Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Kolff’s development of hemodialysis in the 1930s led to a series of advances in the care of patients with end-stage renal disease (ESRD). Although native arteriovenous fistulas and homografts were initial cannulation options for dialysis access, the availability of prosthetic grafts in the 1970s afforded a number of new access sites. Nonetheless, this new type of access generated a new set of complications and expenditures to the health care system, with economic costs of ESRD in the United States at more than $26 billion in 2006.
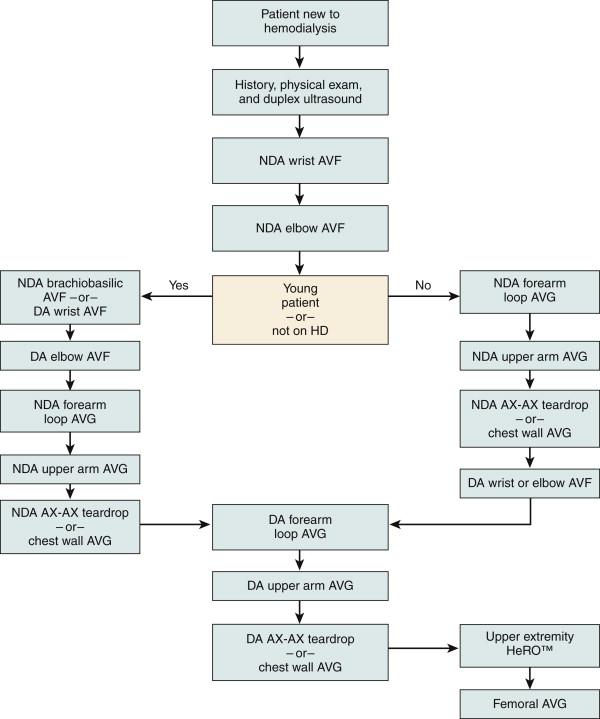
The National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative guidelines promote initial fistula formation in the nondominant extremity. The “fistula first” initiative would suggest creating autogenous access on the dominant upper extremity once native fistula options have been exhausted on the nondominant side. However, a common practice is to remain on the ipsilateral nondominant limb and proceed with a forearm loop or upper arm brachial artery–to–axillary vein arteriovenous graft (AVG).
History and physical examination. The decision to implant a forearm loop or brachial-axillary AVG depends on the existing arterial and venous anatomy. A thorough past medical history and a physical examination of the extremities and sites of previous vascular access should be obtained to preserve the greatest number of sites for future access ( Fig. 64-1 ). A strong palpable pulse is required to provide adequate inflow, and a weak pulse may indicate a proximal defect of the artery or heavily calcified vessels, neither of which allows ample flow to support hemodialysis and both of which may predispose the patient to arterial steal syndrome.
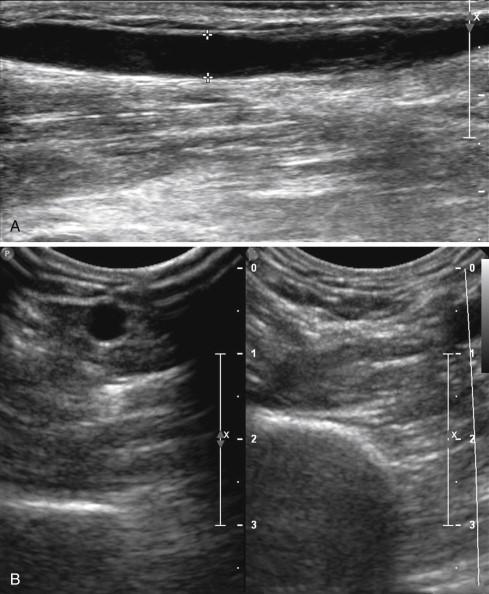
Venous imaging. Determining target vein patency and the quality of venous outflow is essential to careful planning ( Fig. 64-2 ). Venous duplex mapping is limited to determining the adequacy of venous outflow in the antebrachium, antecubital fossa, and axilla, but venography is required to effectively evaluate the central veins, if it is deemed clinically necessary because of a history of prior interventions. Magnetic resonance venography is an alternative to conventional venography, but images are less dynamic and patients with severe renal dysfunction are at risk of nephrogenic systemic fibrosis. However, recent advances in imaging and contrast technology allow for the use of Feraheme as a contrasting agent, which can safely be used in ESRD patients.
Preoperative dialysis. Patients taking hemodialysis require dialysis the day before or the morning of surgery.
Selection of adequate inflow and outflow sites. Inflow arteries must be relatively soft and amenable to clamping. Outflow veins should be greater than 3 mm in diameter and free from prior traumatic injury, thrombus, scar, or occlusion.
Arterial and nerve injury. Distraction performed too forcefully on neurovascular structures can lead to injury, including arterial dissection or neuropraxia.
Graft tunneling. Tunneling the graft too deeply can lead to difficulties in accessing the graft. Care must also be taken to prevent conduit twisting or kinking, which may occur when tunneling too tight of a loop for a forearm graft. When placing a brachial-axillary AVG, the preference is to position the graft posterior to the median nerve to avoid kinking, which can occur if the graft is draped anteriorly over the nerve.
Anastomosis. The anastomosis must be constructed at an appropriate angle and beveled to avoid kinking of the hood. Likewise, excessive tension can lead to tenting of the back wall of the artery at the anastomosis.
Central venous stenosis. A long-standing tunneled dialysis catheter may increase the risk of a central venous stenosis. Likewise, this catheter may need to be relocated before the placement of the access graft to minimize the risk of postoperative arm edema.
Once native fistula possibilities in the nondominant extremity have been exhausted, placement of a forearm AVG may be considered. A brachial-axillary AVG is a more proximal option usually reserved after failure of a forearm graft without the possibility for endovascular or surgical revision. Additional options include axillary artery–to–axillary vein grafts, chest wall grafts, or the hemodialysis reliable outflow (HeRO, Hemosphere, Eden Prairie, Minn.) “graft catheter” device.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here