Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Traumatic facial nerve palsy has been associated with birth weight greater than 3500 g, forceps-assisted deliveries, and prematurity.
When facial nerve paralysis is of developmental origin, it may be part of a broader pattern of altered morphogenesis.
Facial paralysis with associated distal limb deficiency has been seen after early chorion villus sampling, failed dilation and curettage, maternal use of either thalidomide or misoprostol after the first trimester, and maternal hyperthermia during the first trimester, suggesting it may be a manifestation of brainstem disturbances during the first trimester.
Facial nerve palsy is usually unilateral, and decreased movement on the side of the palsy occurs with facial animation.
The surgical treatment of facial paralysis consists of staged techniques using autologous muscle or tendon transplantation to the paralyzed side of the face or reanimation procedures using regional muscle transfers and nerve crossovers.
Prolonged compression or stretching of a peripheral nerve may lead to compression palsy, apparently because of neural ischemia. Developmental congenital unilateral facial palsy has an estimated incidence of 2.1 per 1000. The mechanism of injury is usually either direct trauma from delivery or compression of the side of the face and nerve against the sacral promontory, with the side of the injured facial nerve usually corresponding with the side of the fetal face that was lying against the maternal sacrum during delivery. The facial nerve exits the skull through the stylomastoid foramen behind the ear, where it is protected by the mastoid bone, and then travels to the parotid gland, where it divides and sends branches to all the muscles of the face. Direct compression may occur behind the ear or over the parotid region, although both the maternal sacral promontory and fetal shoulder can also cause intrauterine nerve compression. Traumatic cases are usually unilateral and present with weakness of the frontalis, orbicularis oculi, buccinator, orbicularis oris, and platysma. There may be a history of prolonged or difficult labor or forceps delivery, or evidence of periauricular ecchymoses or hemotympanum. Traumatic facial nerve palsy has been associated with birth weight greater than 3500 g, forceps-assisted deliveries, and prematurity.
Congenital facial nerve paralysis is generally considered to be of either developmental or traumatic origin. When facial nerve paralysis is of developmental origin, it may be part of a broader pattern of altered morphogenesis, such as Möbius sequence ( Fig. 14.1 ), oculoauriculovertebral sequence (hemifacial microsomia) ( Fig. 14.2 ), or CHARGE syndrome (coloboma, heart disease, atresia choanae, retarded growth and development, and/or central nervous system anomalies, genital hypoplasia, and ear anomalies and/or deafness) ( Fig. 14.3 ). In oculoauriculovertebral sequence there is unilateral microtia with conductive deafness and varying degrees of jaw hypoplasia, ocular dermoids, and cervical vertebral abnormalities. CHARGE syndrome can be associated with other cranial nerve deficits, ocular colobomata, choanal atresia, dysplastic ears with sensorineural deafness, hypoplasia of the cochlea and semicircular canals, heart defects, and hypogonadotropic hypogonadism. Of importance to surgeons doing free functional muscle transfers to reanimate the face, facial vessel agenesis is more common in syndromic congenital facial palsy than in those with isolated congenital facial palsy.
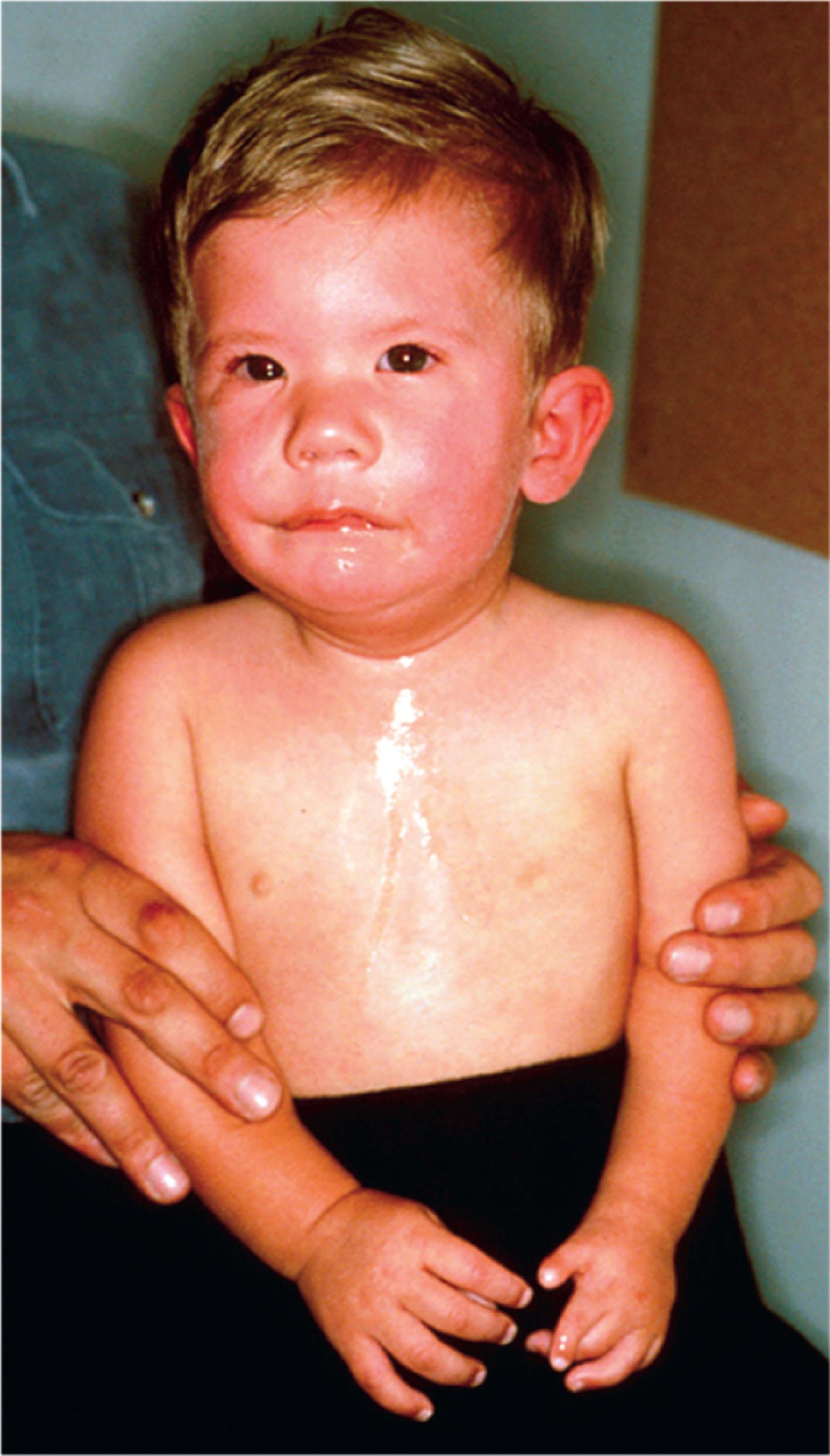
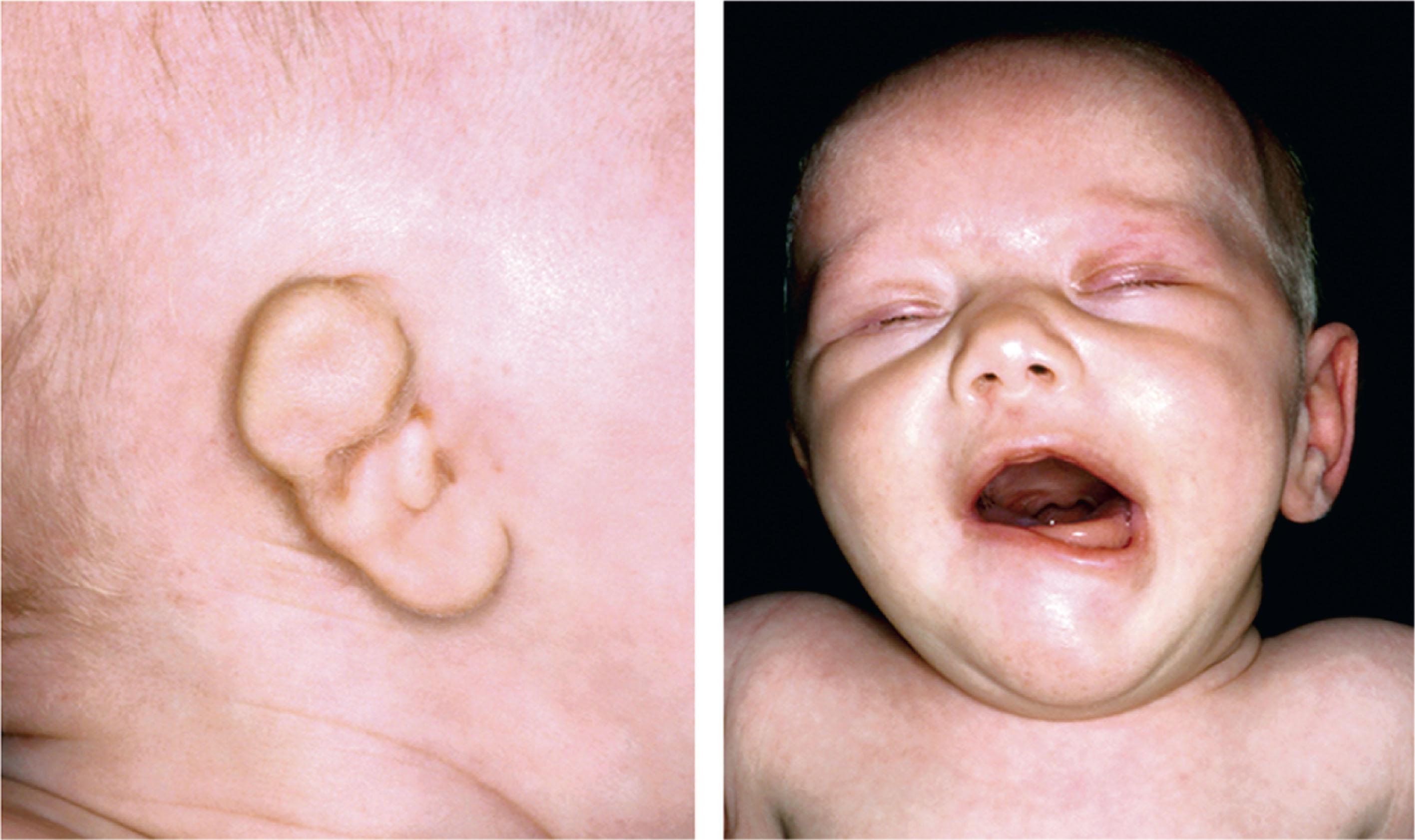

Facial paralysis with associated distal limb deficiency has been seen after early chorion villus sampling, failed dilation and curettage, maternal use of either thalidomide or misoprostol after the first trimester, and maternal hyperthermia during the first trimester, suggesting it may be a manifestation of brainstem disturbances during the first trimester. Congenital facial paralysis of traumatic etiology in otherwise normal children accounts for 8–25% of all facial nerve palsies occurring in the pediatric population, and it requires a systematic evaluation to exclude other syndromic associated anomalies, particularly those affecting vision and hearing. Among 118 cases of aural atresia (see Fig. 14.2 ), facial nerve anomalies were present in 13%, and inner ear anomalies were present in 22%.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here