Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Dissection of the frontal recess is the most difficult of the basic endoscopic dissections.
Care must be taken to preserve the mucosa surrounding the frontal recess. Stripping of mucosa can result in postoperative stenosis and neo-osteogenesis.
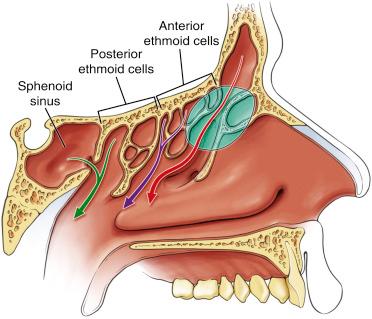
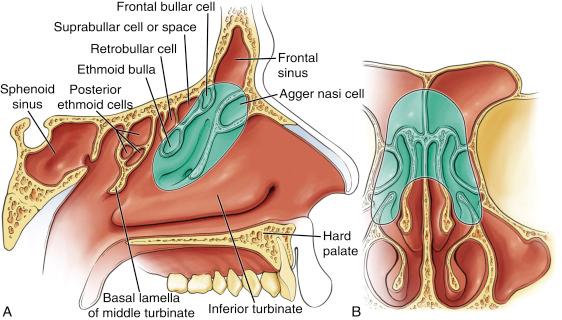
The frontal recess is difficult for another reason: the variable anatomy that can present an obstruction within the frontal recess. Frontal recess cells, posteriorly located frontal bullar cells, and intersinus septal cells all vary in presence and location from patient to patient but must be dissected for a complete frontal recess dissection ( Fig. 9.1 ).
Although a frontal recess dissection can be performed without removing the ethmoid bulla, a more complete and thorough surgery is possible only after the skull base has been cleared of all superior ethmoid bony partitions.
When performed as part of complete functional endoscopic sinus surgery, the frontal recess dissection follows the completion of the maxillary antrostomy, sphenoidotomy, and complete ethmoidectomy.
Proper postoperative care and débridements are critical for long-term patency of the frontal recess.
Other keys to success are the following:
Proper instrumentation
Use of angled through-cutting instruments and probes specially designed for the frontal recess
Good visualization with a minimum of a 45-degree and preferably a 70-degree endoscope
Maintenance of a well-mucosalized frontal recess
Endoscopic frontal procedures can be described by the following classification, based on Wolfgang Draf’s initial work in 1991 using the microscope for endonasal frontal recess dissections:
Draf I: Removal of the superior uncinate with preservation of the agger nasi ( Fig. 9.2 )
Draf IIa: Removal of all cells within the frontal recess ( Fig. 9.3 )
Draf IIb: Draf IIa dissection plus removal of the ipsilateral floor of the frontal recess ( Fig. 9.4 )
Draf III: Bilateral Draf IIb dissection plus removal of the intersinus septum and the superior nasal septum to create a single common opening ( Fig. 9.5 )
Nearly all primary cases and a substantial number of revision cases can be adequately treated using a Draf IIa procedure. This chapter discusses the technique for a Draf IIa dissection; the following chapters are devoted to the Draf IIb and Draf III procedures.
The anatomic shape of the frontal sinus and frontal recess can be visualized as an hourglass, with the narrowest point corresponding to the frontal sinus ostium.
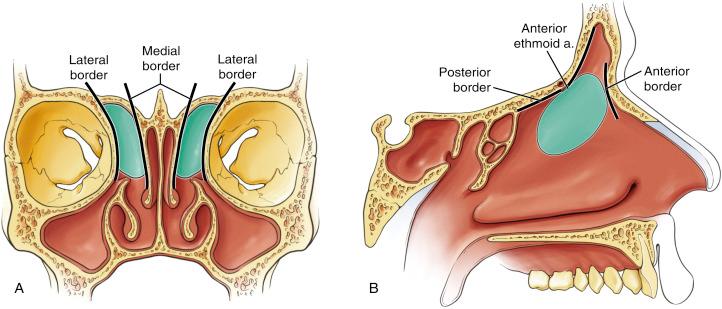
For the purpose of dissection, the frontal recess can be thought of as a box with four borders ( Fig. 9.6 ). Enlarging the recess requires dissection of each wall of the box:
Anterior: the superior uncinate process and agger nasi cell
Medial: the lateral lamellae of the skull base and intersinus septum, and the attachment of the middle turbinate
Posterior: the supraorbital ethmoid cell and the anterior border of the ethmoid bulla
Lateral: the medial wall of the orbit
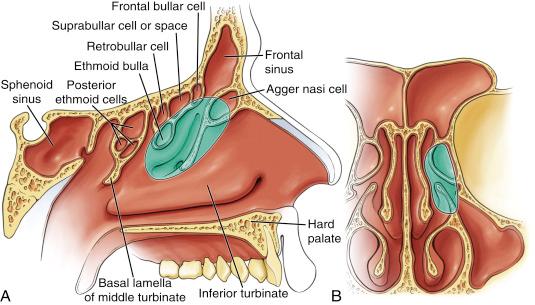
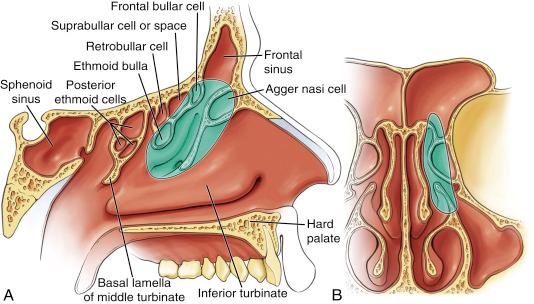
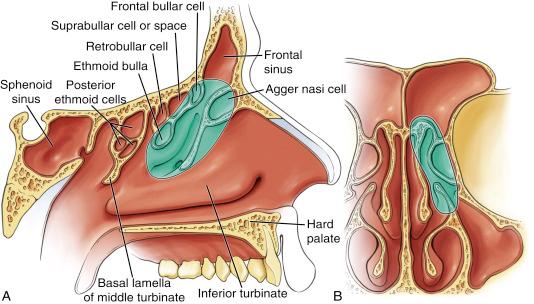
The most anterior of the ethmoid air cells, the agger nasi cell often has the appearance of a bulge in the superior uncinate process. The cap of the agger nasi cell often makes the floor of the frontal recess ( Fig. 9.7A ).
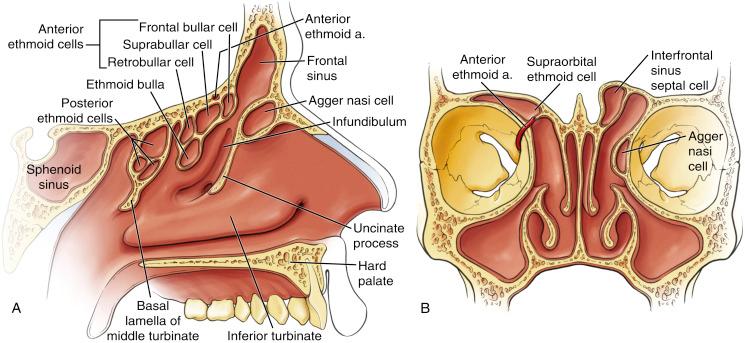
An interfrontal sinus septal cell is a cell that arises along the midline septum of the frontal sinus. As it pneumatizes, it narrows the frontal recess from medial to lateral (see Fig. 9.7B ).
A supraorbital ethmoid cell pneumatizes into the frontal bone over the orbit and behind the frontal recess. It may extend lateral to the frontal recess (see Fig. 9.7B ).
A suprabullar cell arises above the ethmoid bulla and pneumatizes up to the attachment of the bulla to the skull base. It is best seen in sagittal view (see Fig. 9.7A ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here