Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The armamentarium available to both the plastic surgeon and breast reconstruction patient has continued to expand with improvement of techniques and the actual number of flaps and implant alternatives available. The transverse upper gracilis (TUG) flap provides just such an alternative. Although the deep inferior epigastric perforator (DIEP) flap is often the first choice for autologous breast reconstruction, not all patients are good candidates. Patients may lack abdominal tissue, have had previous abdominal surgery or desire to have excess tissue removed from a different donor area. Non-abdominal donor sites such as the superior gluteal artery perforator (SGAP), inferior gluteal artery perforator (IGAP), TUG and profunda artery perforator (PAP) can be considered. Each has unique characteristics and strengths that can be used to advantage, however drawbacks are not inconsequential for the SGAP, IGAP and PAP. Another free flap alternative, the TUG flap, provides an excellent breast reconstruction method in the appropriate patient. Among its many benefits, it has a reliable and straightforward pedicle dissection, good projection and an inconspicuous donor scar.
While some donor tissues can have tedious dissection, the TUG is based on the anatomy of the gracilis muscle and the surgical dissection and blood supply are consistent. The gracilis muscle is entirely expendable, and there are no significant functional changes with loss of the gracilis. And, unlike abdominal donor tissue, bulging or hernia formation are not a factor in TUG harvest.
While DIEP and superficial inferior epigastric artery (SIEA) flaps offer an aesthetic perk, i.e. they are similar to an abdominoplasty, the TUG donor area is based on the excess thigh tissue, fat or skin as it is designed for a medial thigh lift. This side benefit can nudge the patient and surgeon toward selection of this flap over others depending on patient body habitus.
The TUG flap can be used in both immediate and delayed reconstruction, with or without a skin paddle, and can be combined with later implant augmentation or fat grafting to increase size. In patients without a large amount of subcutaneous tissue, the potential for fat grafting or implant augmentation expands the indications of the flap. In addition, two TUG flaps can be stacked to enhance flap volume. Although flap stacking is more technically challenging, this can be an option in unilateral reconstruction patients who do not wish to have later augmentation or fat grafting.
All patients without inner thigh trauma or scarring are potential candidates for TUG flap reconstruction, providing they are free flap candidates. The flap is most commonly indicated in patients with insufficient abdominal tissue or prior abdominal surgery, such as abdominoplasty, liposuction or a failed abdominal flap. Patient preference is often an indication as well. It is not uncommon for patients to wish to avoid abdominal scars. Patients with small and moderate-sized breasts can be good candidates, with the typical patient being pear shaped, with excess medial thigh tissue, and in need of an A to B size cup ( Fig. 7.1 ).

The TUG can be used in both immediate and delayed reconstruction of post-mastectomy deformity. If a free flap is being considered for a partial mastectomy irregularity, the TUG is an alternative. Patients with failed implants, chronic breast wounds or osteoradionecrosis can be considered as well. The placement of the gracilis muscle directly on any areas of osteoradionecrosis can be advantageous.
Like any microsurgical patient, the general health of the candidate should be considered. Advanced age, poor nutrition or underlying comorbidities can make this flap a poor choice. Peripheral vascular disease and possible gracilis pedicle disease can make the artery to the flap calcified. Morbidly obese patients are not good candidates. Because the patient is usually placed in the lithotomy position for flap harvest, positioning the morbidly obese patient may be impossible.
Absolute contraindications are a history of hypercoagulable disorder or bleeding diathesis that cannot be addressed with medical intervention. Previous inner thigh surgery that infringes on the vascular pedicle, perforators or flap design should be a warning to avoid this flap. Caution should be used in the patient with saphenous vein stripping. If a secondary vein is needed for accessory venous outflow (say, a poor internal mammary vessel), the surgeon may want to have the saphenous cutaneous vein available for microsurgical coaptation. The posterior branch of the saphenous vein can be a good second draining vein, similar to the superficial inferior epigastric vein in the DIEP flap. Any history of knee or hip arthritis or arthroplasty could be problematic. The patient should be able to have the hip flexed and knee flexed during the harvest of the flap, which is most commonly performed in the lithotomy position. Lack of joint flexibility can make intraoperative positioning difficult.
The evaluation of the TUG patient follows that of any microsurgical patient: a full history and complete exam are mandatory. Attention is paid to any history of lower extremity issues or lower limb surgery. Medial thigh contour, fat distribution and any excess skin are assessed with the patient in the upright position. The upper medial thigh tissue is evaluated with a pinch test, examining both the laxity of the tissue and the amount of subcutaneous fat. Because the flap extends into the buttock crease posteriorly, this should be assessed as well. The entire lower extremity is examined for abnormalities, such as scar deformity, previous surgical sites, varicosities, asymmetry or edema.
The breasts and chest are examined to understand the potential volume match with the thigh. Is there enough medial thigh tissue to reconstruct the patient to their current size? If there is amastia, will the TUG provide enough of a skin paddle? The TUG is usually performed when volumes of 500 mL or less are needed, but as mentioned above, fat grafting or later augmentation under the flap can be performed. The potential for skin-sparing or nipple-sparing mastectomy is evaluated also. If the entire flap will not be de-epithelialized and the patient has hairy inner thigh skin, they may need later laser hair removal.
Although the risks of complete flap failure are small, consideration in the preoperative evaluation should be made in regard to what lifeboat surgeries the patient is a candidate for, in case of flap failure. Other free flap sources, such as the latissimus pedicled flap, or potential for implant reconstruction are evaluated by inspection and palpation.
If the patient is a TUG candidate, she should understand that the goal of the TUG reconstruction is to have a normal-appearing shape in clothing. Naked, in front of a mirror, there will be scars. If a unilateral reconstruction and donor area are planned, there will be thigh asymmetry postoperatively. The patient is counselled on this. In addition, lateral thigh fullness may be accentuated by medial thigh lifting. If that is the case, outer thigh liposuction might be considered at least three, but usually six months after reconstruction with the TUG. Patients are told a revision surgery, both in the reconstruction and donor area, may be necessary, just as in any breast reconstruction.
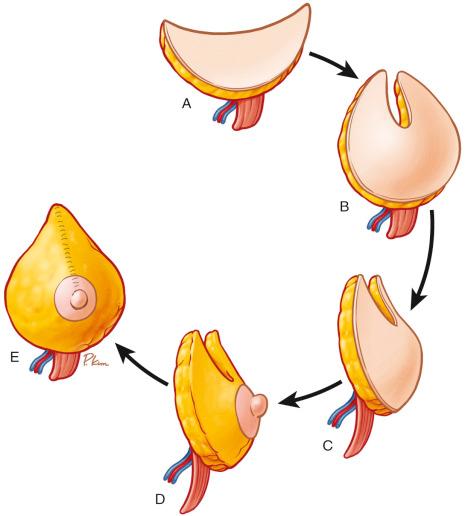
The unique design of the TUG donor area provides for natural flap folding and aesthetically pleasing breast shaping ( Fig. 7.2 ). In contrast to the DIEP or SIEA flap, the coned TUG flap provides improved projection, rather than the flat contour that can be characteristic of abdominal tissue breast reconstruction. Likewise, the TUG design and natural medial thigh donor skin color lend to immediate nipple–areola complex (NAC) reconstruction in some patients. The aesthetics of the TUG NAC are superior to tattooing with local nipple flap creation.
The risks of microsurgery, such as infection, bleeding, clotting, and delayed wound healing are covered in the preoperative evaluation. The patient should understand that closed suction drainage will be needed, and usually is in place for a minimum of two to three weeks. Seroma formation is possible and closed suction for a prolonged period helps minimize this issue.
Preoperative imaging of the donor area is not typically performed. The consistent blood supply of the TUG obviates the need for such an evaluation, unless the surgeon has a specific targeted question.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here