Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The filarial parasites covered in this chapter constitute a group of tissue-dwelling filarial nematodes that persist in the human host for years, causing damage to the lymphatic system that leads to elephantiasis and genital hydroceles (in the case of lymphatic filariasis) or marked inflammatory reactions in the skin and eyes leading to blindness (in the case of onchocerciasis). Both diseases are designated neglected tropical diseases by the World Health Organization (WHO). Global elimination efforts are addressing this significant health burden, using annual or twice-annual mass drug administration of donated anthelmintic drugs in concert with vector-control measures. Significant progress has been made, particularly on onchocerciasis elimination from the Americas. A remaining challenge is to develop a strategy to use in areas of Africa co-endemic for Loa loa and lymphatic filariasis or onchocerciasis—where the existing drug regimens can precipitate significant adverse side effects due to rapid die-off of the high numbers of L. loa parasites. Another challenge is developing more effective macrofilaricidal treatments to kill adult worms in order to shorten the duration of mass drug administration elimination programs.
A 23-year-old male from the Democratic Republic of Congo presented to the emergency room complaining of a worm in his eye. The patient had lived in rural Congo, bathed in lakes and rivers, and had friends with river blindness. For the past year, he had noted sporadic nontender swellings on his arms which resolved spontaneously. Past medical history was unremarkable, and he was taking no medications. The exam confirmed the presented of a 5-mm, moving worm in the scleral conjunctiva with mild conjunctival injection. There was mild photophobia without discharge. Ophthalmologic exam showed cornea was clear, no evidence of uveitis, and normal retina. There were no subcutaneous nodules or dermatitis. White blood cell count was normal, except for 43% eosinophils. Direct visualization of the ocular adult worm was considered diagnostic of L. loa ; however, additional testing was required to evaluate for co-infection and microfilarial burden in order to guide treatment. Filarial IgG antibody level was positive; onchocercal IgG4, which was done to rule out co-infection with onchocerciasis, was negative. Thick smear of blood showed microfilaria with the characteristic L. loa sheath at the tail and a low level of microfilaremia. Since diethylcarbamazine (DEC), the drug of choice for treatment of L. loa , is contraindicated in patients with onchocerciasis due to the risk of severe ocular inflammation and resulting blindness, as a precaution, the Centers for Disease Control and Prevention (CDC) required pretreatment of the patient with ivermectin for potential onchocerciasis co-infection, before releasing the DEC for treatment of the L. loa .
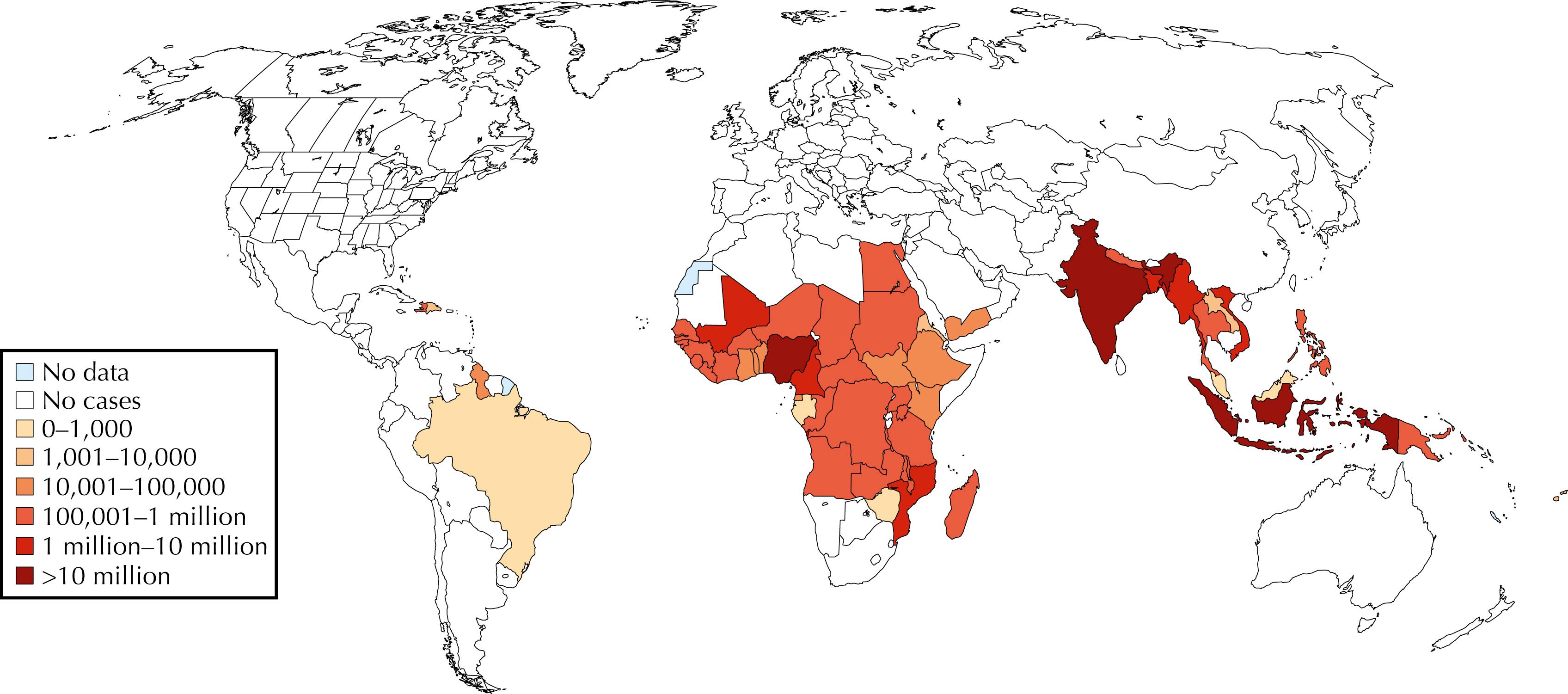
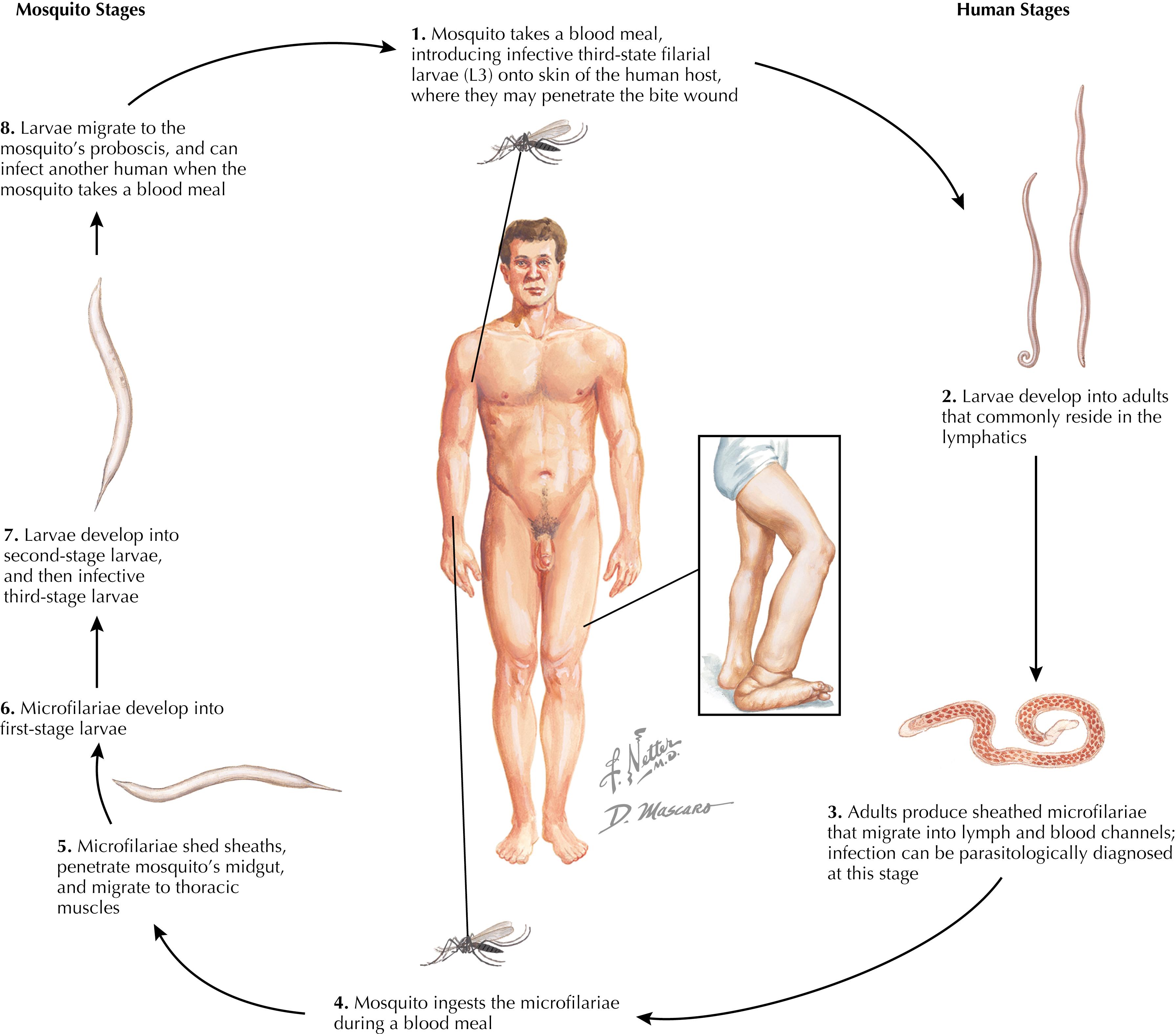
Lymphatic filariasis is a leading cause of permanent and long-term disability worldwide. W. bancrofti is responsible for the vast majority of cases and is found throughout the tropics and in some subtropical areas worldwide ( Fig. 84.1 ; Table 84.1 ). B. malayi is present in South, Southeast, and East Asia. B. timori is restricted to the island of Timor and its environs. The global burden of lymphatic filariasis is not well defined, but it is known to be endemic in 72 countries, placing 1 billion persons at risk, with the WHO most recently estimating 120 million people to be currently infected—2% of the world’s population. Of these, 44 million have clinical manifestations such as lymphedema, elephantiasis, hydrocele, lymphangitis, chyluria, and renal disease. The remaining infected individuals often have subclinical lymphatic or renal injury. In addition to the disease burden, there is a significant social, psychological, and economic burden owing to social stigma, physical stigmata, and inability to work. The current estimates are that 4.6 million disability-adjusted life years (DALYs) are lost each year to this disease.
| Parasite Species (Disease Name) | Distribution | Vector | Adult Location | Microfilariae Location | Clinical Features |
|---|---|---|---|---|---|
| Wuchereria bancrofti (bancroftian lymphatic filariasis) | Tropical regions | Anopheles , Aedes , and Culex species | Lymphatics | Blood | Lymphangitis Elephantiasis Hydrocele Chyluria |
| Brugia malayi (brugian lymphatic filariasis) | South, East, and Southeast Asia | Mansonia , Anopheles , and Aedes species | Lymphatics | Blood | Lymphangitis Elephantiasis |
| Brugia timori (brugian lymphatic filariasis) | Indonesia | Anopheles species | Lymphatics | Blood | Lymphangitis Elephantiasis |
| Onchocerca volvulus (onchocerciasis, river blindness) | Africa, Central and South America | Simulium species | Skin | Skin | Dermatitis Subcutaneous nodules Eye lesions Visual impairment |
| Loa loa (loiasis) | Central and West Africa | Chrysops species | Connective tissue | Blood | Calabar swellings Subconjunctival eye worm |
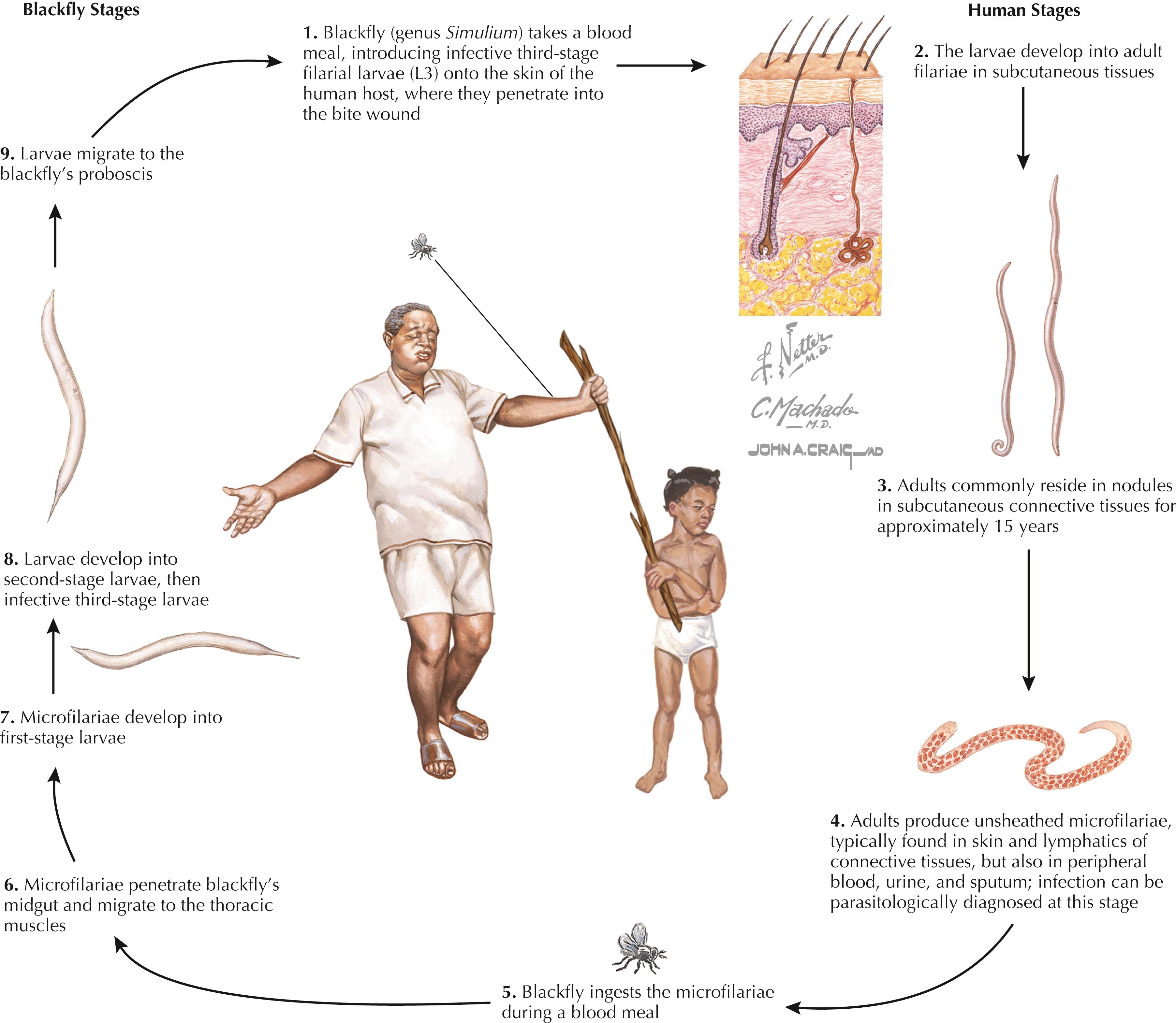
Onchocerciasis, commonly called river blindness , is caused by the filarial parasite O. volvulus and is one of the most common infectious causes of blindness worldwide, second only to trachoma. There are an estimated 25 million infected individuals in 30 countries, primarily in Africa but also Yemen and limited areas of the Americas, with 123 million living in endemic areas and at risk of infection ( Fig. 84.2 ). Of those infected, an estimated 300,000 individuals are blind and another 800,000 are visually impaired. Each year, 1,990,000 DALYs are lost to onchocerciasis; of those, approximately 40% are a result of eye disease and 60% from severe skin manifestations. This disability affects not only the infected patients but also the children who escort blind individuals, preventing them from attending school. Fertile riverine areas needed for agricultural development are abandoned because of the risk of this disease, which has devastating socioeconomic consequences. Infections outside of endemic populations may occur in expatriates, usually only those living for a prolonged period in affected areas.
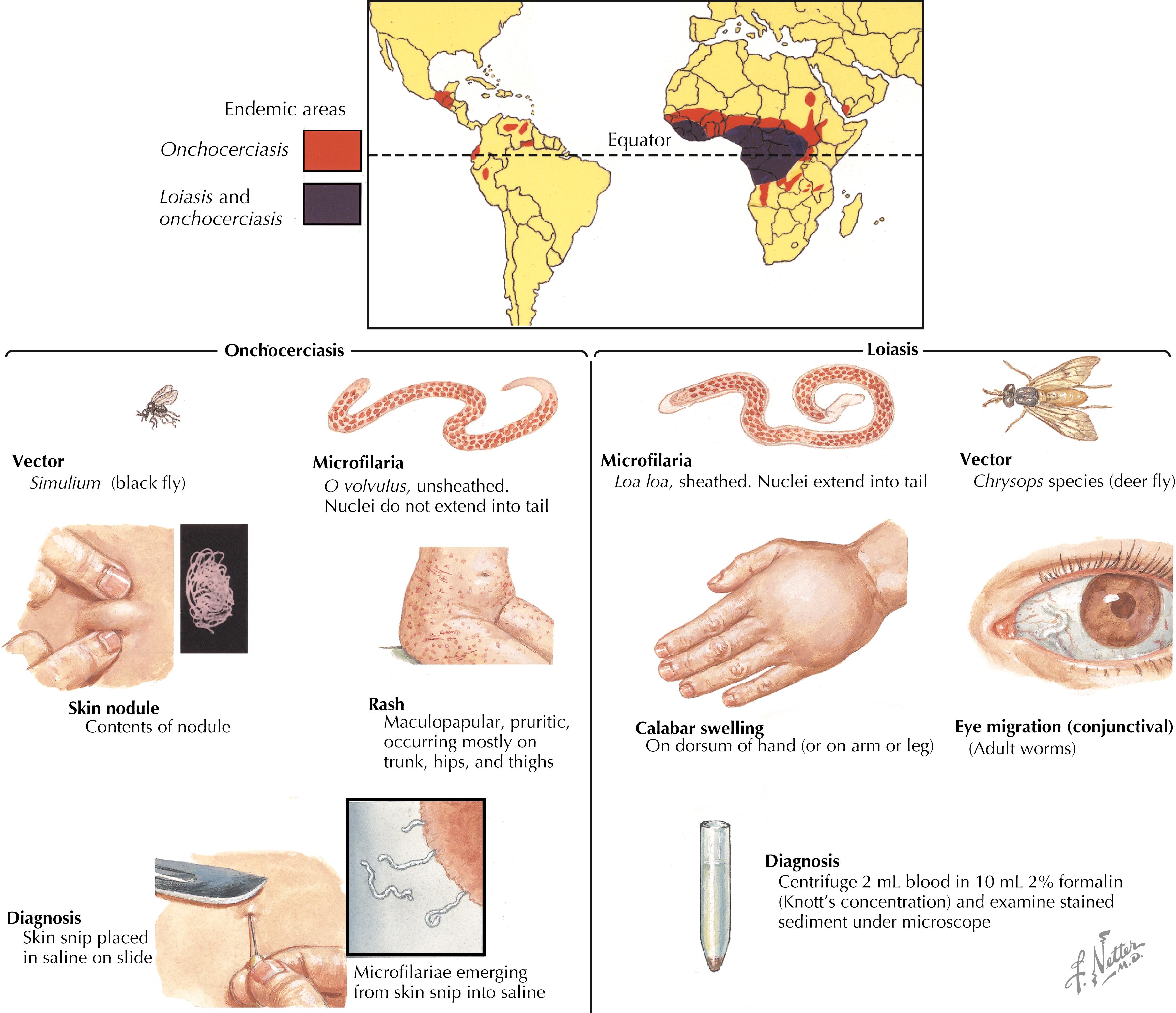
Loiasis occurs only in rainforest and swamp forest areas of Central and West Africa, as its distribution is primarily restricted by its transmission vector (see Fig. 84.2 ). Its primary significance is its co-endemicity in areas of Africa with lymphatic filariasis and onchocerciasis, because patients with L. loa co-infection cannot be treated with the usual anti-microfilarial regimens used in mass drug administration programs owing to side effects from high numbers of dying L. loa microfilariae in the circulation and tissues.
Risk factors for acquisition of the mosquito-borne filarial parasites W. bancrofti , B. malayi , and B. timori include living in endemic areas with exposure to a broad range of potential vectors that promote human-to-human spread (see Table 84.1 ). For lymphatic filariasis, the mosquito vectors are diverse and include Anopheles species, Culex species, Aedes species, and Mansonia species. Infants, children, and adults are exposed to mosquitoes carrying infective larvae ( Fig. 84.3 ). There is no natural animal reservoir for W. bancrofti or B. timori , but a very small percentage (under 5%) of domestic and wild animals such as monkeys and cats tested have been found to be infected with B. malayi . Urbanization in endemic areas may be contributing to an increased risk of lymphatic filariasis because infected and susceptible individuals may then live in close proximity to each other and to stagnant, contaminated water that provides a breeding ground for the vector. Irrigation projects may further increase risk.
Onchocerciasis is termed river blindness because the vector, the Simulium species black fly, breeds along rivers in fast-flowing water where its larvae can filter feed. Residents along rivers are at highest risk, but the fly has also been carried by monsoon winds for hundreds of kilometers, reinfecting areas that have previously eradicated the fly vector. There is no animal reservoir for onchocerciasis, and transmission is human to human (see Fig. 84.4 ). The severity of ocular disease varies considerably among geographic zones, possibly based on the different vector-parasite complexes. The disease in the West African savanna is responsible for the most severe ocular disease; in the most affected villages, more than 10% of the population may be blind.
L. loa is transmitted by the day-biting tabanid deer flies of the genus Chrysops , which rest in the forest canopy and lay eggs in mud, so transmission is primarily in the rainy season. The flies become infected during a blood meal taken from an infected human and transmit the infective microfilariae (larvae) during subsequent human bites.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here