Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
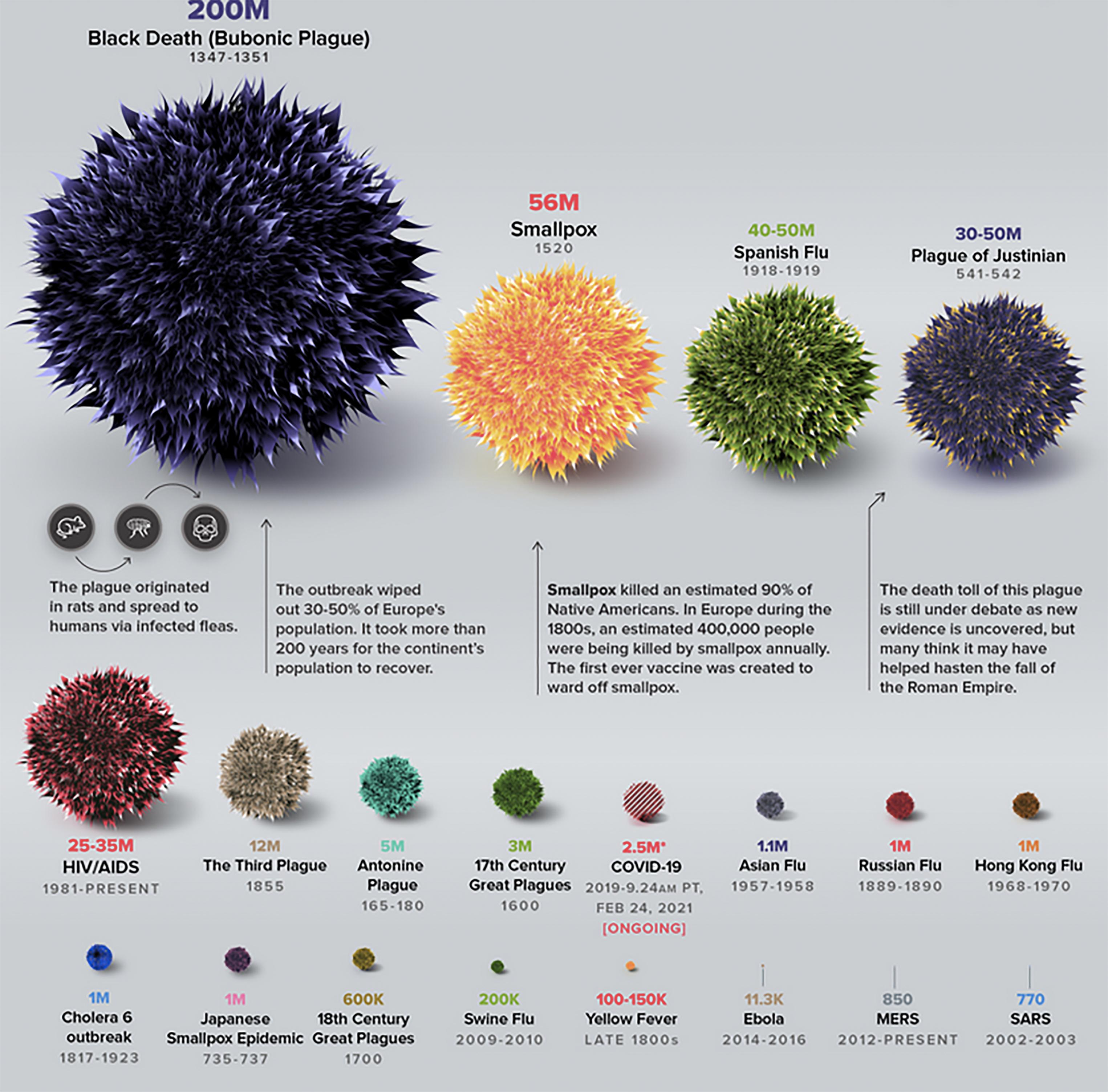
China awoke on December 31, 2019 to the first public message from the Wuhan Municipal Health Commission alerting its residents of a cluster of 27 cases of viral pneumonia of unknown etiology that had emerged in Wuhan, capital of the Hubei province and home to over 11 million people. The news reached the US Centers for Disease Control and Prevention (CDC) later that day. Four days later, the genomic sequence of the new respiratory virus was established by the Chinese National Institute of Viral Disease Control and Prevention (NIVDC), which isolated the pathogen from patients in Wuhan and named it novel coronavirus, or 2019-nCoV. The sequence was posted on the NIH genetic sequence database, GenBank, on January 13, 2020. On that day, the first case outside of China was confirmed in Thailand, and a week later the United States in turn reported its first case. On February 11, the International Committee on Taxonomy of Viruses (ICTV) rebaptized the virus SARS-CoV-2 due to the similarity of its genetic sequence with the virus responsible for the 2003 Severe Acute Respiratory Syndrome (SARS) outbreak. That same day, the World Health Organization (WHO) named the disease produced by SARS-CoV-2, COVID-19, an acronym which stands for Coronavirus Disease 2019. By mid-February 2020, the global death toll had surpassed the one thousand mark, exceeding the fatalities caused by the SARS and Middle East Respiratory Syndrome (MERS) epidemics (774 and 866 lives, respectively; Fig. 1.1 ). The WHO eventually declared the outbreak a global pandemic on March 11, 2020, 6 weeks after its designation of “public health emergency of international concern.”
Coronaviruses belong to the Coronaviridae family of single-stranded RNA viruses. They owe their name to their characteristic appearance under electron microscopy: a viral envelope with petal-like spike projections, akin to the solar corona. Coronaviruses are divided into four main genera based on their genomic characteristics: Alphacoronavirus, Betacoronavirus , Gammacoronavirus , and Deltacoronavirus . The first two genera are known to infect mammals (including humans), while the last two predominantly infect birds along with pigs. There are currently seven known human coronaviruses that have been recognized since the 1960s. Three of them, MERS-CoV, SARS-CoV, and the novel SARS-CoV-2, are beta-coronaviruses and are credited with large outbreaks and the ability to produce severe respiratory and extrapulmonary symptoms. The other four, HCoV-NL63 and HCoV-229E of the Alphacoronavirus genus, and HCoV-OC43 and HCoVHKU1 of the Betacoronavirus genus, however, usually only cause a mild upper respiratory tract illness.
Phylogenetic genomic analyses of isolated SARS-CoV-2 virions confirm the zoonotic nature of viral transmission to humans. These analyses have revealed a high degree of similarity with the genomes of horseshoe bat coronaviruses, making bats of the Rhinolophus genus the most likely primary reservoir for the novel coronavirus. Specifically, SARS-CoV-2 shares 96.2% of its genomic identity with the BatCoV-RaTG13 strain, and 87%–88% with the bat-SL-CoVZC45 and bat-SL-CoVZXC21 strains. There is less similarity with the genome of SARS-CoV (79%) and even less with that of MERS-CoV (50%). Interestingly, while the whole genome of SARS-CoV-2 is closest to that of bat coronaviruses, the receptor-binding domain (RBD) of the spike protein responsible for the docking of the virion particle to the angiotensin-converting enzyme 2 (ACE2) receptor on human cells ( Chapter 2 ) is closest to that of a SARS-like coronavirus isolated from dead Malayan pangolins smuggled into the Guangdong province of China. One of the posited putative mechanisms for the origin and zoonotic transfer to humans of SARS-CoV-2 is therefore the genetic recombination of bat and pangolin coronaviruses within an animal host that has yet to be fully identified, followed by a “jump” to humans which then acquired enough adaptations to enable a human-to-human transmission. Although beyond the scope of this manual, the theory of laboratory manipulations being at the origin of the emergence of SARS-CoV-2 is disputed and believed to be largely improbable.
At the start of the outbreak in China, the Huanan Seafood Wholesale Market in Wuhan came under the lens of policy officials and scientists for being the location where the SARS-CoV-2 outbreak may have originated as a majority of the initial cases were traced back to exposure to the market. The “wet” part of the market where wildlife is commonly traded has been under particular scrutiny as mounting phylogenetic data identified pangolins and bats as likely reservoirs and intermediate hosts of the virus. To this day, the claim that the Wuhan market is at the origin of the outbreak remains significantly contested since many initial cases could not be traced back to the market and, reportedly, no animal samples tested positive for the virus.
As of late 2020, the rise of so-called “variants” has been a source of concern for scientists and public officials worldwide. These viral mutants are problematic because, compared to the “wild-type” SARS-CoV-2 virus, they are transmitted more efficiently, evade currently established diagnostic tests, are more resistant to available treatments, make developed vaccines less effective, and can produce more severe disease. Variants that fulfill the above criteria of enhanced transmissibility and virulence are referred to as “variants of concern,” or VOC. Five such VOCs have been detected in the United States and are the object of close monitoring by the CDC and other federal agencies. At the end of February 2021, the most rampant variant in the United States was the B.1.429 variant, initially detected in California and making up about 8% of all SARS-CoV-2 lineages in the country. Another variant, B.1.427, also discovered in California, represents 3.3% of all lineages found in the United States. Both variants have a 20% increased transmissibility and have a moderate impact on the efficacy of therapeutics and reduced neutralization by antibodies produced during the previous infection or vaccination. A close third is the “United Kingdom” or B.1.1.7 variant which accounts for 2.6% of lineages in the United States. Although it is more transmissible than other VOCs (~ 50%), it appears to have only a minimal impact on the efficacy of therapeutics and convalescent or postvaccination antibody neutralization. Finally, the “South African” B.1.351 and “Brazilian/Japanese” P.1 variants only account for 0.1%–0.2% of all lineages found in the United States at the time of writing.
What started in January 2020 as an outbreak seemingly confined to a single region in China spread with astounding velocity to all continents, vehicled by the free movement of people, powered by the engines of globalization. While it took over 3 months to reach the first 100,000 cases, the global doubling time, i.e., the period of time it takes for the number of cases to double worldwide, came down to only 6 days at the end of March 2020. The first million cases were reached on April 2, 2020. The month of June saw a spectacular acceleration of the global caseload, with one million increments occurring every 7–8 days. For most societies, the summer of 2020 (July to September) came as a period of relative lull with regard to the spread of the virus allowing communities to reopen businesses and governments to loosen restrictions. This slowing of viral activity was, however, short-lived and, from October 2020 to January 2021, a sharp increase in cases and fatalities spiked across the world as people were drawn closer together indoors due to holiday celebrations and colder temperatures in the Northern Hemisphere. With much anticipation, the eyes of the world were turned to the progress made in the development of vaccines, approval for their emergency use, and mass vaccination campaigns. December 2020 marks the beginning of vaccination rollouts, starting in the United Kingdom and quickly spreading across the world. At the time of writing, as the world slowly gets immunized, the curves have started to show a decline in the rates of deaths and new cases, amid concerns of rising deadly variants. By the beginning of March 2021, over a year after it first emerged, SARS-CoV-2 had claimed 2.53 million lives, infected a known 114 million cases, and led the governments of more than half of the world population to enforce some form of confinement. The following section presents a timeline of the pandemic worldwide, highlighting important dates and events related to viral transmission, drug/vaccine development, and lockdowns.
January 1: Chinese health authorities order the closure of the Huanan Seafood Wholesale Market in Wuhan to carry out investigations and disinfection.
January 13: China reports the first death attributed to COVID-19.
January 20: Human-to-human transmission is confirmed by the China National Health Commission. The United States confirms its first case of a man from Washington state who had recently returned from a trip to Wuhan.
January 23: Wuhan, accompanied by other Chinese cities, shuts down all public transportation and goes into an official lockdown as countries around the globe start restricting flights from and to China.
January 24: France reports its first cases of COVID-19, the first in the European Union (EU).
January 26: The Chinese Center for Disease Control and Prevention (CCDC) starts to develop vaccines against SARS-CoV-2.
February 2: First death outside of China is reported in the Philippines.
February 3: China begins a clinical trial of Gilead’s remdesivir on patients with COVID-19. The drug was previously investigated during the Ebola outbreak.
February 5: The Diamond Princess cruise ship docks in the port of Yokohama, Japan, with several passengers suspected of having contracted COVID-19. The ship remained in quarantine until March 1, its passengers gradually repatriated to their countries of origin. The ship outbreak eventually totaled 712 confirmed cases and 13 deaths.
February 22-March: The period stretching from the third week of February into March was marked by a rapid spread of the infection across Western Europe which became a new epicenter of the outbreak. Northern Italy led the number of cases and fatalities, closely followed by France, Spain, and Germany, rapidly overwhelming the health-care system in these countries.
February 26: Brazil confirms its first case of COVID-19, the first in South America. By this day, every continent with the exception of Antarctica has had confirmed COVID-19 cases.
February 29: The United States reports its first death from the virus, but earlier fatalities may have occurred in retrospect.
March 11: The WHO declares the COVID-19 outbreak a pandemic.
March 15: The first stay-at-home order in the United States is issued by Puerto Rico, followed by most US states in the next 2 weeks.
March 17: The EU, which now has “more reported cases and deaths than the rest of the world combined, apart from China,” officially closes its borders to nonessential international travel. The travel restriction, initially set to last 30 days, was extended twice and has been undergoing gradual lifting with select countries since July 1, based on epidemiological, social, and economic considerations.
March 18: The WHO launches the Solidarity trial which aims at comparing several treatments against COVID-19: remdesivir, chloroquine, hydroxychloroquine, lopinavir/ritonavir, and interferon-beta. Participating countries are Argentina, Bahrain, Canada, France, Iran, Norway, South Africa, Spain, Switzerland, and Thailand.
March 26: The United States now has more COVID-19 cases than any other country in the globe. This trend continues through at least August 2020.
April 2: The number of COVID-19 cases around the world exceeds the million mark. More than 50,000 people have died from the virus worldwide.
April 18: Use of hospital resources (ventilators, ICU, and all hospital beds) in the United States reaches its peak during the first wave of the pandemic.
April 28: The number of cases surpasses one million in the United States and the death toll in the country exceeds that incurred during the Vietnam war.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here