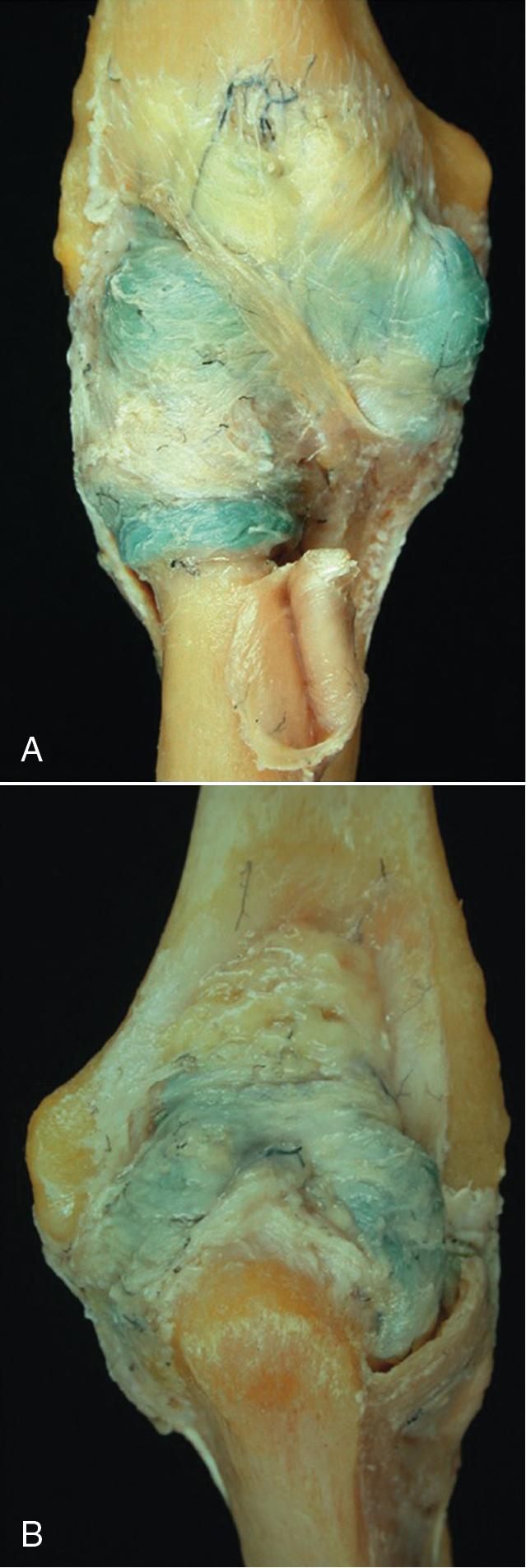
The proximal attachment of the anterior joint capsule is immediately proximal to the coronoid and radial fossae. The capsule extends distally with attachment to the annular ligament laterally and the ulnar coronoid medially ( Fig. 42.5 ). It is important to note that transverse and oblique fibrous bands provide additional mechanical strength to the anterior capsule. The anterior capsule is taut in elbow extension and lax in flexion. It is innervated by variable branches of major nerves traversing the joint, in accordance with Hilton’s law. The posterior capsule traverses from just above the olecranon fossa to the articular margins of the sigmoid notch distally. The elbow joint has a fluid capacity of 25 to 30 mL at 80 degrees of elbow flexion, a useful volume to be mindful of when challenging the elbow joint for suspected traumatic arthrotomy.
Plica synovialis is a fold in the anterior capsule that courses the joint obliquely over the radial head and neck and inserts into the anterior distal capsule near the lesser sigmoid notch. It is a normal anatomic structure with variable prominence that may become thickened and produce symptoms of a snapping elbow.
Specialized thickenings in the medial joint capsule comprise the anterior, posterior, and transverse segments of the MUCL or UCL of the elbow ( Fig. 42.6 ). This complex functions as the primary valgus restraint of the elbow followed by the radiocapitellar articulation and dynamic stabilizers such as the flexor-pronator mass. The anterior and posterior bands provide reciprocal function with the anterior band tight in extension and the posterior band tight in flexion. The transverse component (ligament of Cooper) has minimal contribution to elbow stability. ,
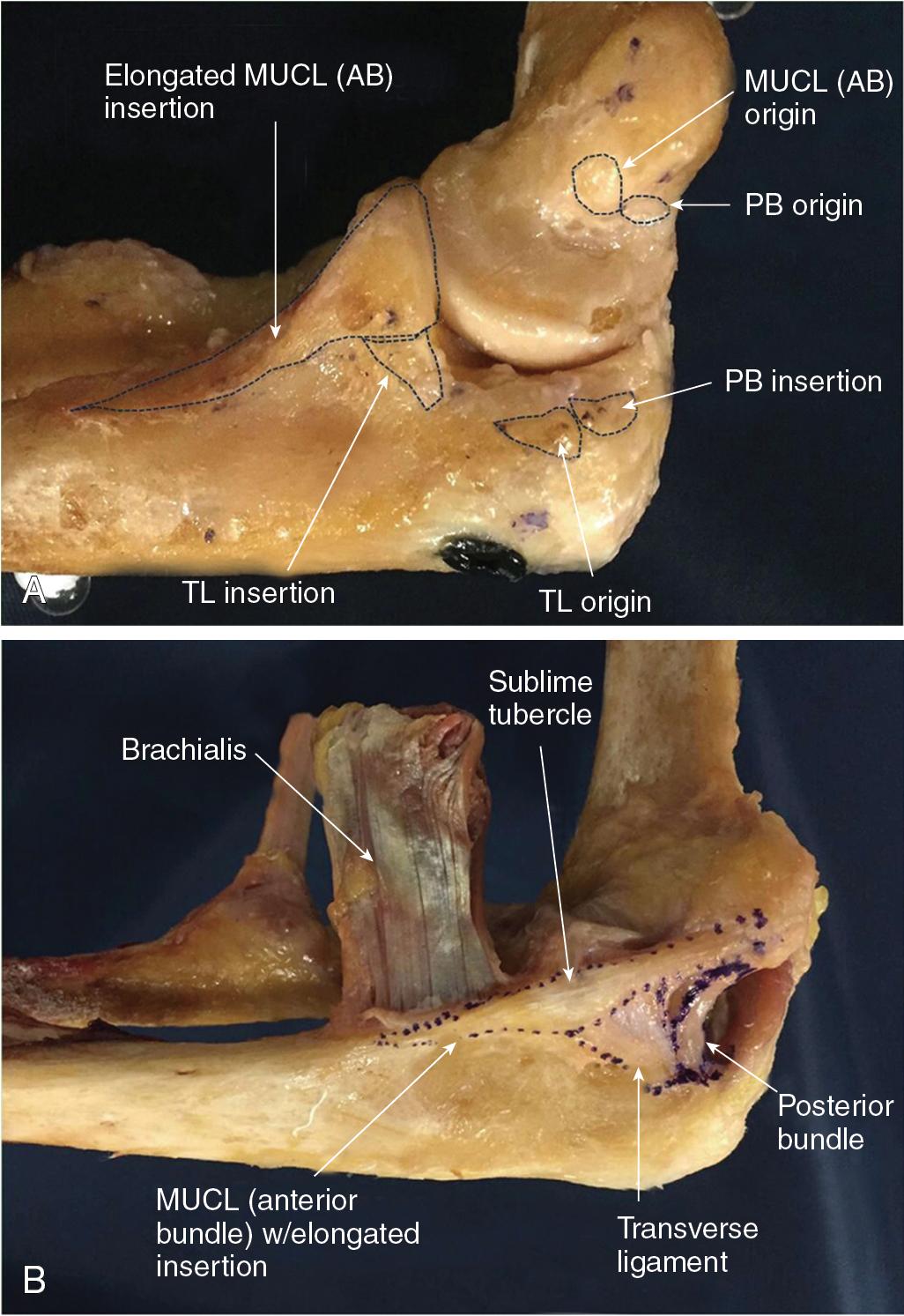
The MUCL originates from a broad attachment on the anteroinferior surface of the medial epicondyle. The surface area of the origin has been variably described in the literature ranging from 17 to 45.5 mm 2 . In the sagittal plane, the anterior bundle of the MUCL is located at the axis of elbow rotation near the anteroinferior margin of the medial epicondyle. The posterior bundle is positioned along the midportion of the medial margin of the semilunar notch. Recent literature , , describes the anterior bundle insertion site as a longer distally tapered segment along the ulnar ridge which encompasses the sublime tubercle with an insertion surface area ranging from 127.8 to 187.6 mm 2 .
The width of the anterior bundle has been demonstrated to range from 4.0 to 7.6 mm. The posterior bundle is measured to be 5 to 6 mm at the midportion of the fan-shaped posterior segment.
In contrast to the medial collateral ligament complex, the lateral ligaments of the elbow follow a less discrete pattern with significant individual variation. It is comprised of the (1) radial collateral ligament; (2) the annular ligament; (3) a variably present accessory LCL; and (4) the LUCL. These structures are further outlined in Fig. 42.7 forming a “Y” configuration with distal attachments on the anterior and posterior aspects of the semilunar notch.
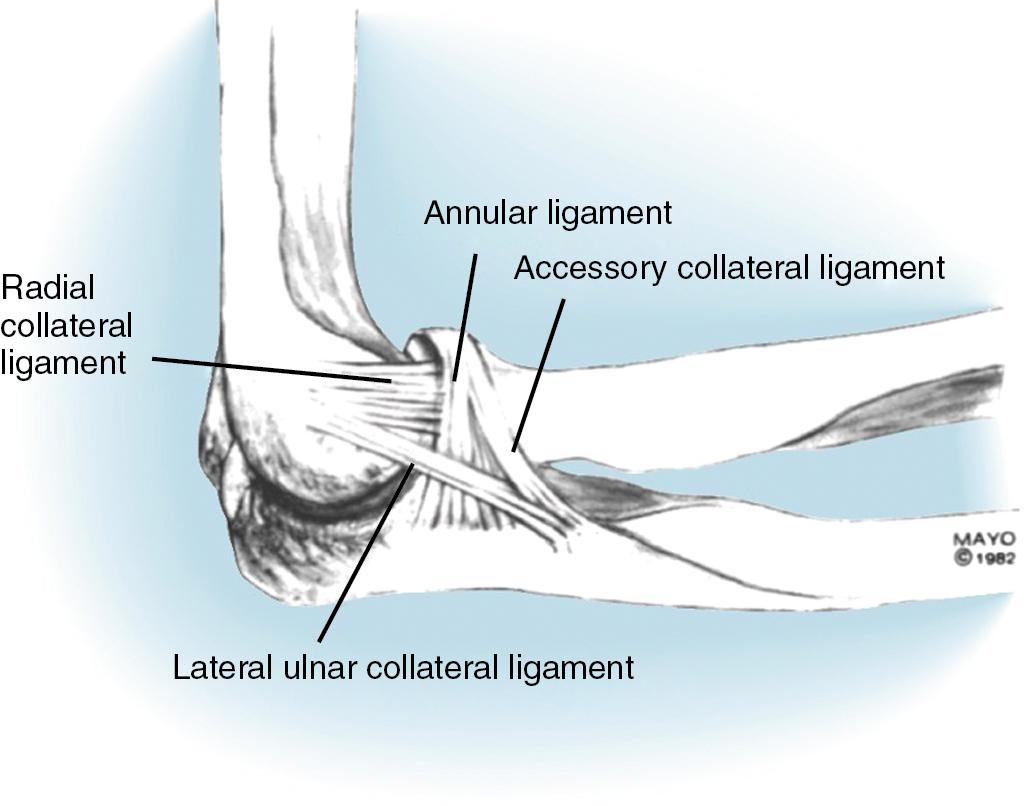
The radial collateral ligament originates from the lateral epicondyle and coalesces with the annular ligament in its attachment to the radial head. The superficial aspect serves as an attachment site for the origin of the supinator muscle. The average length of the radial collateral ligament is 20 mm with an average width of 8 mm. The radial collateral ligament maintains near uniform tension throughout elbow range of motion. The annular ligament is a strong band of tissue that traverse from the anterior and posterior margins of the lesser sigmoid notch circumscribing the radial head and maintaining it contiguous to the proximal ulna. Functionally, the annular ligament becomes taut anteriorly in supination and posteriorly during pronation. The LUCL originates from the lateral epicondyle and blends with the fibers of the annular ligament, arching superficial and distal to insert onto the supinator crest of the ulna. The LUCL functions as the primary varus stabilizer to the ulnohumeral joint and its deficiency is often the prime cause of posterolateral rotatory instability of the elbow.
There are a number of bursae surrounding the elbow with varying clinical relevance. They can be anatomically divided into deep and superficial bursae; the deep bursae are situated between muscles or between muscle and bone and have limited clinical relevance. Whereas superficial bursae included the olecranon and medial and lateral epicondylar bursae can result in clinical pathology.
The most significant deep bursa is the bicipital radial bursa located at the radial tuberosity. It can manifest with inflammation and pain with pronation and supination that may be confused with biceps tendinitis. Clinically, crepitus on pronation and supination suggests tendinopathy whereas fullness or swelling that is accentuated on pronation is more consistent with bicipital radial bursitis. , MRI can aid in this diagnosis with symptomatic treatment entailing rest, ice/heat, and anti-inflammatories. The radiohumeral bursa can be identified deep to the common extensor tendon, below the ECRB and superficial to the radiohumeral joint capsule, this can be involved with exacerbation of lateral epicondylitis.
Medially and laterally, there are subcutaneous epicondylar bursae that are often present although do not commonly result in a clinical pathology. The olecranon bursa is the most common site of superficial bursitis, it typically develops around 7 years of age and its position is between the olecranon process and subcutaneous tissue. The most common etiologies include overuse, direct impact trauma, inflammatory, hemodialysis, or infectious conditions. A logical approach to the management of bursitis involves control of any underlying systemic or inflammatory process followed by conservative management with a resting splint and compression. Second line management in the setting of aseptic bursitis may entail aspiration and injection of a corticosteroid. In this setting it is key that the needle enters the skin in a separate location from the bursa to avoid a continuous soft tissue tract to the skin and prevent chronic drainage. It is important to note the potential for infection and potential subdermal atrophy associated with corticosteroid injection. Chronic bursitis that is refractory to nonoperative measures may merit a surgical treatment. Endoscopic methods of excision have been described with limited long-term data or support. We advocate for an open approach via a longitudinal incision for olecranon bursal excision. If a large olecranon osteophyte is present and may be the inciting factor for the bursitis, this may be obliquely osteotomized via reflection of the triceps. It is of utmost importance to be mindful of freeing the bursa from the skin to avoid devitalizing or button-holing through the skin flap. Upon excision, use of an absorbable suture to secure the skin to the deep structures is vital to eliminate the dead space. A solution of doxycycline can be used to irrigate the wound as a bactericidal agent that will facilitate scar generation and reduce recurrence. A compressive dressing in the early recovery period helps aid wound healing and prevention of fluid accumulation. ,
Muscles crossing the elbow joint control motion of the limb and provide dynamic stability to aid the static stabilizers. This can be further sub-categorized into elbow flexors (biceps, brachialis), elbow extensors (triceps), flexor pronator mass (resist valgus forces), and the mobile wad of three (brachioradialis, extensor carpi radialis longus [ECRL] and ECRB—resist varus forces). The anconeus muscle is thought to have a minor role in elbow extension and as a contributor to varus restraint and posterolateral rotatory stability.
A basic overview of this musculature is covered in this section. The details of exposure, functional examination, and surgical techniques are discussed in the appropriate chapters pertaining to the given structure.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here