Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
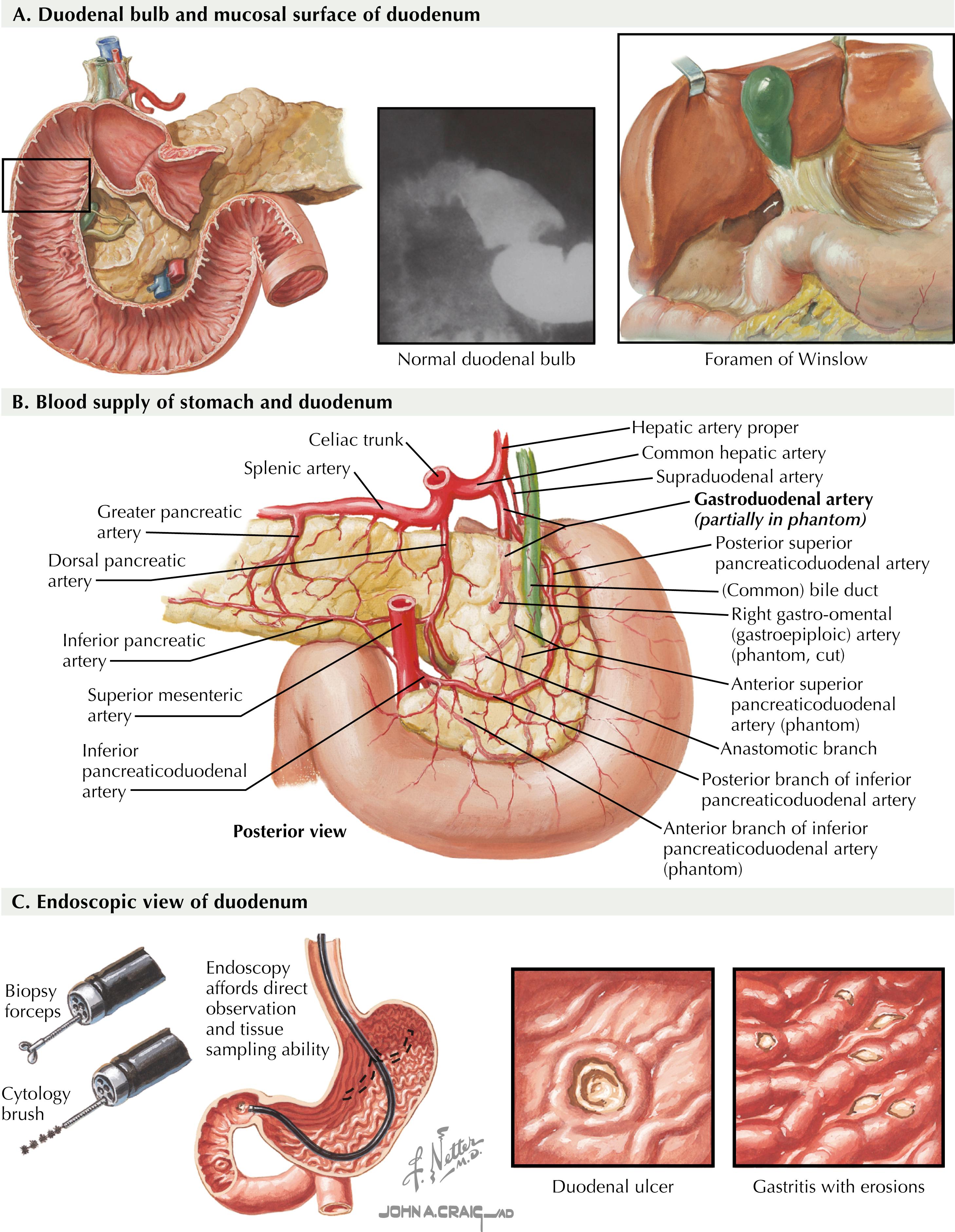
Gastric emptying procedures may play a role in the management of various disease processes, including benign or malignant gastric outlet obstruction, gastroparesis, and pyloric stenosis. Depending on the diagnosis, treatment options may include medical management, enteral or decompressive access tubes, surgical endoscopy, and surgical resection. A thorough understanding of gastric and duodenal anatomy is important when considering endoscopic and surgical gastric emptying procedures ( Fig. 9.1A through C ).
Generally, the treatment for gastric outlet obstruction (GOO) should be managed in the least invasive manner that is appropriate in the context of the disease process. Benign GOO may result from ulcer disease, which may necessitate surgery in medically refractory situations. Malignant GOO may be managed by surgical or endoscopic treatment options based on the individual patient’s needs. Gastroparesis treatment should begin with medical management followed by endoscopic per-oral pyloromyotomy (POP), gastric electric stimulator, laparoscopic pyloroplasty, and, ultimately, gastrectomy if necessary. Pyloric stenosis may also be managed endoscopically or surgically.
Nonsurgical options may be implemented for some forms of gastric outlet obstruction. Although results have been disappointing, botulinum toxin, endoscopic dilation, and stenting have been implemented in the treatment of gastroparesis. Stenting remains a valid treatment option in the management of inoperable gastric outlet obstruction.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here