Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Functional restoration is an intensive and goal-oriented form of interdisciplinary chronic pain management. It was originally developed at the Productive Rehabilitation Institute of Dallas for Ergonomics (PRIDE) to treat individuals with chronic spinal pain (CSP) who are disabled from performing important activities of daily living (ADLs), including work duties. It is now applicable to many forms of chronic pain in addition to CSP, which are injury related or involve the spine as a noninjury “target area” (see Chapter 108 ). The success of this treatment approach in restoring function to disabled individuals depends on several crucial principles common to all credible functional restoration programs, which include the following:
Medical supervision: A functional restoration program has a medical director, or multidisciplinary medical team, providing medical supervision and consultation on related or comorbid medical issues.
Quantitative assessment of physical and psychological function: Objective measurements of physical performance guide the measurement-driven physical training. Physical measurements are aimed at both the painful “weak link” body part(s) and whole-body functioning. A mental health assessment, including a clinical interview and validated self-report questionnaires (graded by severity levels to aid with clinical interpretation), help complete a whole-person functional assessment.
Integrated interdisciplinary treatment team on site: A functional restoration program must have an integrated treatment team whose members are on site, full time, and dedicated entirely to the care of program patients.
Outcome tracking: Because functional restoration is frequently a last option for CSP treatment, outcomes after the program represent the outcome of a full course of surgical and nonoperative therapies performed over an extended period of time. Objective, measurable outcomes (including socioeconomic variables and validated self-report questionnaires) are critical components of functional restoration programs and their quality assurance.
Irrespective of whether the CSP origin is injury related or not and surgically treated or not, virtually all such patients have, to a greater or lesser extent, several crucial pathologies in their multifactorial pain process. These include:
A presumed musculoskeletal degenerative, postinjury or postoperative structural pain generator of a mechanical nature for which interventions and the passage of time have maximized healing beyond further correction or anticipated spontaneous recovery.
A deconditioning syndrome of progressive inactivity resulting from pain (and associated psychological issues), with development of a spinal weak link relative to other uninvolved body parts. Deconditioning involves loss of motion, strength, endurance and coordination, and adversely affects function of adjacent body links.
Development of psychosocial dysfunction (often including mood disorders, insomnia, fear-avoidance, posttraumatic stress, and central sensitization), which is sometimes accompanied by accentuation of premorbid psychiatric conditions.
The frequent well-intentioned but often overdone tendency to overmedicate the pain, creating opioid-dependent “chemical copers,” becoming progressively and comfortably accommodated to dysfunction and disability.
Gradual decrease in commitment to social functions (e.g., work and family role) due to physical and motivational consequences of these factors, further reducing the patient's participation in family and community activities.
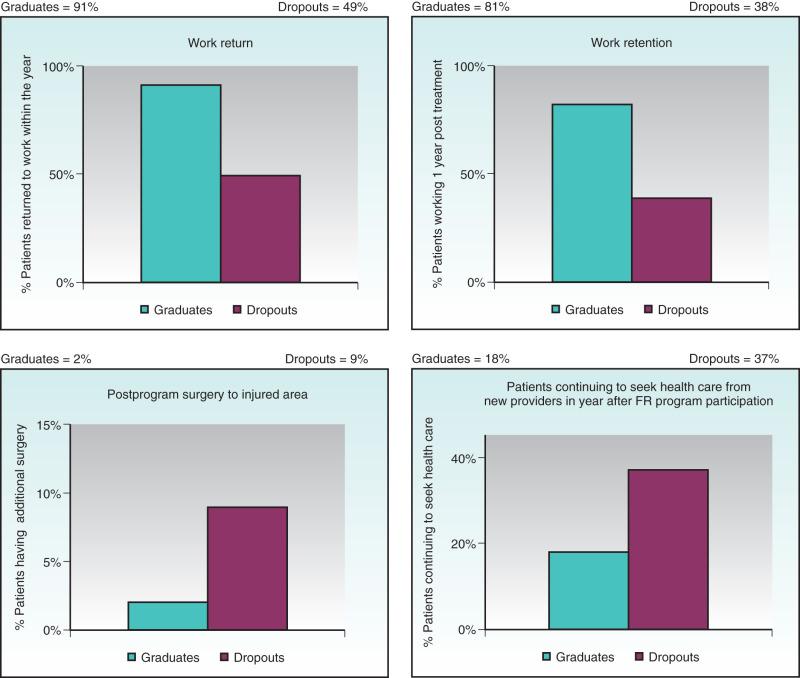
Functional restoration has proven outcomes that comprehensively deal with all of these CSP factors. Box 111.1 lists important components of a functional restoration program. Fig. 111.1 shows four treatment outcome variables, collected 1 year after completion of the PRIDE functional restoration program, over a 10-year span, from 1999 to 2008.
Quantification of physical capacity
Quantification of psychosocial function
Reactivation for restoration of fitness
Measurement-driven reconditioning of the weak link functional unit
Retraining in multiunit functional task performance
Work simulation
Multimodal disability management program
Stress and pain management skills training
Didactic classroom education
Medication management with opioid taper
Vocational/societal reintegration
Formalized outcome tracking
It has been recognized for a long time that minimizing bed rest and maximizing an early return to activity are not harmful and show improved functional outcomes over “restful waiting” in 90% of patients who suffer an acute episode of low back and/or leg pain. Moreover, aggressive, quota-based rehabilitation appears to improve symptoms more rapidly than natural history in placebo-controlled trials. Even without treatment, pain symptoms improve over 90 to 120 days in the majority of patients. Despite medical advances, there is still a paucity of knowledge as to appropriate triage and disposition of the 10% of spinal pain patients who fail all single-provider interventions (including surgery) and absorb 80% to 90% of the money spent on spine care and associated medical issues. Since the 1980s, integrated, interdisciplinary, advanced functional restoration rehabilitation has been recognized as the gold standard of care for treating patients who do not improve with other interventions. This chapter seeks to address the most challenging patients—those who fail to improve within 90 to 180 days with any single-provider modality—and who often receive increasingly aggressive and invasive interventions with unpredictable functional outcomes. Creating a best-practice model for this population is further complicated by the fact that CSP frequently does not correlate with radiologic findings nor do treatment outcomes correlate with radiologic criteria for success.
A phasic nonoperative care model of primary, secondary, and tertiary modes of treatment of spinal disorders has become widely accepted. The concepts underlying this model have been identified in consensus panel documents provided by the North American Spine Society and national treatment guidelines. Each mode brings with it greater expense but commensurately greater functional return in exchange for the increased cost. Briefly outlined, primary care refers to modalities applied during the acute injury phase, intended to modify symptoms during tissue healing. These include—but are not limited to—manual techniques, early single-specialty mobilization, and educational programs. So-called passive modalities may include immobilization after surgery, electrical stimulation, temperature modulation, and traction. Treatment is customarily provided by a single professional, with a limited number of treatments applied to a large number of acute-phase patients who appear clinically and radiologically appropriate.
Secondary care refers to therapy provided to a smaller number of patients not responding to initial symptom-modification treatment. Postacute or postoperative symptoms often require care plans focused on physical reactivation, combining quota-based exercise programs with education. Occasionally, additional passive modalities are employed for symptom modification. The main aim is to prevent late-phase deconditioning that is associated with prolonged inactivity in the transition from functional impairment to disability. In some cases, secondary care may have a degree of programmatic consolidation (e.g., work conditioning or work hardening), particularly toward the end of the postacute period. The lead role in secondary care is usually performed by physical and occupational therapists, with physicians, mental health professionals, social workers, disability managers, and/or chiropractors acting as consultants to ensure progress back to maximal function.
The small percentage of patients who fail to respond to secondary care, or those who fail to benefit from complex surgical procedures, become chronically impaired. These patients often respond positively to a tertiary care environment as the final option to regain lost function. When functional restoration, for one reason or another, is not made available, these patients are frequently consigned to opioids and repeated failed interventions, which are delivered with no strategy for functional recovery. Although tertiary rehabilitation is strongly advocated in national guidelines, physician awareness remains limited, as does the availability of tertiary care. Treatment management guidelines, such as the Official Disability Guidelines ( ODG ) or from the American College of Occupational and Environmental Medicine, identify evidence-based standards that are common to reputable tertiary-care programs. Increasingly, these guidelines, which define minimum standards of assessment and treatment, carry the weight of law in many large states and Canadian provinces. Although tertiary-level treatment is heterogeneous by nature, these guidelines help enforce minimum standards in configuration and outcomes for chronic pain management and functional restoration programs to meet the needs of a diverse population.
As noted previously, the 10% of patients with injuries whose spinal pain becomes chronic accounts for 90% of the cost of health care utilization and disability benefits for this disease category. The more chronic the spinal disorder becomes (the longer time passes after the injury without symptom resolution and return to normal functioning), the more likely that patients will become more severely disabled from normal ADLs. Chronic pain and disability are usually accompanied by psychosocial stress, social withdrawal, depression/anxiety, physical deconditioning, substantial losses (including loss of finances, sleep, and physical functioning), and declining coping skills. A biopsychosocial perspective views chronic pain and associated dysfunction as a complex interaction of biologic, psychological, and social variables, and is an essential concept in the treatment of this myriad of interacting symptoms.
The inability to confront and overcome losses—combined with the downward spiral of pain, disability, and psychosocial distress—may lead CSP patients to overuse opioid medication, benzodiazepines, and other symptom-mediating medications, usually under the direction of a well-meaning physician who sees no other options. This single-modality approach can lead to further physical disuse and withdrawal from ADLs. Until very recently, it has become an increasing feature of the worker's compensation (WC) injury system that insurance carriers intentionally enable and encourage opioid dependence for chronically disabled CSP patients as an alternative to intensive rehabilitation and functional recovery. The carriers have been allowed to “cost shift” financial benefit responsibility to the federal government through Social Security Disability Income (SSDI) and health care to Medicare, while using various legal strategies to declare results of the injury “resolved,” thus negating further responsibility for the state WC system. The more recent focus on the harmful effects of opioid addiction and the loss of worker productivity for a large segment of the working-age population receiving “permanent disability payments” under SSDI has begun a trend of the federal government pushing back, at least initially with Medicare set-asides.
Since Progressive Resistance Exercise programs were developed for the orthopedic rehabilitation of soldiers after World War II, we have learned much about the secondary physical changes accompanying immobilization, disuse, and deconditioning in the spine and extremities. Spontaneous healing or surgical intervention may produce structural recovery of disrupted musculoskeletal tissues in a relatively short 6- to 12-week time period. In cases of severe injury, permanent tissue changes often remain after maximal tissue healing in the form of deformed bony structures or soft tissue instability and scarring. These structural pathologic changes may lead to permanent biomechanical derangements that can produce chronic pain. At its most severe, the structural changes may also include arthrofibrosis, perineural scarring, adhesive joint capsulitis, joint subluxations, and development of sympathetically mediated neuropathic pain syndromes.
One path for the development of CSP in many spinal injury patients is explained by the fear-avoidance model. Fear-avoidance is a nonadaptive style for coping with pain, involving avoidance of ADLs due to fear of increased pain and/or fear of injury/reinjury. There is evidence that elevated fear-avoidance levels during the acute or subacute spinal pain phase can increase the risk that the pain will become chronic. In contrast to spinal pain patients who engage in adaptive behaviors (attempt to “stay positive,” maintain their mobility, and gradually increase their level of daily activities following their injuries), the fear-avoidant patient begins to catastrophize and anticipate increased pain and possible reinjury with increased activity. These dysfunctional thought patterns lead to overprotection of injured body parts, hypervigilance (overmonitoring of physical symptoms), decreased physical activity, decreased social interaction, and increased and exaggerated pain perceptions. Chronically inhibited movement, physical disuse, and avoidance of normal ADLs will inevitably result in physical deconditioning, which is characterized by decreased elasticity of muscles and tendons, decreased range of motion (ROM) of joints, decreased muscle strength, weakness of the cardiovascular system, impairment of normal healing, and somewhat less common neuropathic or central pain phenomena (e.g., complex regional pain syndrome or central sensitization). Fear-avoidance of increased movement and activity is self-reinforcing because attempts to increase activities very often result in pain flare-ups, muscle spasms, or muscle strains, due to the deconditioning syndrome.
The deconditioning syndrome is usually reversible and correctable through training and education in contrast to many of the permanent structural changes referred to previously. Deconditioning involves loss of capsular elasticity, leading to progressive loss of joint motion (and sometimes even to complete rigidity or “frozen” joints). Deconditioning also includes loss of neuromuscular function, leading to muscle fiber atrophy and attendant loses of strength, endurance, recruitment, and coordination. These localized musculoskeletal deficits in the injured, or target weak link, are often accompanied by more generalized aerobic capacity deficits. As the combination of structural and deconditioning pain and physical deficits take hold, inactivity and further deconditioning are accentuated in a vicious cycle of declining physical functioning.
In addition to physical deconditioning, central sensitization can become a contributing factor in chronic spinal pain. Central sensitization is a phenomenon in which neuronal dysregulation in the central nervous system results in hypersensitivity to both noxious and nonnoxious stimuli. It has generally been associated with functional disorders, such as fibromyalgia, but it has become increasingly recognized that central sensitization is a factor for many CSP patients. Evidence suggests that, after a painful spinal injury, a series of events (including hyperalgesia, allodynia, deficiency in descending and/or ascending central modulatory mechanisms, cognitive-emotional sensitization, and sensorimotor conflicts) occur in a subgroup of spinal pain patients, leading to central reorganization that maintains pain in the absence of ongoing peripheral nociception. One longitudinal study found that spinal pain patients are more likely to develop widespread pain as regional spinal pain becomes more chronic. Two separate studies conducted in functional restoration treatment populations found that 32% of CSP patients also met the American College of Rheumatology diagnostic criteria for chronic widespread pain, and 23% of chronic musculoskeletal pain disorder patients met criteria for comorbid fibromyalgia. Patients with central sensitization often develop central sensitivity syndromes (CSSs), with a long list of associated maladies that often result in disability and/or opioid dependence. These CSSs include fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, migraine headaches, myofascial pain, and others. The high likelihood of fear-avoidance and opioid dependence with these patients makes them excellent candidates for functional restoration.
Physical deconditioning, high pain sensitivity, psychosocial distress, and social withdrawal inevitably result in a high prevalence of psychopathology in many CSP patients. Rates of both premorbid and postinjury psychiatric illness in the CSP population (e.g., major depression, substance abuse, anxiety disorders, personality disorders, childhood trauma) are much higher than for the US population in general. An especially strong relationship has been found between chronic pain and major depressive disorder, in which comorbidity may reach over 50% as compared to US population estimates of 5% to 17%. Furthermore, psychiatric symptoms (especially anxiety and substance disorders) have been found to precede the spinal injury for many CSP patients. In addition to psychiatric diagnoses, patient-reported symptoms of depression, anxiety, sleep disturbance, and perceived disability tend to be highly elevated for the average patient who enters functional restoration.
With all of these factors leading to partial or total disability from work, recreation, or the family role, it is not at all surprising that many different groups of CSP patients are eligible for a functional restoration program. By its nature, it is especially suitable for work-related injuries, WC cases, or other types of compensation injuries (long-term disability, Social Security Disability, motor vehicle accidents). Patients who have become totally disabled from work by CSP are the most obvious candidates for functional restoration and are usually discovered and referred first. Delay in pursing surgical intervention or multiple surgeries sometimes leads to significant worsening of CSP by increasing the longevity of chronicity of disability, and these patients may present for treatment late. In today's competitive workplace and WC state systems, injured workers may be returned to duty prematurely and may have difficulty moving from part-time or light-duty work back to performing full-duty materials handling or positional requirements.
In addition to WC cases, functional restoration can be equally effective for treating patients with chronic pain and disability related to noncompensable injuries or pain of insidious onset. In countries such as Sweden, where access to the best health care does not require an injury, the majority of CSP symptoms are reported by patients to begin insidiously rather than with a reported “incident or injury.” In the United States, while a majority of patients report that their symptoms started from an “injury,” a large subset of chronic pain patients begins insidiously and may be associated with various psychiatric or other comorbid conditions, often characterized by central sensitization and/or opioid dependence. Many patients with CSP from an insidious origin develop their disability slowly over years. Some patients develop spinal deconditioning through enforced disuse from other medical or nonmedical situations; these patients may develop disability due as much to the deconditioning as to the primary disease or other process that originally led to the inactivity. Once partial or total disability associated with a CSP disorder has developed, such patients are excellent candidates for functional restoration ( Box 111.2 ).
Worker's compensation injuries developing chronic partial/total disability
Postoperative patients with long periods of disability and disuse due to prolonged surgical recovery
Patients developing neuropathic or sympathetically mediated regional pain or radiculopathy disorders
Central sensitization with a spinal target area
Central sensitivity syndromes (e.g., fibromyalgia)
Patients becoming deconditioned through fear-avoidance
Patients developing disability primarily due to opioid dependence
Patients enabled to disability by cost shifting to federal financial and health benefits
The interaction of fear-avoidance of ADLs, social withdrawal, physical deconditioning, high pain sensitivity, opioid overuse, psychosocial distress, and psychopathology is complex. If all of these biopsychosocial factors are not addressed effectively, the treatment is likely to fail. When addressing these interacting factors, it is important to understand that many chronic spinal patients have lost hope and self-esteem. It is not simply a matter of prescribing an antidepressant and putting them into physical therapy (PT). Treatment success requires sustained encouragement and education from the treatment team to guide patients through the therapeutic process, which helps them “see the light at the end of the tunnel” and recognize that they have a chance for a more positive future and the ability to function successfully with normal ADLs, including sustained employment.
In a functional restoration program, a team of professionals works together with each patient toward a common goal of increasing physical and psychosocial functioning. Team members provide services within their individual disciplines to address the physical and psychosocial barriers that are preventing patients from reaching their full functional potential. In contrast to multidisciplinary treatment, in which all team members may or may not provide services in the same clinic and may or may not communicate regularly, all interdisciplinary team members in a functional restoration program provide treatment in the same facility. They communicate on a daily basis, both formally (in case conference meetings) and informally, and are always available to address patient needs as they arise. The functional restoration treatment team includes a supervising medical director, nursing staff, physical and occupational therapists, mental health professionals, and rehabilitation counselors (case managers).
The supervising medical director or multidisciplinary medical team helps to guide the rehabilitation program and treatment team. The physician must have a general background in sports medicine, musculoskeletal injury, psychoactive medications, disability management, and rehabilitation supervision. The medical director is usually assisted by a nurse “physician extender” or practitioner who must be able to educate patients on medical matters, triage musculoskeletal problems, provide medication control, and communicate with outside agencies about medical issues as they arise.
Both the physical and occupational therapists guide patients through mobility, strength, endurance, coordination, and core stability exercises while providing patient education on active pain management strategies. They supervise group stretch classes and gyms on a daily basis and work individually with patients as needed. The physical and occupational therapists may also have a team of exercise technicians who help monitor and guide patients through individual and group exercises. Physical therapists are responsible for ROM and strength assessments, and they supervise most of the progressive resistive exercises for individual joints or targeted weak link spine areas. Occupational therapists work more with whole-body functional activity simulation to help individuals overcome physical obstacles that are limiting productivity at work and home. They are also primarily responsible for functional capacity examinations at program admission and discharge. At the original PRIDE functional restoration program, the functional capacity evaluation (FCE), isokinetic testing, and other functional measurements are compared to a normative database (based on age, gender, and body mass index) to discover an initial tolerable training level in measurement-driven training. This is applied in the PT gym, where regional spinal or extremity weak links are trained, and in the occupational therapy (OT) gyms, where whole-person materials handling or positional requirements are trained. A computerized 75-step progressive resistance training program is also individualized to the patient population to ensure slow but steady recovery of function.
Mental health professionals are a vital component of functional restoration and can come from a variety of similar disciplines, including psychology, counseling, social work, and marriage and family therapy. They can provide a variety of services, including mental health assessments, supportive psychotherapy, psycho-education, and cognitive- behavioral therapy. They must address psychosocial factors, which can impede physical progress and return to optimal functioning.
Rehabilitation counselors/case managers oversee each patient's case. They must be knowledgeable about insurance coverage rules and federal and state WC guidelines. They communicate with payer sources and employers, provide vocational assessments and counseling, and facilitate referrals to state agencies for vocational assistance as needed. The case managers often function as team leaders within the program to identify the minority of patients who are progressing slowly (or not at all), highlighting the socioeconomic secondary gain issues that may be causing nonorganic illness behaviors, and setting up patient and family conferences to deal with crucial issues such as nonattendance, failures of cooperation and compliance, and patient frustration. They work closest with the supervising physician on behavioral issues during the program and provide documentation at the conclusion of the program on functional limitations, work return capabilities, and job plans. The case managers also supervise the outcome tracking process.
All team members must be involved from the outset in the initial assessment and quantification of barriers to the patient's recovery. This effort should be led by a medical director or physician member of the team, who, along with the nursing staff, performs an outpatient medical examination to review history, physical findings, and relevant radiologic or other diagnostic data. The intent of this visit is fourfold. First, the physician should look for medical barriers that were overlooked during previous evaluations and ensure that existing tissue damage is unlikely to improve with additional surgical intervention or activity limitation. Second, the physician should assess the degree to which psychosocial distress is causing other physiologic barriers such as insomnia, mood disorder, fear-avoidance, central sensitization, or inorganic signs that will undermine the success of the individual patient. Third, the physician should identify and document the patient's desired outcome from this intervention. Finally, a physician should make every attempt to establish a therapeutic relationship and provide education to overcome resistance to treatment. As the team leader, the physician should take care to avoid a confrontation at this meeting (this is occasionally the desired secondary gain outcome of some patients) by reassuring patients that they have a choice and that the shared outcome of this visit is that patients give the program a chance. Often, this is achieved by empowering patients to evaluate the program at the same time the program is evaluating them. Simultaneously, the physician should take note of specific declared goals of the patient and pass these along to the evaluating team to ensure early bonding through shared understanding that team members are aware of and supportive of the patient's functional goals. Additionally, this is the first opportunity for the physician and nursing staff to help clarify and guide the patient's treatment expectations, to make it plain that the primary outcome of the program is functional return, and to introduce the concept that disability is a choice.
A potentially useful component of the initial evaluation is the physician's proposal of the Surgical Option Process (SOP). It comes into play if there is uncertainty or disagreement about whether a surgical option is likely to enhance recovery. In many cases, such uncertainty may bring the medical care sequence to a grinding halt related to this indecision. The SOP has recently been presented as an effective method of overcoming this recovery barrier. The patient who enters functional restoration with a surgical option agrees to participate in the first 50% of the program. At that point, an SOP determination meeting with the physician allows the patient to select the option to either pursue or decline surgery. If the patient decides to pursue surgery, the program is placed on medical hold while the patient pursues renewed surgical consultation and a pathway to a fresh determination of whether surgery is likely to be beneficial in the face of the patient's personal assessment that it is needed. Those who decline surgery simply complete the program. In a pilot and subsequent larger study, outcomes of the SOP have proven very promising. In 70% of patients who elected to decline surgery, almost all (99%) continued to avoid surgical intervention over the postprogram year. Of the 30% who decided to pursue surgery, about half ended up receiving it, while the other half did not. Most of the patients failing to receive surgery after electing to pursue it were denied based on the determination by their surgeon or consultant (and rarely by a patient or an insurance carrier denial). Using the SOP model, delays in treatment that lead to further physical and psychosocial declines are avoided by the application of a decisive methodology.
If the patient is deemed appropriate for nonsurgical treatment, the physician should first initiate an interdisciplinary evaluation and then follow up with the patient in a second physician visit to go over the results. The results of this interdisciplinary evaluation determine whether a full or abbreviated functional restoration program will be requested. Lesser levels of care might still be feasible for patients who are working, have very limited disability, or have minimal psychosocial barriers and who have relatively high physical ability. Individual therapies, or work conditioning/hardening–equivalent treatments are available for those not requiring a full tertiary functional restoration program.
The functional restoration interdisciplinary team is in charge of the two-component evaluation. First, the Physical Department performs PT and OT individual assessments, followed by an FCE. The details of the FCE are discussed later in this chapter. Second, the Disability Management Team, consisting of mental health professionals and case managers, performs two critical interviews. The first is a formal mental health evaluation, while the second explores social and economic factors associated with the patient's disability, leading to identification of barriers to recovery and a plan to meet treatment goals. These components of preparing for a multimodal disability management process are also discussed later in the chapter. The results of this evaluation are shared with the patient at the second physician visit and are presented to referring physicians and payers during the treatment preauthorization process.
The physician team leader takes the quantitative evaluations and initiates a frank discussion with the patient on the basis of firm data. It is hoped that the patient has bonded with one or more of the staff members in the course of the assessment process and has been impressed with the thorough assessment and milieu of function at the facility. If the patient agrees to proceed, the physician plans the length of the program on the basis of achieving maximum function. Instead of making patients “good as new,” the team tries to focus patients on functional goals and manage their expectations toward reaching a functional plateau—possessing the physical strength and endurance to remain at a job and the psychological tools to control pain and cope with daily stressors. It is hoped that this important meeting will readjust patient expectations to internalize the concept of continued recovery after the program—keeping the patient focused on getting “good enough” rather than perfect. On the basis of objective data from the initial interdisciplinary assessment rather than simply relying on subjective pain reports, patients have set their own speedometer for the length and intensity of the treatment program. With the patient's agreement to participate in treatment, a comprehensive medication management strategy is also discussed with the patient. This strategy involves the use of medications specifically related to the findings of the initial evaluation to help control the identified problems (e.g., pain, inflammation, mood disorder, insomnia, neuropathic factors, cognitive issues, and/or central sensitization). It is important that patients understand that new medications and dosages may be prescribed at this point with the intention of reducing medication as pain recovery and functional improvement progress. Finally, the patient's agreement to enter the program is a tacit agreement to pursue functional posttreatment goals that are primarily vocational and societal but may also include familial and educational enrichment.
It is a reality of current medical practice that almost every insurance system now requires preauthorization for complex treatments; functional restoration interdisciplinary programs are no exception. Over the past decade, this process has been streamlined to some degree by the acceptance of national guidelines that have been previously discussed. Most state and federal worker's compensation carriers now have a preauthorization process, often delegated to a semi-independent vendor and guided by some type of state or federal rules. The peer review process involves submission of data for determination of authorization, usually overseen by a semi-independent physician evaluation, and often permitting a telephonic peer call between the requesting facility staff and peer reviewer. There is usually a single reconsideration appeal process inherent in the system. Whatever the methodology, the results of the physician assessment and interdisciplinary evaluation become integral to the approval or denial of the program within these systems. At this writing, such a formal preauthorization process is not generally part of group health coverage and the rules regarding interdisciplinary pain management are heterogeneous and arcane. There is also a large variation between what is permitted in hospital and outpatient settings. It is anticipated that the consolidation of national health care system reforms will ultimately create some standardization and clarity, but right now the ability of patients outside the WC system to participate in such programs may be limited in scope by financial barriers. In some states, state vocational rehabilitation agencies may provide some supplementation to medical insurance to assist patient rehabilitation for vocational recovery and preparation for retraining or work placement options.
For spine surgeons, the main principle to understand in tertiary level, interdisciplinary, functional restoration is that the usual way we assess activity tolerance (i.e., by endurance and pain) is, in this self-selected population, unreliable and counterproductive to functional return. As such, validated, reproducible quantitative measures of physical dysfunction must be employed to track functional gains. The FCE has become a popular term that denotes a variable set of methods and tests. Different methodologies for performing FCEs exist. They often lack specificity, physics-based principles of accuracy and precision, and comparisons to normative databases. Functional restoration requires true quantification of function because the absence of numeric data leaves physically inhibited patients and their care team enslaved by the cliché, “If it hurts too much, don't do it.” An understanding of the principles of accuracy, precision, and sources of error is necessary when performing a quality FCE and interpreting the results. In the PRIDE model of functional restoration, physical capacity assessment implies the assessment of the injured musculoskeletal spinal region, generally involving quantification through reproducibility of mobility, strength, and endurance of a given functional unit or around a given joint. On the other hand, the term functional capacity assessment implies measurement of whole-person performance—taking compensatory strategies into account in tasks that are specifically designed to stress the injured body parts (e.g., materials handling capability for lifting, carrying, or pulling, as well as tolerance of positions and activities such as sitting, standing, walking, and climbing). Research has focused on responsiveness of prerehabilitation functional measurements with retesting at the end of the program and comparison to specific normative databases. Aided by a new generation of quantitative tools and an evidence-based consensus on techniques for FCEs, a reproducible prognostic FCE is now possible, even for difficult chronic pain patients. This innovation permits an individual patient's comparison with both normative data and an absolute job requirement for materials handling and positional tolerances.
Trunk motion is a compound movement combining intersegmental spine and hip motion components. A patient with a completely fused spine, but very loose hamstrings, can often bend forward to perform toe touches using hip motion alone. Although it is difficult to measure intersegmental motion nonradiologically, inclinometers may be used to separate the hip motion component from the lumbar spine motion component and derive valuable information. The basic information on inclinometry originally came from British rheumatology, and the system has been used, in one form or another, in Europe for over 50 years. As with all physical capacity measures, ROM information is only useful when compared with a normative database and contextualized by an identifiable effort factor. For lumbar ROM, the effort factor is the comparison between the hip motion component and the spine straight-leg raise test measurement.
Contrary to the belief of many clinicians, a surprising amount of information can be obtained from visual observation of sagittal and coronal lumbopelvic motion. In subjects with normal spine and hips, forward bending occurs in a sequence (easier to recognize with the observer's hands on the top of the pelvis) in which the lumbar spine flexion occurs early and faster than the hip motion component. This represents an inborn physiologic strategy, recognizable by all familiar with “stoop labor,” in which the spine “hangs on the ligaments” and then descends further through the action of the more powerful gluteal musculature around a hip access. When this pattern is interrupted in a patient population, it usually represents motion limited by pain or fear, but may also point to unrecognized segmental rigidity, spasm, or efforts to deceive the examiner. Segmental rigidity is an especially important finding. It is assessed through observation of coronal movement, which is often a source of pain, and is potentially correctable by exercise alone or the combination of exercise and facet injections at the rigid levels.
Several devices are commercially available for assessing isometric, isotonic, or isokinetic trunk strength in various planes of motion. Most involve some type of pelvic stabilization, with application of force through a line projecting between the sternum and scapulae, thus representing trunk strength as torque (torsional force) around a pelvic fulcrum with a lever arm individualized to a subject's height. Cervical dynamic strength measurement devices have been seen in prototype form but are not currently available, leaving isometrics as the only cervical alternative. Isokinetic devices stabilize the variables of acceleration and velocity in order to provide torque as the primary independent variable. Isokinetic testing narrows the Gaussian distribution of values by limiting the number of independent variables, which, in our opinion, provides a more valid test. Isometric test models employing strain gauges have been used for more than 60 years. Though commercially available, dynamic isokinetic trunk strength testing has only been available since 1985. There is abundant literature demonstrating efficacy in identifying isolated motion-segment dysfunction (differentiating weakness and/or decreased endurance) and quantifying outcome improvements. Only a few commercially available isometric or isokinetic devices still exist. PRIDE currently uses a dynamometer connected to a sagittal semi-seated torso testing device ( Figs. 111.2 to 111.4 ).

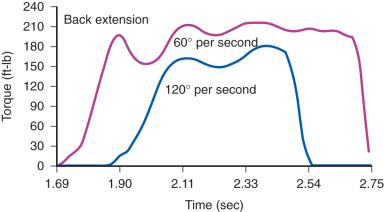
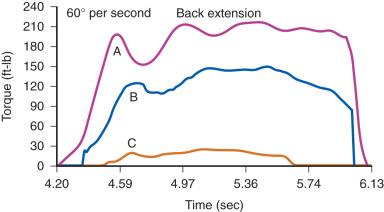
Isolated trunk strength results from normal subjects have been compared with CSP patients with and without prior surgery. Substantial differences have been shown between these groups, initially with incremental trunk strength improvement demonstrated during rehabilitation of chronically disabled spine pain patients (see Figs. 111.3 and 111.4 ). The intent of all of the devices is to isolate and challenge the trunk strength component of the thoracolumbar functional unit by stabilizing above and below the area to be tested. The isolation of the vulnerable weak link portion of the vertebral biomechanical chain, linking the shoulder girdle to the pelvis, is intended to assess muscle strength and endurance just as measuring quadriceps and hamstrings is of prima facie importance to knee function. For any of the devices to be useful, the dynamometer must give accurate and reproducible measurements and the testing protocol must conform exactly to the one that was employed when the normative database was created. The normative database can then be used to express the individual's results as a percent of normal.
The inactivity that leads to deconditioning and a regional spinal motion/strength weak link in patients with CSP also reduces cardiovascular fitness, creating a feed-forward effect on decreasing weak-link endurance and overall functional tolerance. Treadmill, bicycle, and upper body ergometry have long been used to measure the cardiovascular response to a measured workload. Significant deficits in aerobic capacity are frequently present in chronic and postoperative CSP patients. These deficits are somewhat proportional to the duration of disability and the degree of inactivity. Because inactivity may also produce deconditioning of arms and legs, the patient may quit the ergometry test due to limb fatigue rather than reduced cardiovascular fitness. However, these alternative scenarios can usually be distinguished either by interval monitoring of the heart rate delta achieved at the point of voluntary test termination or by comparing the upper and lower body ergometric results. In most deconditioned patients who are exerting full effort, an exaggerated heart rate response to relatively low workloads is customarily the limiting factor of the test. Such testing leads to a determination of the extent to which aerobic capacity training and/or lower and upper extremity strength training need to be added to the functional restoration program.
The whole-body task performance assessment, usually the province of the occupational therapist, requires a skilled eye and a highly burnished insight. Whereas quantification of the isolated lumbar region has multiple internal checks, the whole-body materials handling performance component effort is subject to interference by a number of psycho-socioeconomic factors. A patient may demonstrate limited ability to lift, carry, push, or pull due to weakness, fear-avoidance, or chronic fatigue but may also avoid performing well on these tasks because of perceived financial secondary gain. Physically, whole-body performance problems may be entirely due to the injured lumbar spine or may have to do with comorbid problems in the arms, upper back, or legs. Detecting the reason for suboptimal whole-body performance can sometimes be difficult. The whole-body performance assessment is divided into two major subsections that can be classified as materials handling and positional tolerance. These functional requirements can be compared to job descriptions, household tasks, or recreational demands to determine specific functional capabilities.
Lifting capacity has long been the gold standard for spine-related, materials-handling functional capacity. It is still the measurement of greatest concern to those medical and nonmedical personnel who judge the patient's work capacity or vocational suitability. The isometric lift task employed in the National Institute of Occupational Safety and Health guidelines is still in wide use and has a large comparative database, though it does not quite rectify the inherent lack of generalizability of isometric measurements. To give the full picture of any materials-handling task, several measures—including isometric, isokinetic, and isoinertial —may be combined. All whole-person tests are standardized to provide interpretable, quantifiable information to assess the proximity to job-specific task performance, keeping the patient accountable to a specific outcome of choice. Within the domain of whole-body task performance, the subdomains of materials handling (e.g., floor-to-waist lifting, waist-to-shoulder lifting, carrying, pushing, pulling) and positional tolerance (e.g., sitting, standing, balance, stair/ladder climbing, reaching, squatting, walking, kneeling, or reaching) each have to be assessed and collated. Repeated longitudinal testing adds validity to programmatic compliance and credibility to the physician's attestation of task-specific suitability to the prospective employer. In addition, longitudinal studies, demonstrating sufficiently large differences in prerehabilitation and postrehabilitation performance measures, are an effective demonstration of the program's relevance and validity.
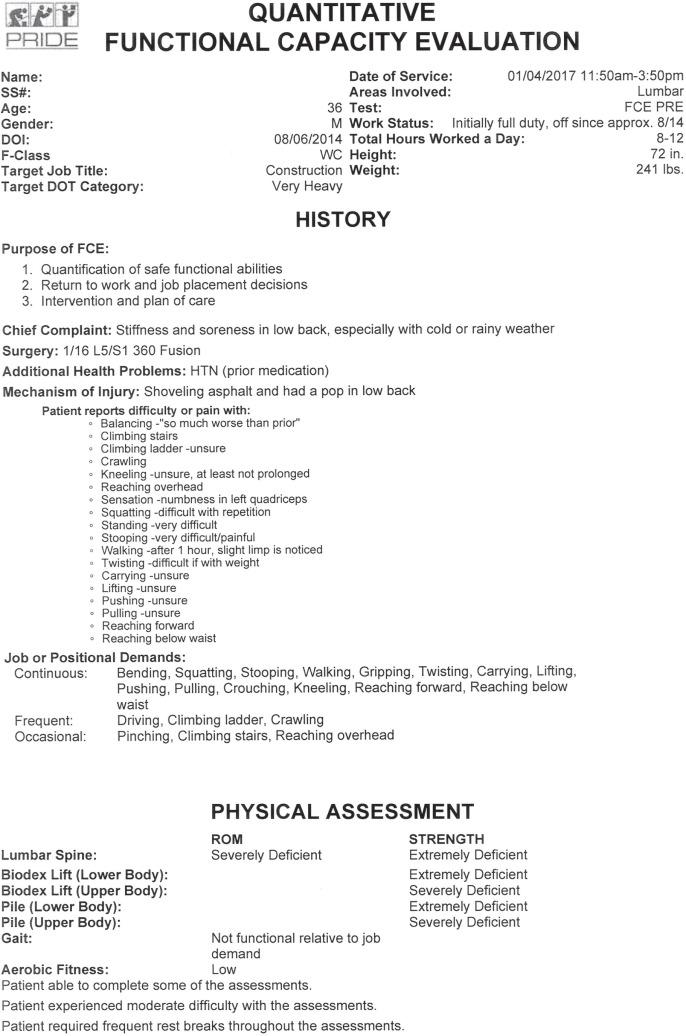
A quantitative FCE has been developed for use in the PRIDE program. Examples of pre- and postrehabilitation FCE reports are provided in Figs. 111.5A and 111.5B , respectively. The patient entered the treatment program with 28 months of injury-related total disability and 12 months following L5–S1 fusion. His job of injury, in construction, required a very heavy physical demand level. He was terminated from his job of injury while in treatment and chose a target job goal of construction project manager. As can be seen in Fig. 111.5A , the patient tested at a below sedentary level in the initial FCE, in large part due to his inability to do any floor-to-waist lifting. Chronic pain patients are frequently so physically inhibited by their psychosocial comorbidities that “0” scores on one or more tests are not uncommon at the initial FCE. The extreme deficits of trunk strength that he demonstrated in the Biodex lift test and the Progressive Isoinertial Lifting Evaluation indicated that he was unable to develop torque, which was likely due, at least in part, to pain inhibition. After completing the functional restoration program, however, his physical demand level had increased to heavy, which met the demands of his target job (see Fig. 111.5B ). The principles underpinning an FCE in a chronic pain population are discussed in an American Medical Association book on FCEs by Galper and colleagues.
In summary, quantification of physical function is a relatively new, important, but still underused tool in assessing patients with CSP. Quantification of physical functional capacity requires patient motivation, but because an effort factor can be identified by a skilled therapist with each physical capacity test, suboptimal effort can be recognized and used to evaluate and address patient fear-avoidance beliefs, hyperalgesia, or motivational barrier.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here