Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Paronychia, felons, and flexor tenosynovitis (FTS) are some of the most common infectious pathologies seen among hand surgeons. They are most often bacterial in origin—with Staphylococcus aureus as the most common pathogen—and can be pyogenic (pus-forming).
Paronychia is an infection of the lateral or proximal nail fold and soft tissue, which can also extend to the germinal and sterile matrix beneath the nail.
A felon is a purulent infection that develops within the volar septate pulp tissue of a finger or thumb.
Pyogenic FTS is a purulent infection that occurs within the sheath surrounding the flexor tendons.
Pyogenic infections should be dealt with promptly to prevent tendon scarring and necrosis, soft-tissue loss, proximal migration, and bacteremia.
Rapid progression of pyogenic infections is common in patients with diabetes or IV drug use and among those who are immunocompromised.
A recent history of puncture or injury to the soft tissue is common, but not required, for the development of pyogenic infections of the finger and hands.
Bites are a common mechanism of hand infection. Cats specifically have sharp, needle-like teeth, delivering bacteria ( Pasteurella multocida )-laden saliva into wounds, which then quickly seal over. Human bites from physical altercations are also common, most frequently occurring on the dorsal ulnar hand at the level of the metacarpophalangeal joints.
There are no contraindications to surgical management of pyogenic infections of the fingers and hand. The adage “the sun never sets on an abscess” remains relevant, regardless of the clinical setting. Even in critically ill patients, most finger infections can be temporized by lancing at the bedside under a digital block.
Clinical examination is the hallmark of diagnosis for felons, paronychia, and pyogenic FTS. Laboratory markers, such as white blood cell count (WBC) and erythrocyte sedimentation rate/C-reactive protein (ESR/CRP), are commonly within normal limits and of little clinical utility.
Patients with a finger infection will often report a recent history of swelling, erythema, and worsening pain within the finger or hand.
The common physical examination findings of pyogenic FTS are classically described by Kanavel ( Fig. 5.1 ):
Fusiform swelling (also described as a “sausage digit”), with tense swelling along the entire length of the digit
Flexed posture
Tenderness to palpation along the flexor tendon sheath
Pain with passive digital extension

Felons are characterized by tense swelling of the volar pulp and a well-defined area of blanching overlying an obvious abscess ( Fig. 5.2 ). As the infection worsens and pressure increases, a type of localized compartment syndrome can develop within the septa of the pulp tissue, leading to extreme pain.

Paronychia are initially characterized by unilateral swelling, erythema, and pain of the lateral nail fold on one side. As the infection progresses, the swelling and erythema will affect both lateral nail folds and extend proximally into the dorsal skin of the digit ( Fig. 5.3 ).

X-rays are necessary to rule out associated osteomyelitis or bony destruction, subcutaneous gas formation, or any retained foreign bodies.
Ultrasound is useful when there is concern for proximal spread into the deep spaces of the hand or forearm. Pain that spreads from the finger to the hand or forearm should raise concern.
Magnetic resonance imaging (MRI) is of little clinical utility for simple felons, paronychia, and FTS and will only serve to delay treatment.
The flexor tendons of the fingers are contained by longitudinal sheaths, which are reinforced by the pulley systems within each individual finger. The A1, A3, and A5 pulleys originate around the distal necks and interphalangeal (IP) joints of the metacarpal, proximal phalanx, and middle phalanx, respectively. The A2 and A4 pulleys originate at the diaphysis of the proximal and middle phalanx, respectively, and function to prevent bow-stringing of the flexor tendons.
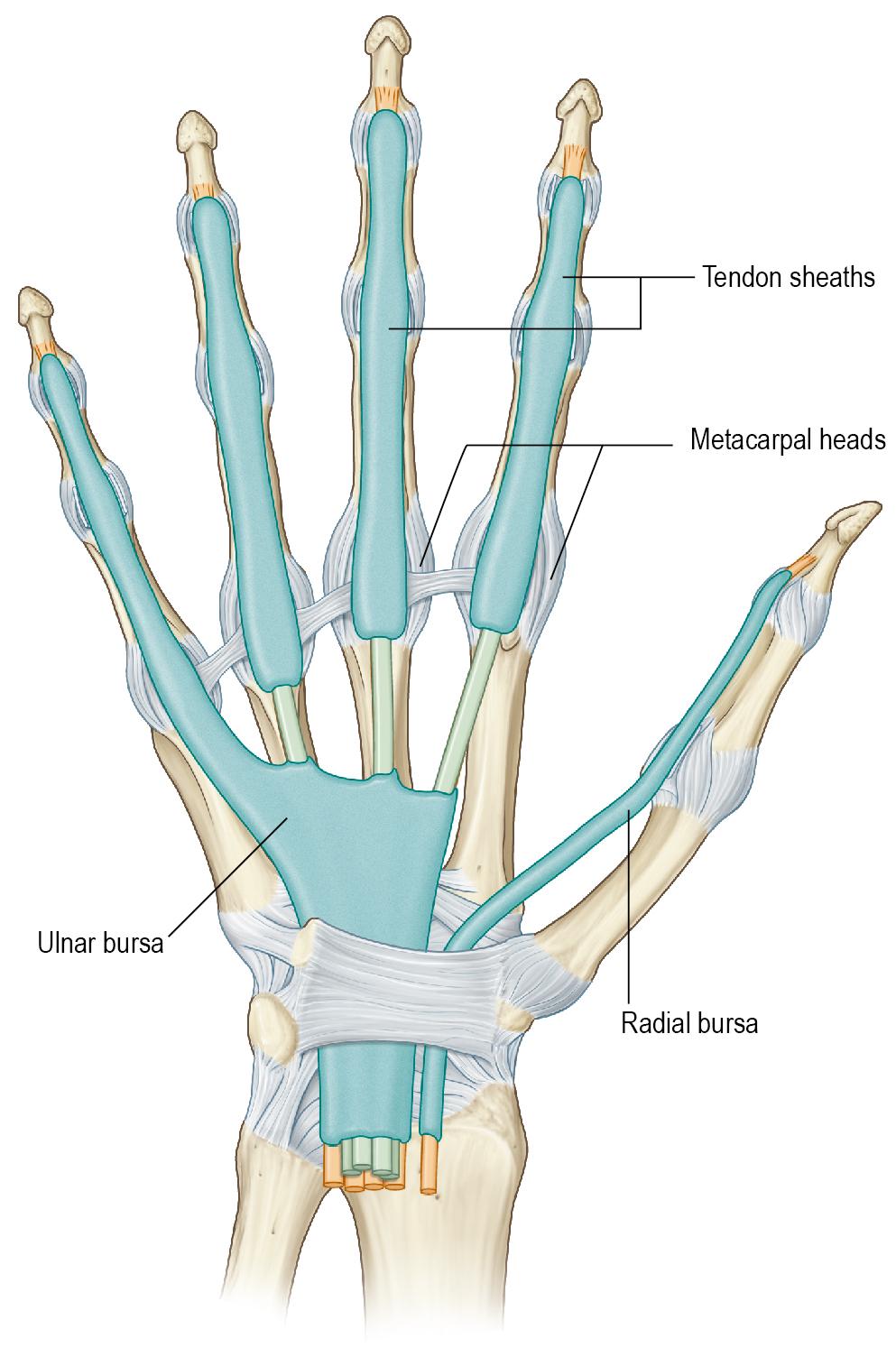
The flexor sheaths of multiple digits may be connected via radial and ulnar palmar bursa, although several anatomic variations have been described. The space of Parona, which is located proximally at a level between the carpal tunnel and pronator quadratus, often permits direct connections between bursa. The connections permit communication between the flexor tendons of the thumb and small finger and can facilitate seeding of the infection to the other digits. For example, a small finger pyogenic FTS can spread to include the thumb as well, forming a so-called “horseshoe abscess” ( Fig. 5.4 ).
Standard supine positioning with a hand table is used.
The inflammation associated with infections can cause increased surgical site bleeding, which makes it difficult to define normal anatomy. Use a digital or forearm-based tourniquet as necessary. Do not exsanguinate before inflation because this can force proximal extension of an underlying abscess. Instead, elevate the arm and let gravity assist with venous drainage before tourniquet inflation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here