Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
![]() Access video content for this chapter online at Elsevier eBooks+
Access video content for this chapter online at Elsevier eBooks+
Transgender patients typically do not identify with the gender assigned at birth. Both the genital sex, as well as the secondary sex characteristics that develop during puberty, produce clinically significant psychological distress, also known as gender dysphoria. A complex and extended transition period is usually required that involves numerous diagnostic processes, medical-surgical treatments, and extensive psychological support. All of this is aimed at allowing patients to achieve the physical expression of the gender with which they identify, averting severe psychological conflicts, improving self-esteem and quality of life, decreasing the risk of social stigma and interpersonal violence, and fostering the patient’s successful integration into the workplace, family, and society.
One of these medical-surgical treatments, facial surgery – popularly known as facial feminization surgery (FFS) – has steadily gained importance and is emerging as a key element in the complex transition process, primarily for transfeminine patients. In combination with hormone therapy (HT), FFS can be considered as fundamental as genital reconstruction. Despite the evidence regarding the importance of and need for facial treatment for this group, many gaps remain that must be addressed, and views differ about the role that this surgery plays in the treatment algorithm. There is a need for a clear, concise definition of the different treatments involved, the type of patient for whom this surgery is indicated, and its place in the transition process timeline.
From a technical point of view, FFS can be defined as the set of surgical procedures associated with different surgical specialties (oral and maxillofacial surgery, craniofacial surgery, plastic and reconstructive surgery) designed to soften and modify facial features perceived as masculine or non-harmonic, and which, therefore, are decisive in the visual identification of facial gender. On a somewhat philosophical note, a much more specific term would better suit the type of surgery discussed in this chapter: facial gender-affirmation or gender-confirmation surgery (FGCS). The popularly known concept of FFS is, in fact, so broad that it can include groups of patients without any gender identity problems, for whom the techniques included in FFS are absolutely indicated (e.g., cis females with unusually prominent supraorbital ridges or cis males with especially wide jaws). This new term, facial gender-confirmation, indicates that although the surgical techniques are the same, their objective is very clear-cut and, moreover, they are intended for specific patients with well-defined needs. This chapter focuses exclusively on FGCS for transfeminine patients, due to the low incidence of surgical treatment in transgender male patients and its near absence in the scientific literature reviewed. With more readily available access to care, it is to be expected that patients who identify as transgender males will also increasingly seek out some aspects of FGCS as outlined above.
The World Professional Association for Transgender Health (WPATH) has established internationally accepted Standards of Care (SOC) with recommendations of the best practices in the healthcare of transgender and gender diverse people. Until the release of Version 8 of the SOC in September 2022, FGCS could technically still be considered as cosmetic in nature. Now, FGCS has been categorized as a medical necessity. Current literature demonstrates that FGCS improves quality of life in the mid- and long-term; individuals report high levels of satisfaction with their surgical results; and individuals are significantly more satisfied with the appearance of their face compared to individuals who had not undergone surgery. Additionally, all studies reported a low complication rate and no mortality. The results were direct and consistent, although partly imprecise due to certain study limitations. Further research focusing on separate aspects of FGCS is both encouraged and necessary.
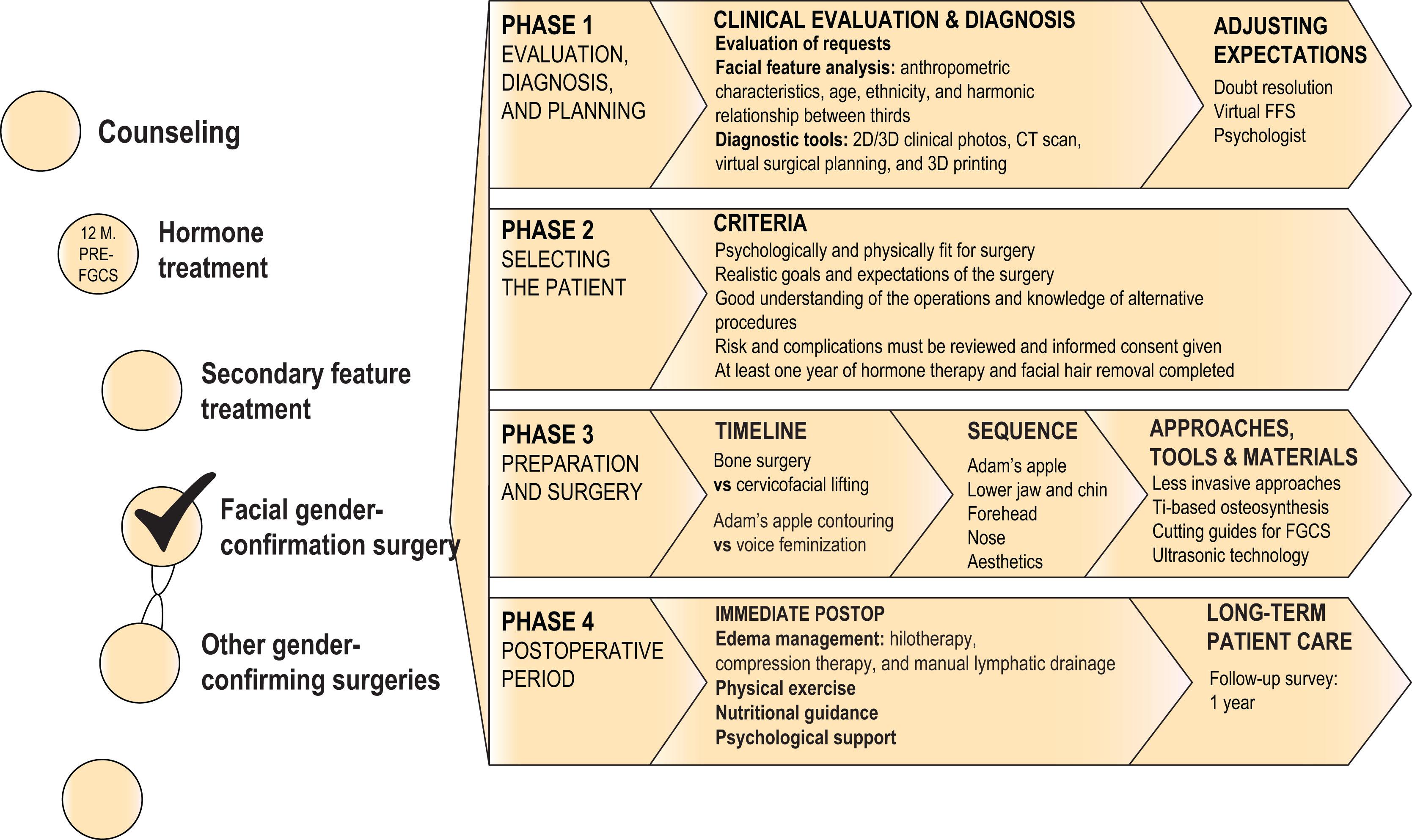
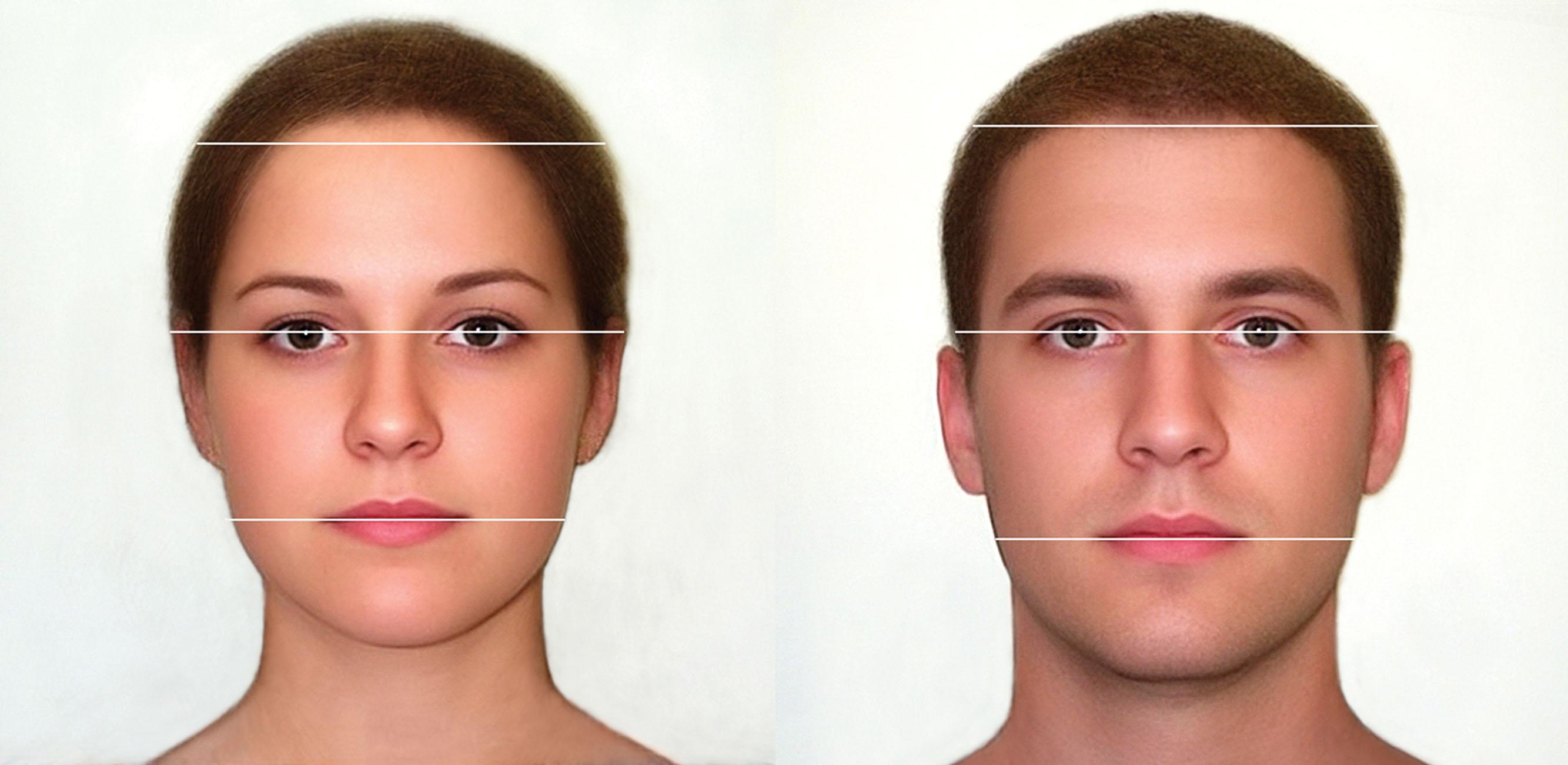
This chapter presents clear guidelines for specialists treating transfeminine patients who plan to undergo FGCS based on over a decade of practice in our clinic ( Fig. 17.1 ). We have slowly developed and honed these principles while working with over 2300 facial gender surgery patients in our center from August 2008 to April 2023. During that time, we have confirmed that it is crucial to identify the features that make a face masculine, know the appropriate tools to use in each case, and have a thorough understanding of the correct surgical techniques required in each situation, always being guided by the dual criteria of safety and natural results. Moreover, as one of the fastest-growing areas within plastic surgery, fact-based information about gender surgery must be disseminated to improve patient outcomes and foster innovation in the field.
Each patient has a unique facial structure, making it important to adapt surgical options to a patient’s individual needs rather than taking a standardized approach. The clinical evaluation consists of recognizing the features that contribute to male facial identification and identifying which of those can be realistically and predictably modified with surgery. Each of the features must be evaluated not only on an individual basis, but also in the context of the proportionality and symmetry of the entire face. The indication for facial feminization procedures must be based on the clinical parameters of the patient, as well as on a detailed anatomical study of the craniofacial structure, which will be used to design the surgical plan.
Genetic sex is determined at conception, but gonadal hormones play a vital role in the differentiation of male and female phenotypes throughout human development. Prenatal and adolescent levels of testosterone, the most abundant androgen, condition the appearance of facial features related to gender identity, which can be divided into primary (structural) and secondary aspects (non-structural).
These differentiating features appear in the fronto-naso-orbital complex, the nose, the malar region, the lower jaw, and the thyroid cartilage ( Fig. 17.2 ). As the growth of these structures under hormonal influence is not reversible pharmacologically, these features are generally approached and modified using surgery.
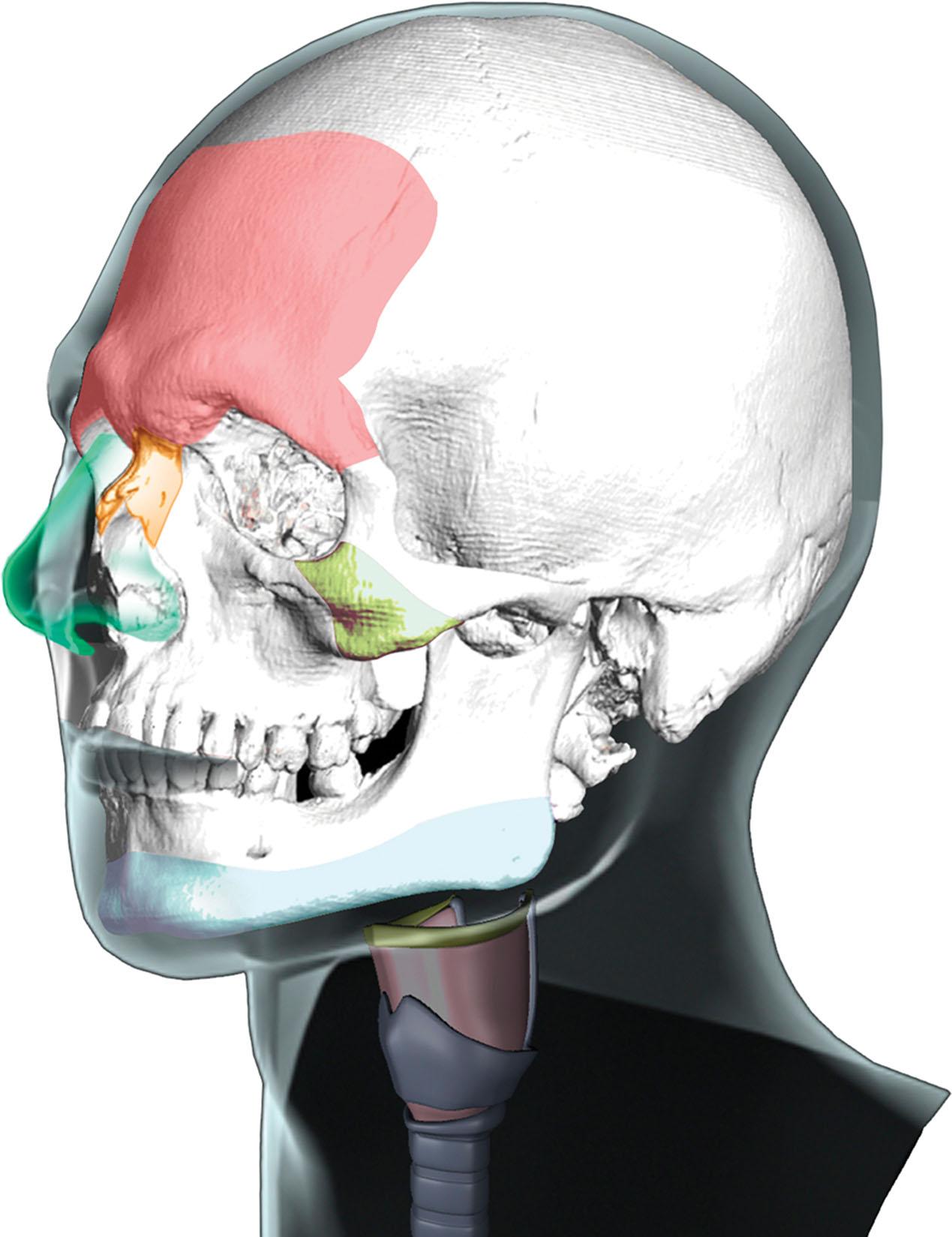
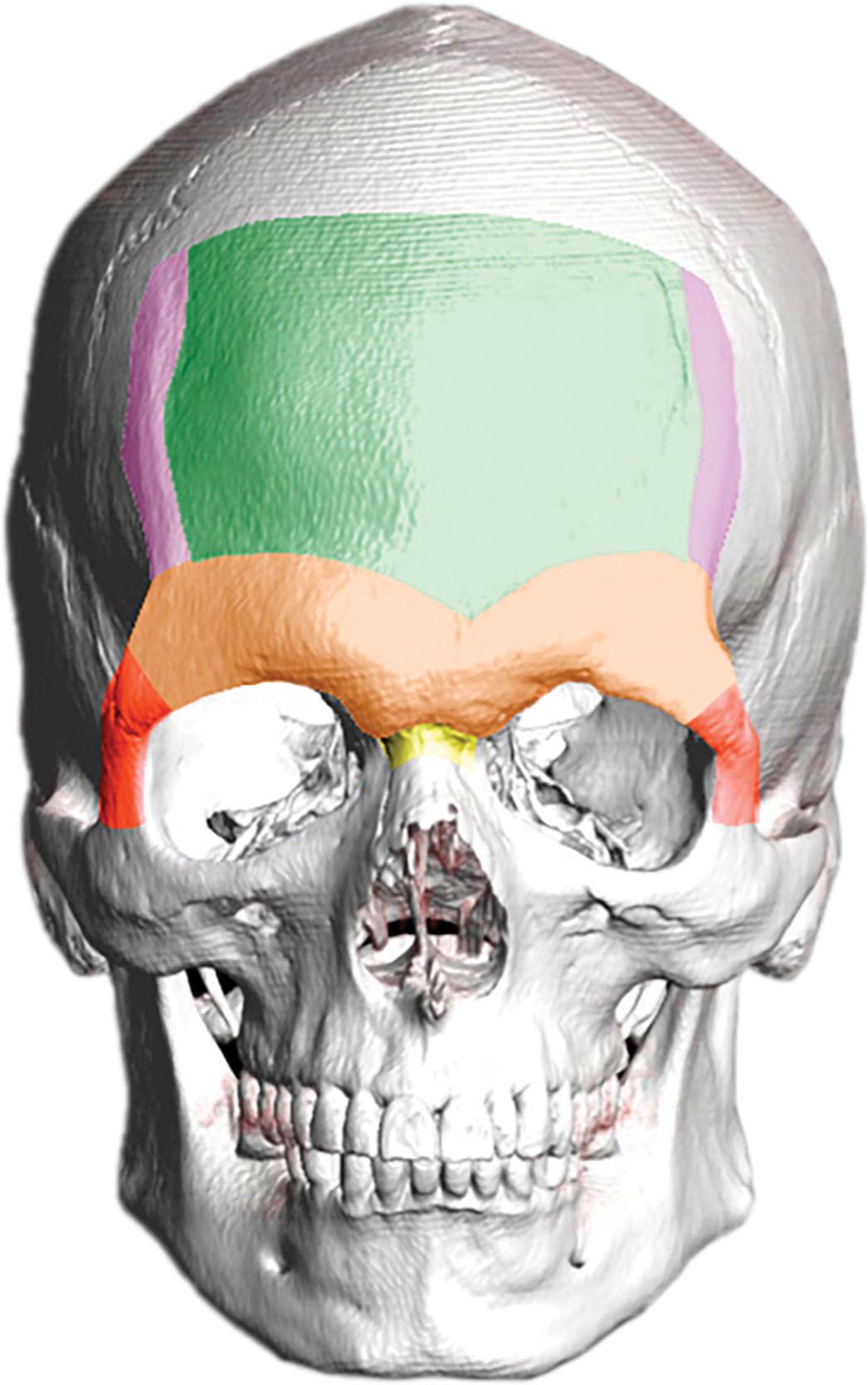
This area is often the greatest determinant of facial gender. The region encompasses the forehead surface, the frontal bossing (the most prominent region of the frontal area) and the supraorbital ridge, the frontomalar buttresses, the temporal ridges, and the frontonasal transition ( Fig. 17.3 ). The supraorbital ridge, which determines the position of the eyebrows and the positioning of the periorbital soft tissues like the eyelids, is almost invariably more strongly developed in the male than in the female. Typically, all the areas are more pronounced and have greater bone volume in the male than in the female skeleton.
The male nose is usually larger than the female because it has a greater mass of bone and cartilage. Female noses tend to be narrower, the tip is often sharper, and the nostrils may be smaller. The frontonasal transition and the nasolabial angle tends to be more acute in males. However, the nose has characteristics conditioned by ethnicity and age that are almost as important as gender-based differences.
As a general rule, the malar bone volume is greater in men, which can result in well-defined cheeks. However, prominent round cheeks are compatible with femininity, due to a greater concentration of fat in this area in women driven by estrogen (i.e., the greater volume is not due to bone). This has specific implications when it comes to deciding the best treatment in this region.
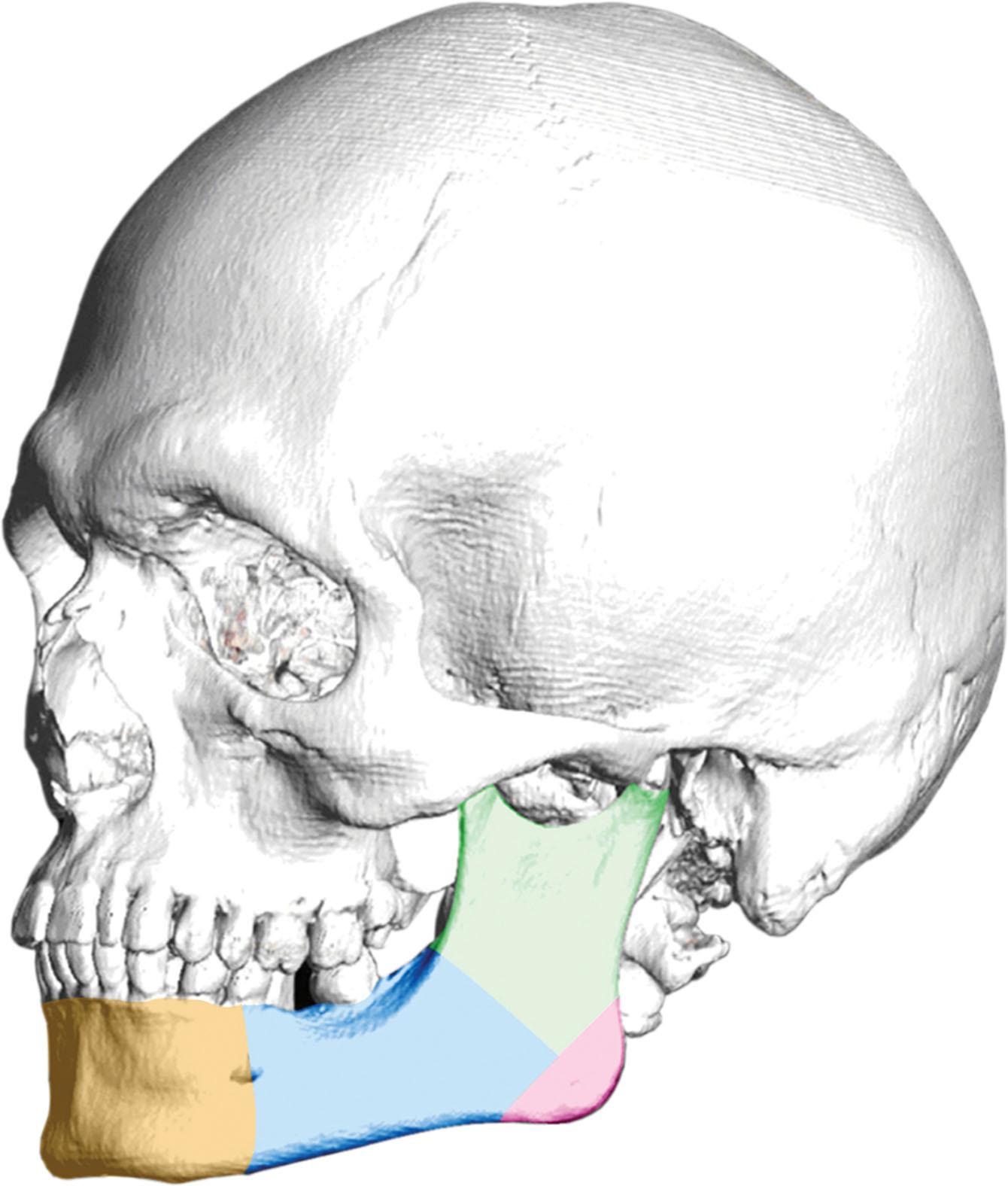
The lower jaw areas to be considered in FGCS are the chin, the mandibular body, the mandibular angles, and the ascending ramus ( Fig. 17.4 ). The male jaw tends to be larger, with greater body height and a broader ascending ramus. The mandibular body typically has greater bone volume in males, which produces a lower facial third that is wider than in women. The mandibular angle formed by the body and ramus tends to be more acute in males, at times with everted gonial angles, and with possible size variance according to the masseter muscle insertions. The male chin tends to be more square-shaped, with more pronounced and defined transitions between the chin and mandibular body, greater bone volume, and vertical height excess.
The larynx structure generally has a greater volume and is larger (greater in diameter and more prominent) in males. The most prominent area of the thyroid cartilage, comprising the laryngeal prominence and nearby structures, is suitable for contouring modification.
In addition to structural facial features, a series of secondary traits are equally important in the identification of facial gender. These include, most notably, the hair and hairline, facial hair and skin texture, and the distribution and volume of facial fat.
When approaching the upper facial third in transfeminine patients, both the anatomy of the fronto-naso-orbital region and the overall condition of the hairline – format, height, and hair density – should be considered as a unit.
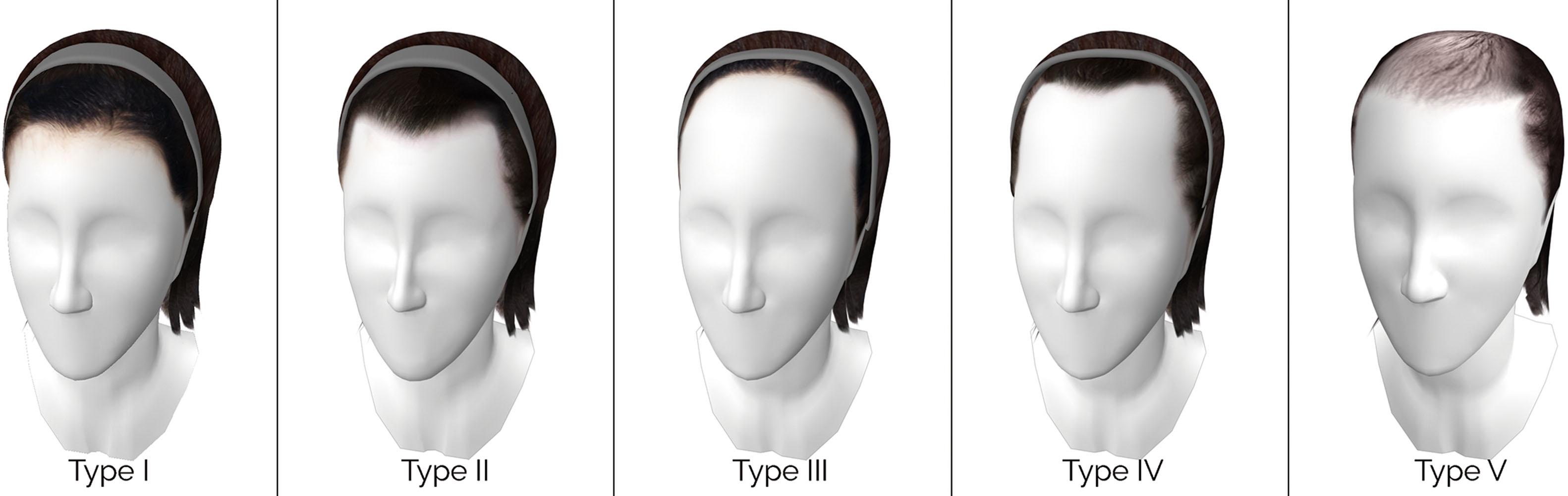
The hairline format can follow different patterns. Male hair may be conditioned by androgenic alopecia (loss of hair due to hormonal influence) and tends to have an M-shaped primary hairline with recessions at the temples. The female hairline usually has a rounded shape, the hair is not normally affected by alopecia and, proportionally, the hairline implantation is higher in the center than with men. Although transfeminine hairlines are comparable to male hairlines, they are distinctive in that alopecia stabilizes as a consequence of HT. The most common patterns found in transfeminine patients are M-shaped (receding hairline at the temples), rounded (without recessions), and undefined (marked front line and temple recessions due to advanced alopecia).
The height of the hairline is the distance between the glabella and the trichion (intersection of the hairline and the middle line of the forehead). For a better clinical analysis and broader understanding, we have implemented a simple measurement tool based on facial analyses done by Hamer to evaluate hairline height: the Lipuhai Rule ( Fig. 17.5 ). This tool can be used to carry out the complementary analysis that should always be part of a thorough clinical case study.
Hair density refers to the number of follicular units (FU) per cm 2 (FU/cm 2 ) on the scalp. Density and the composition of the FU can be easily measured with a simple hand-held device called a densitometer. Additionally, the presence or absence of miniaturization can be assessed with a dermatoscope.
In 2017, we proposed a transfeminine hairline classification based on the observation and analysis of the hairlines of 492 transfeminine patients treated by our group. The analysis established five possible hairline height and format types: type I hairline with normal height and rounded format; type II hairline with normal height and receding hairline at the temples, often called an M-shaped hairline; type III naturally high hairline; type IV high hairline due to alopecia, which is usually associated with a receding hairline at the temples; and type V undefined hairline due to advanced alopecia ( Fig. 17.6 ).
Almost all men have facial hair, which conditions their skin type and quality, making it thicker and rougher.
Women generally have a greater volume of facial fat with a more concentrated pattern in the middle third of the face (malar area).
Since all the secondary aspects can be strongly determined by hormonal influence, they generally respond well to HT. Physical changes that may occur in the scalp and face of transgender females in the first 3–12 months of estrogen and antiandrogen therapy include stabilization of alopecia and/or regrowth of hair, decreased facial hair, softening of skin, decreased oiliness of skin, and redistribution of facial fat. Although a decrease in facial hair growth may be a desired cutaneous change for transgender women on HT, studies have shown that HT alone may not interrupt the growth sufficiently. In light of this, most transgender women seek hair elimination procedures (laser facial hair removal or electrolysis) to achieve more desirable effects. It is therefore preferable to start the treatment of the secondary aspects before beginning structural FGCS (at least 12 months before surgery), so that the changing features do not interfere with a reliable treatment plan ( Fig. 17.7 ).

A detailed preoperative analysis of facial features must take into consideration anthropometric characteristics, age, ethnicity, the harmonic relationship between facial thirds, and factors like the patient’s aesthetic preferences. This requires the use of specific tools:
The entire process of a patient’s facial gender modification should be recorded in photographs, following a clear protocol, including clinical photographs, both pre- and postoperative (preferably in the immediate and long-term postoperative period), and intraoperative photographs of the procedures performed.
In addition to enhancing the clinical documentation process, 3D camera technology makes comprehensive facial analyses possible. Stereophotogrammetry estimates the 3D coordinates of points on a face to yield a volumetric mesh. Beyond merely rendering a 3D image, the technology can also be used to perform anthropometric analyses of facial soft-tissue landmarks with a reliability of <1 mm.
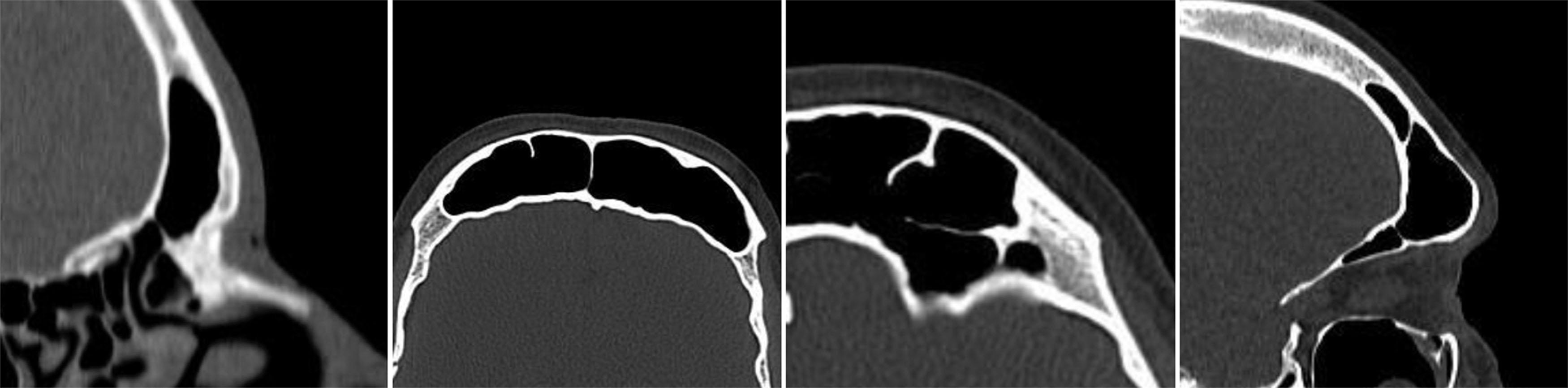
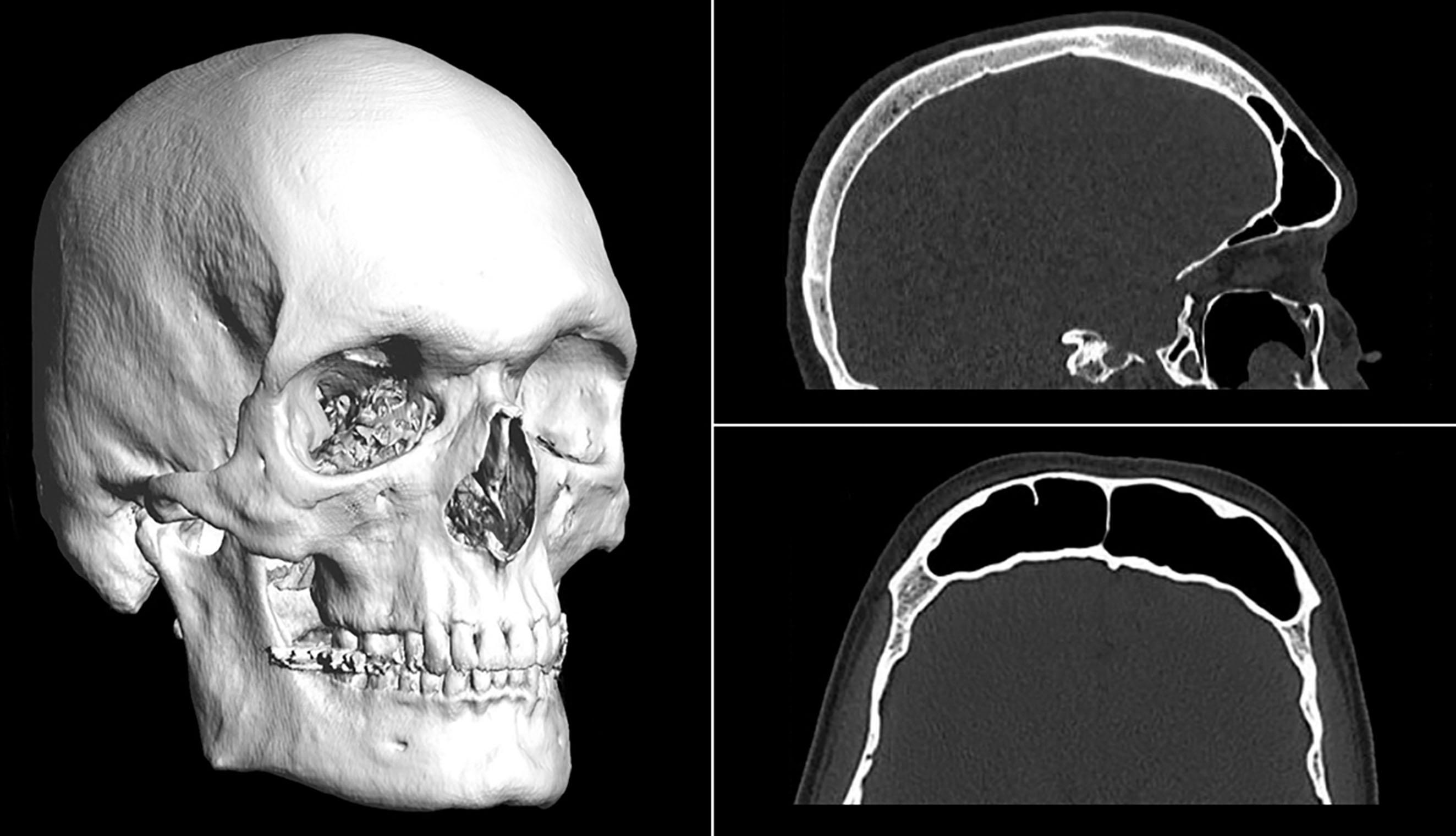
By combining computed tomography (CT) and 3D reconstruction, it is possible to obtain detailed and accurate anatomical information. This is essential when it comes to detecting facial features that can be surgically modified, providing the surgeon with precise information and assisting surgical planning ( Fig. 17.8 ).
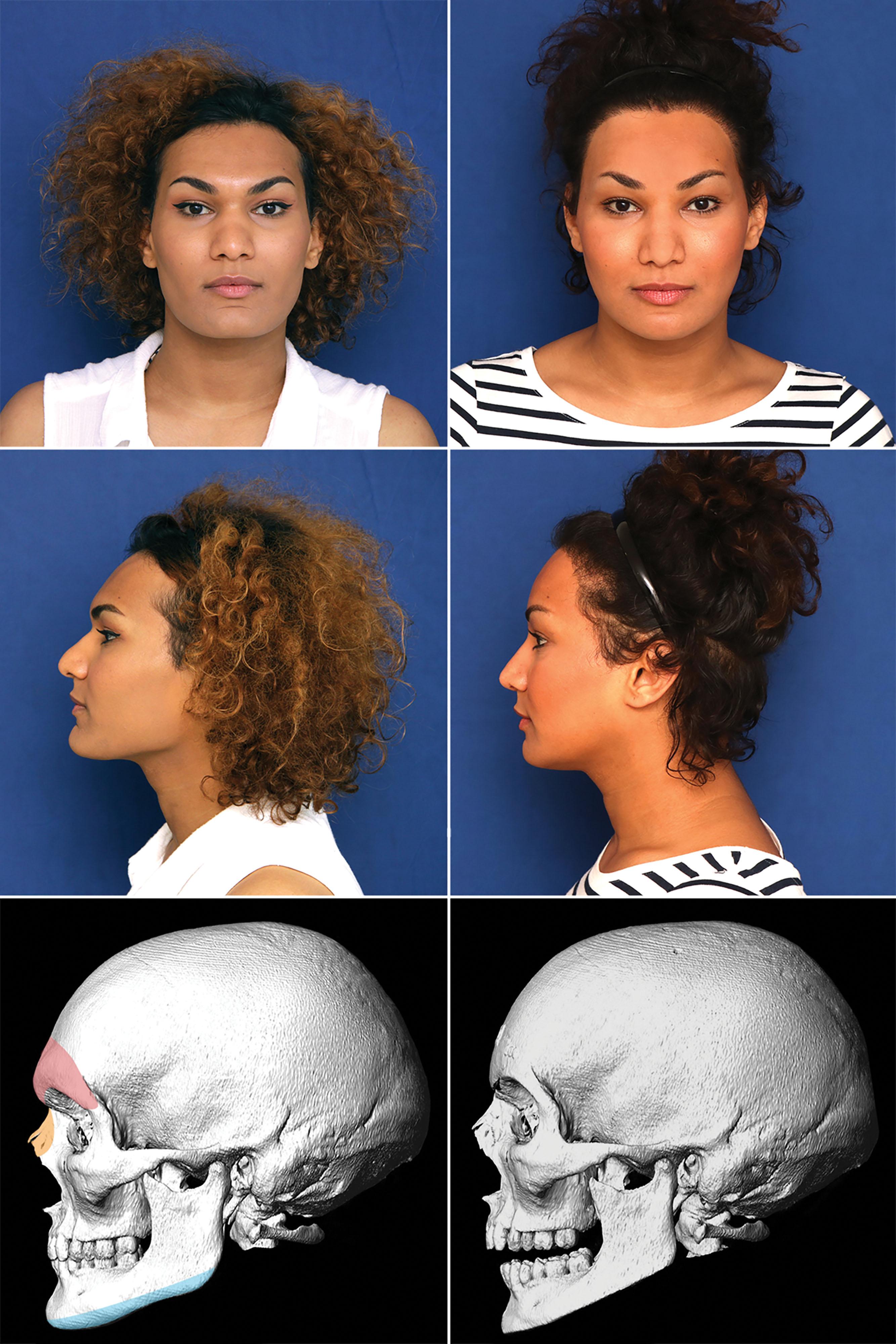
Virtual surgical planning has gained increasing popularity across craniofacial applications including orthognathic surgery, head and neck cancer reconstruction, and pediatric congenital abnormalities. Recently, our surgical group developed a specific planning software for FGCS in conjunction with Software Nemotec S.L. (Nemotec, Biotech Dental, Madrid, Spain). Using this tool, which is integrated into the NemoStudio platform, it is possible to create a lower border-supported cutting guide printed in biocompatible material for use on the day of surgery.
Additionally, the possibility of producing stereolithographic 3D printed models using data from CT images has significantly improved preoperative assessment. In this respect, the standardized incorporation of 3D printing allows for the practice of model surgery, with which surgeons can refine the precise procedures to be performed on the patient on the day of surgery.
Once the elements that make the face masculine have been identified, the indicated surgical procedures are determined. Table 17.1 presents a correlation between the areas into which the face is divided, the features that comprise the areas, and the type or types of procedures that can be used to modify each area. Algorithm 17.1 presents an algorithm of the procedures used in FGCS.
 |
It is critical to listen to and understand the patient’s own views regarding her face. However, patients often have unrealistic ideas about the possible results of their feminization surgery. It is important to explain that the surgery will modify certain features, but that at no time will it modify the core identity of their face or change it completely, since this would go against the principle of naturalness, a core concept of FGCS.
Virtual FFS (VFFS) is an educational tool that simulates the potential results of facial feminization procedures on photographs of the patient ( Fig. 17.9 ). VFFS is highly useful for the diagnostic, planning, and communication phases between specialists and patients. It provides a realistic, reliable approximation of the results and, based on our unpublished observations, can be a significant factor in surgical decision-making. However, the patient should be made aware that, as with all simulations, there is some margin of variability with respect to the results obtained with FGCS in the mid- to long-term. Further studies are necessary to substantiate the validation of this tool and assess how it might be incorporated into predictive software to facilitate its use.

Additionally, regular counseling from a psychologist who specializes in transgender health should be provided throughout the entire FGCS process. During the preoperative period, the patient may present signs of anxiety about the operation. This might be due to fear of pain, fear of anesthesia, high expectations, or uncertainty about how family members and friends may react to the surgery. For that reason, it is important to carry out an initial psychological evaluation to assess the patient’s expectations regarding the surgery, their state of mind, and personal wellness.
While the fronto-naso-orbital complex is one of the main areas that determines the identification of facial gender, the hairline also plays a crucial role in the upper third of the face. The combined evaluation of these two features should be a basic premise of FGCS.
Forehead reconstruction (FR) is one of the basic procedures in facial feminization. It completely modifies the fronto-naso-orbital region and softens and feminizes the patient’s expression. The surgical plan is devised to:
Open the frontonasal angle.
Achieve an adequate backward position of the entire forehead, including the anterior wall of the frontal sinus, while maintaining a harmonic rounded shape.
Open the orbital areas.
Soften the entire forehead surface.
Reposition the eyebrows above the new supraorbital ridge.
If necessary, redefine the hairline via hair transplant as part of the same surgical process.
Although other authors defend different techniques (isolated burring or the use of filling materials), in our experience, the proposed reconstruction technique offers satisfactory and safe results regardless of the anatomy of the frontal region ( Fig. 17.10 ). This method preserves the anatomical integrity of the anterior frontal region, pursues adequate functionality of the frontal sinus, and achieves optimal outcomes (in terms of proper setback), regardless of the preoperative situation.
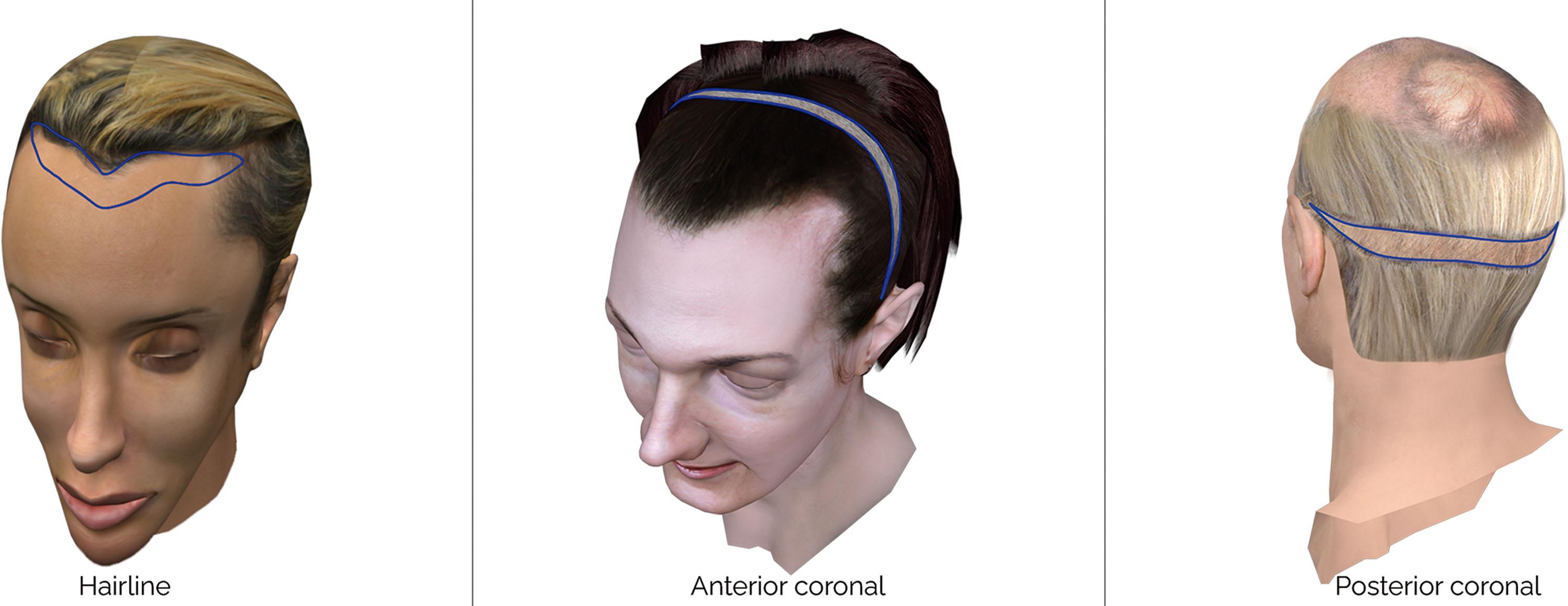
It is essential to discuss the best access (approach route) to reach the frontal bone region: modified coronal approach (anterior or posterior) ( Fig. 17.11 ) or hairline approach ( Fig. 17.12 ). In our opinion, this access should be based on the characteristics of the patient’s hairline and its implantation. The first access route is the modified coronal approach. This modification includes the elimination of an elliptical fragment of the scalp, making it possible to eliminate the excess skin generated after the bone recontouring and allowing for better adaptation of the wound edges, a discrete lifting effect on the forehead and, when necessary, the use of the FU included in this fragment for simultaneous transplantation in the hairline and temporal recessions. In patients with a significantly and disproportionately high hairline (type III transfeminine hairline; see Fig. 17.6 ), the approach can be made through the hairline, where the remaining cutaneous fragment is eliminated to shorten this vertical dimension. For both types of approaches, coronal and hairline, an oblique cutaneous incision with a 35–45º scalpel inclination is recommended. This helps preserve the FU and, after a suitable scarring period, produce hair growth through the scar itself.

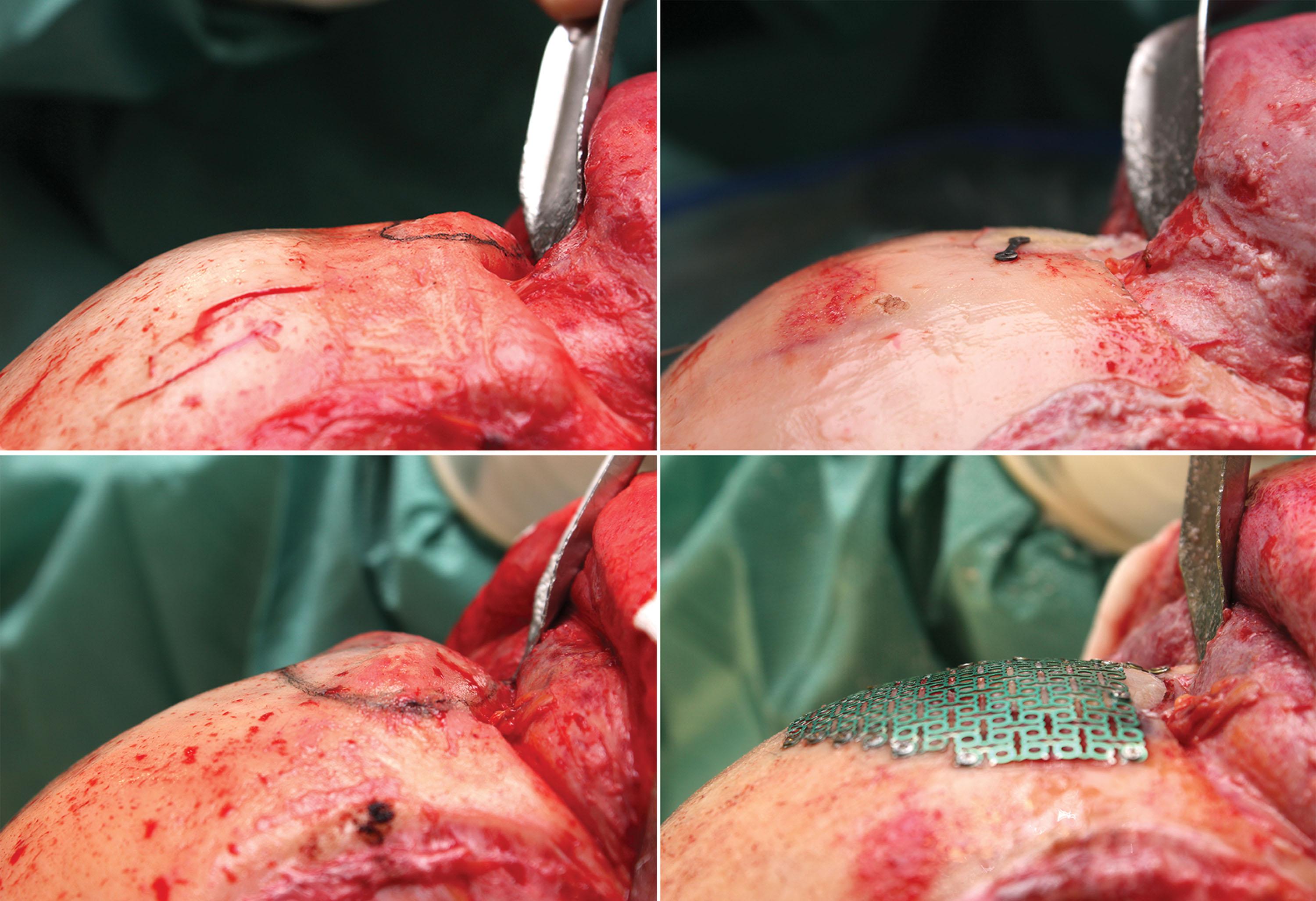
Once the approach route is chosen, during the detachment, anatomical layers are identified to prevent injury to the frontal branch of the facial nerve ( Fig. 17.13 ). Next, a wide pericranial flap is designed with an anterior base that extends to both frontomalar sutures ( Fig. 17.14 ). During this maneuver, it is essential to identify the supraorbital nerves and detach them correctly, which may require osteotomy of the bony rim that separates them from the orbital cavity. In some situations, this detachment may require the use of ultrasonic saw technology. Access is made to the fronto-naso-orbital region, with exposure of the nasal bones ( Fig. 17.15 ).

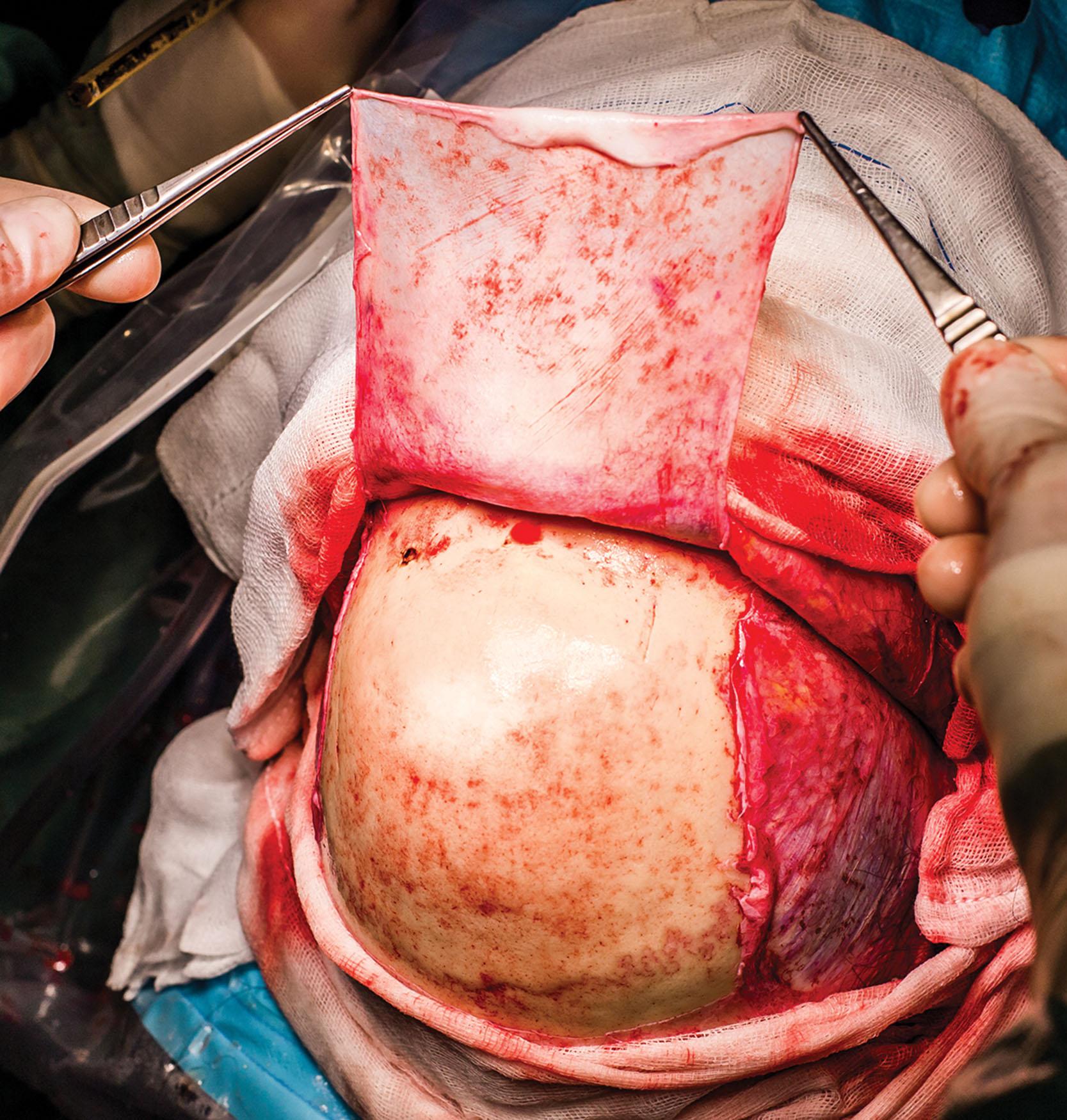
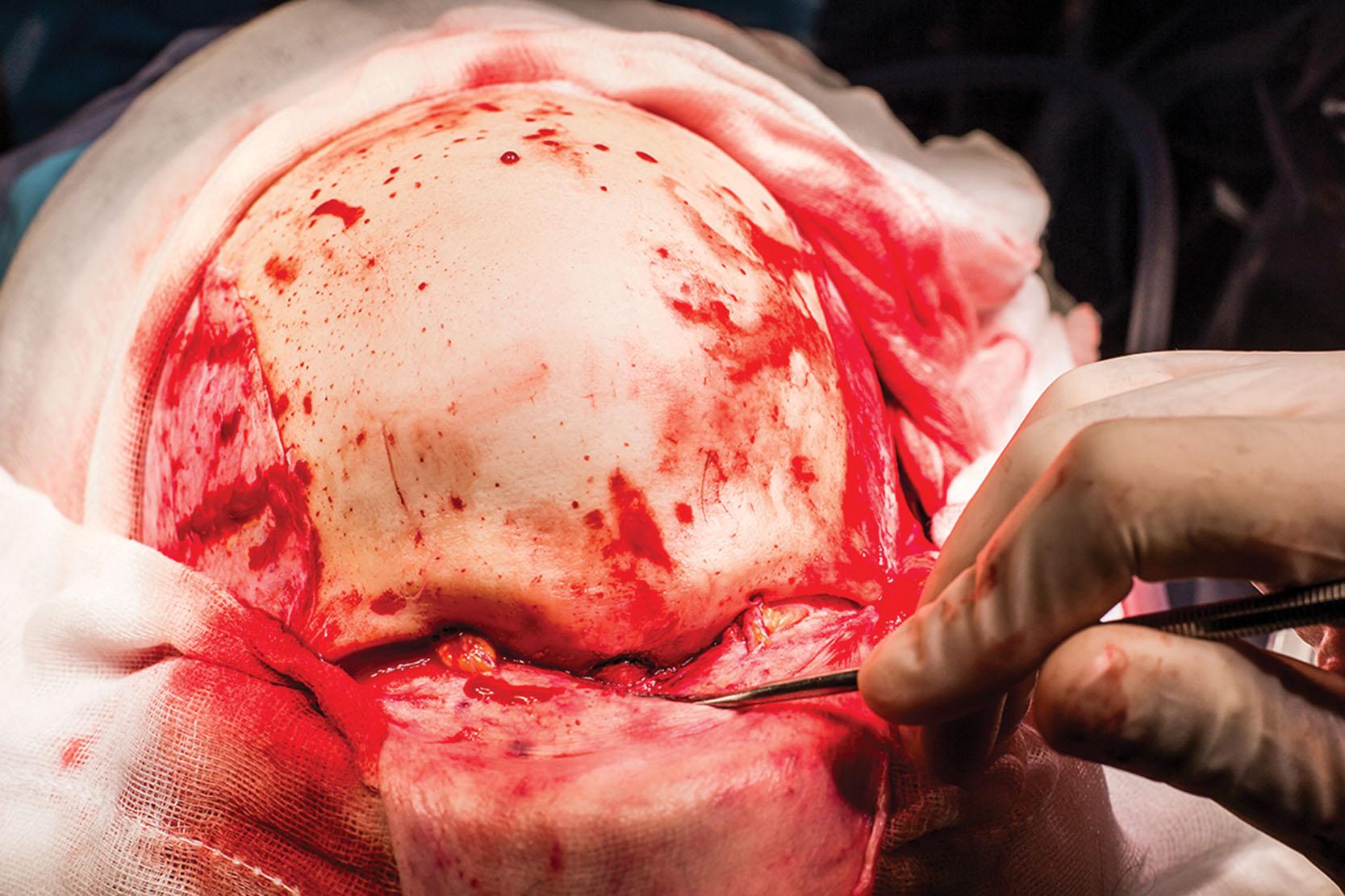
In cases where there is some projection of the upper forehead region, an upper forehead setback procedure by bone shaving can be done prior to the osteotomy of the anterior wall of the frontal sinus. The aim is to make this area as level as possible with the insertion of the nasal bones into the forehead. After the shaving, the retropositioning needed across the entire fronto-orbital ridge will become more evident ( Fig. 17.16 ). With foreheads that are especially square-shaped or have marked temporal ridges, correct exposure and shaving is essential in these areas ( Fig. 17.17 ).
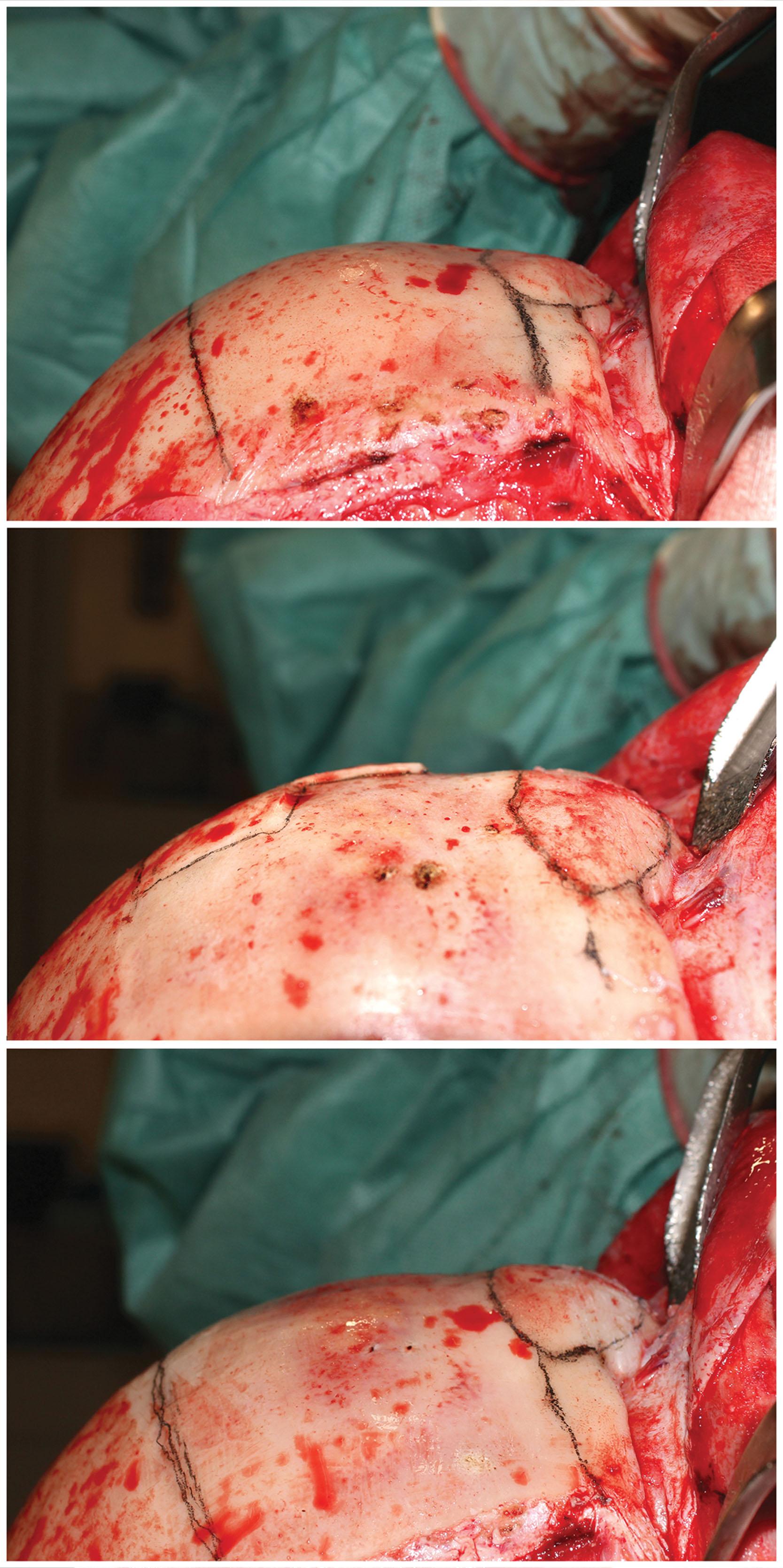
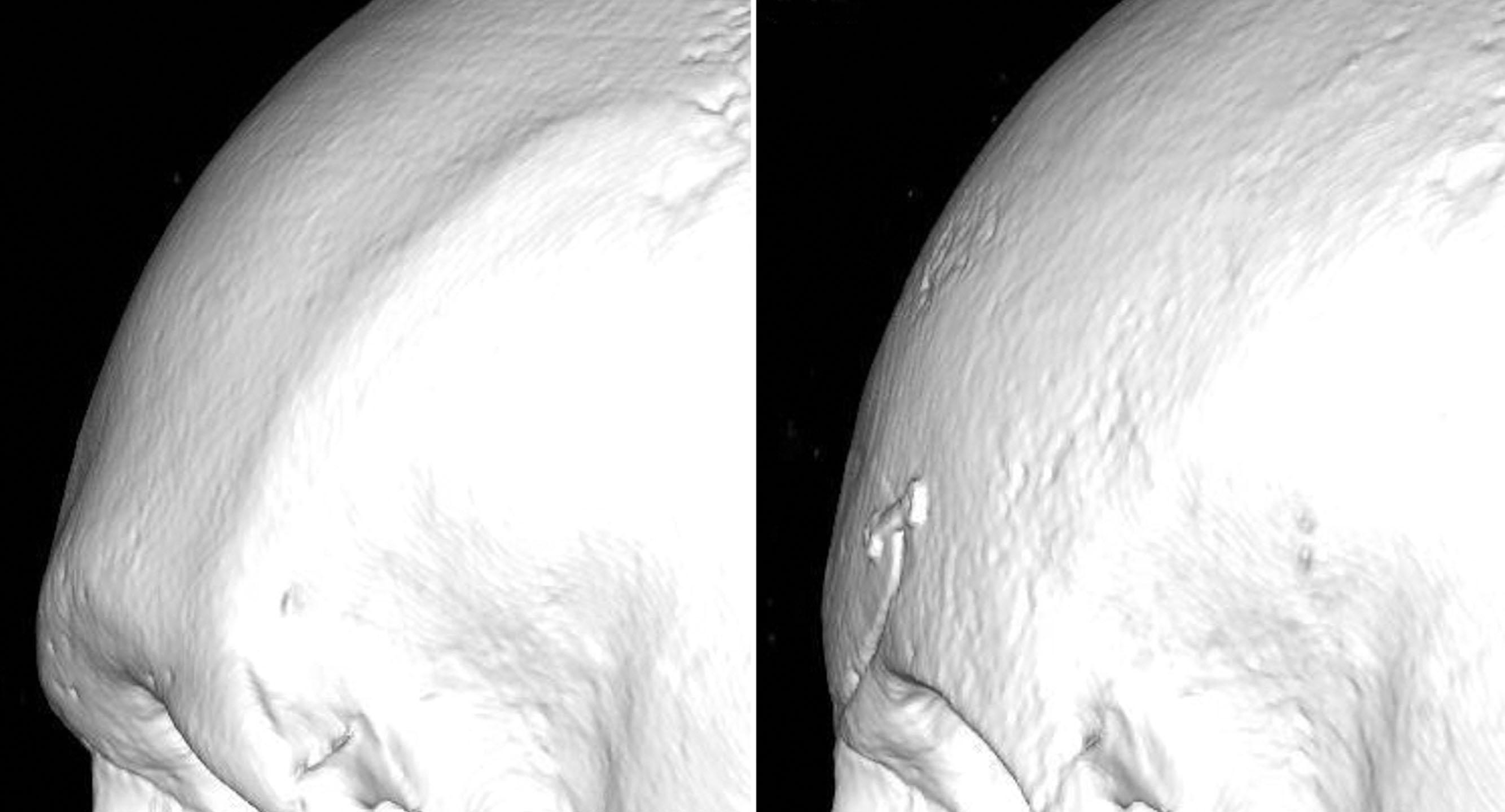
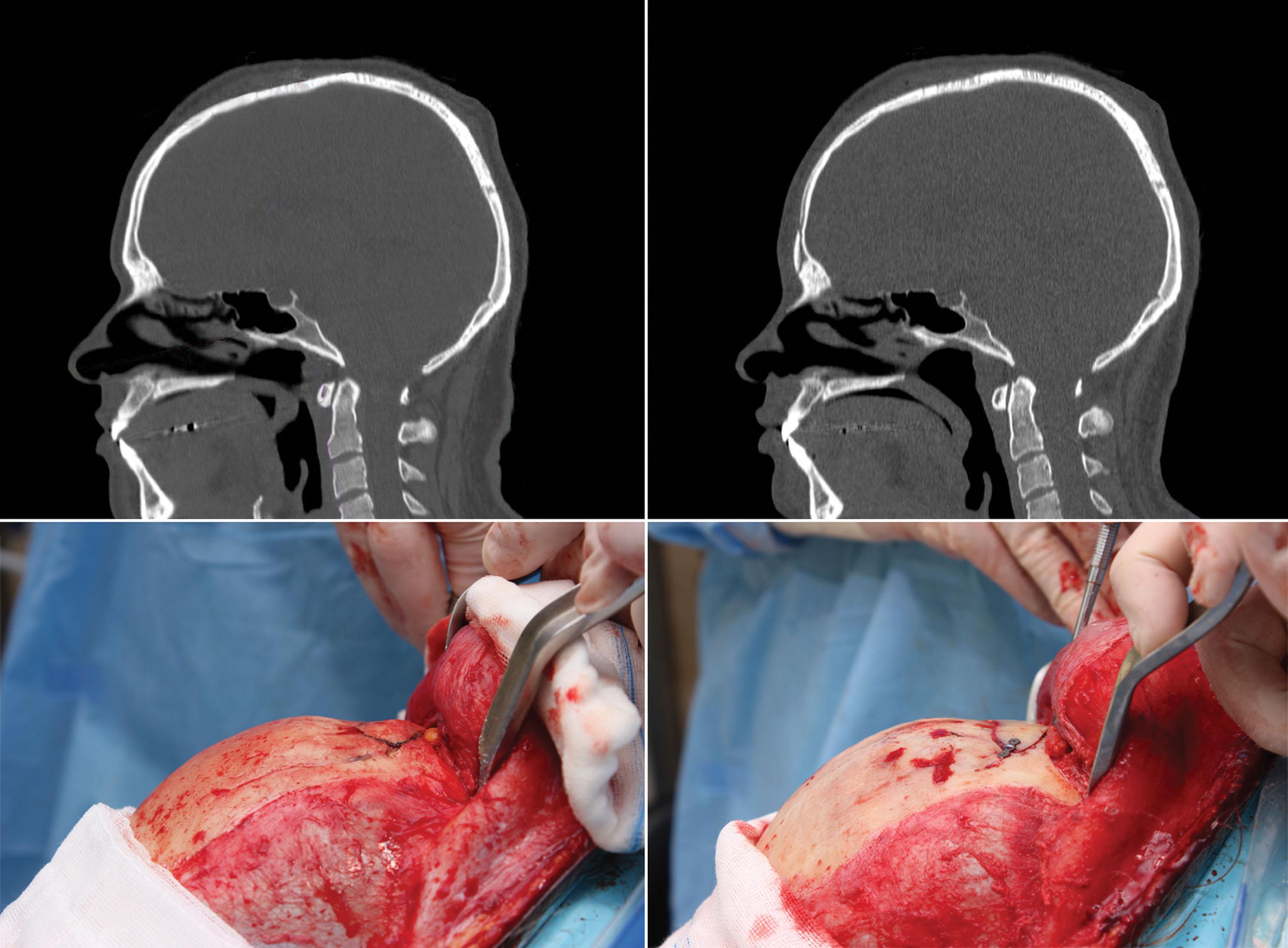
The next step is the osteotomy of the anterior wall of the frontal sinus ( Fig. 17.18 ), which is removed and meticulously sculpted, always taking care to prevent any perforations ( Fig. 17.19 ). This process must take into consideration the anterior wall’s maximum projection, its thickness, the sinus length (cranial–caudal and lateral), the location and characteristics of the posterior wall of the sinus, the frontonasal angle, the location of the orbits with respect to the sinus, the state of the sinus, and the possible absence of a sinus ( Fig. 17.20 ). Most of these anatomical and functional considerations must be analyzed before surgery using a CT study ( Fig. 17.21 ). With access to the sinus secured, the permeability of both frontonasal ducts is ascertained and the undamaged sinus lining preserved ( Fig. 17.22 ).


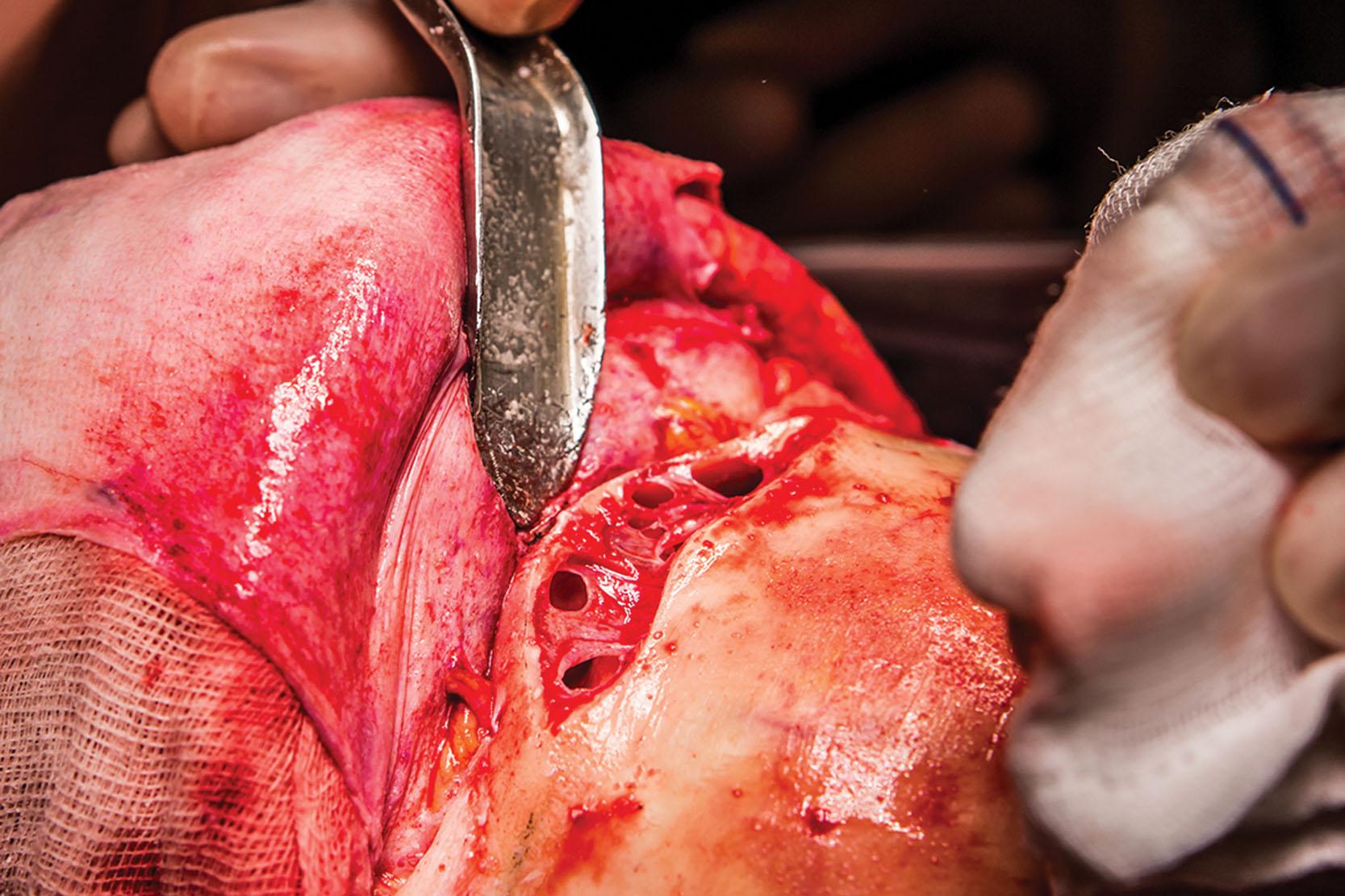
After the osteotomy, the next step involves recontouring the region around the frontal sinus, including the supraorbital ridge and frontonasal transition, levelling the setback as described in step 3.
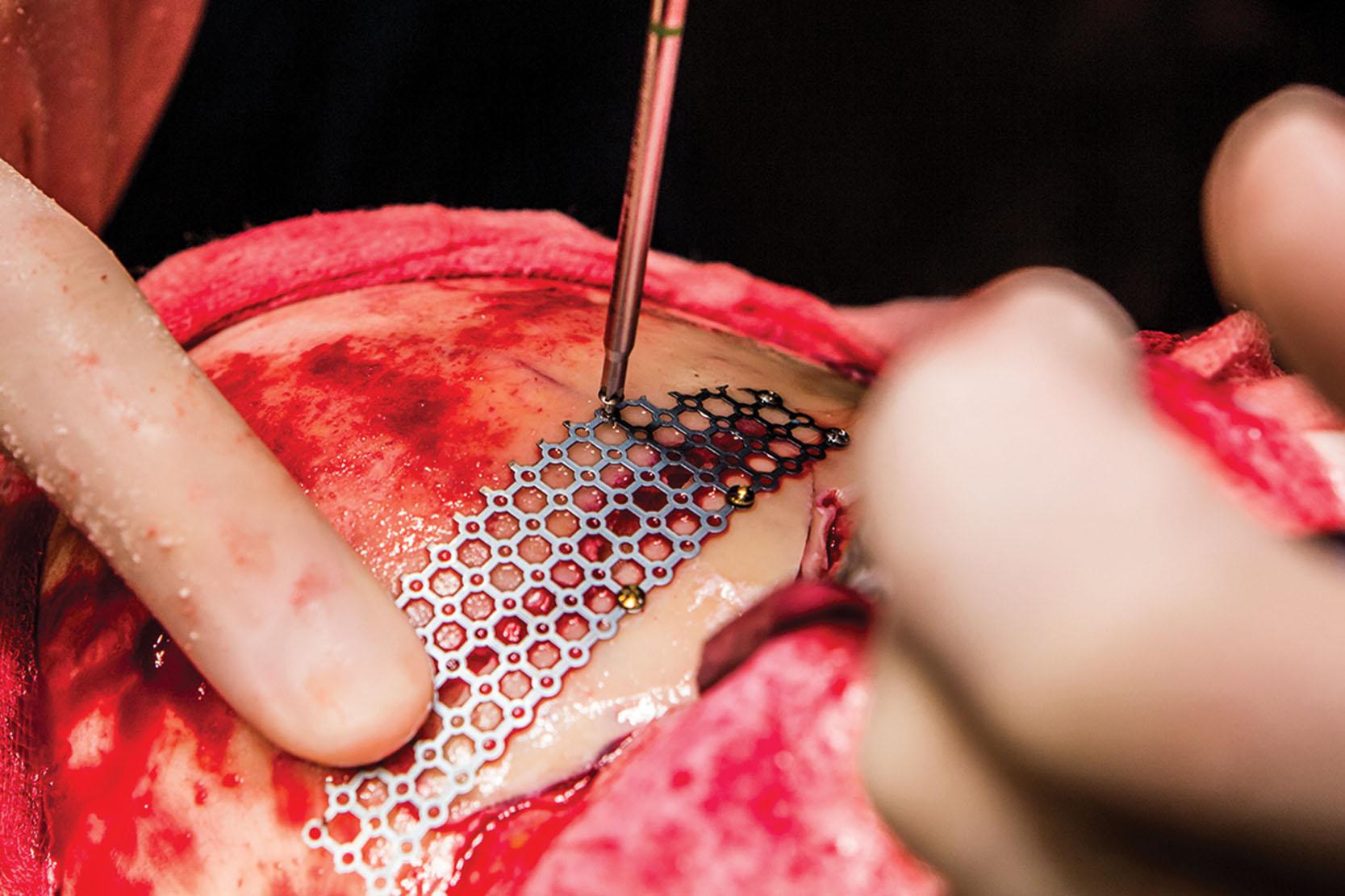
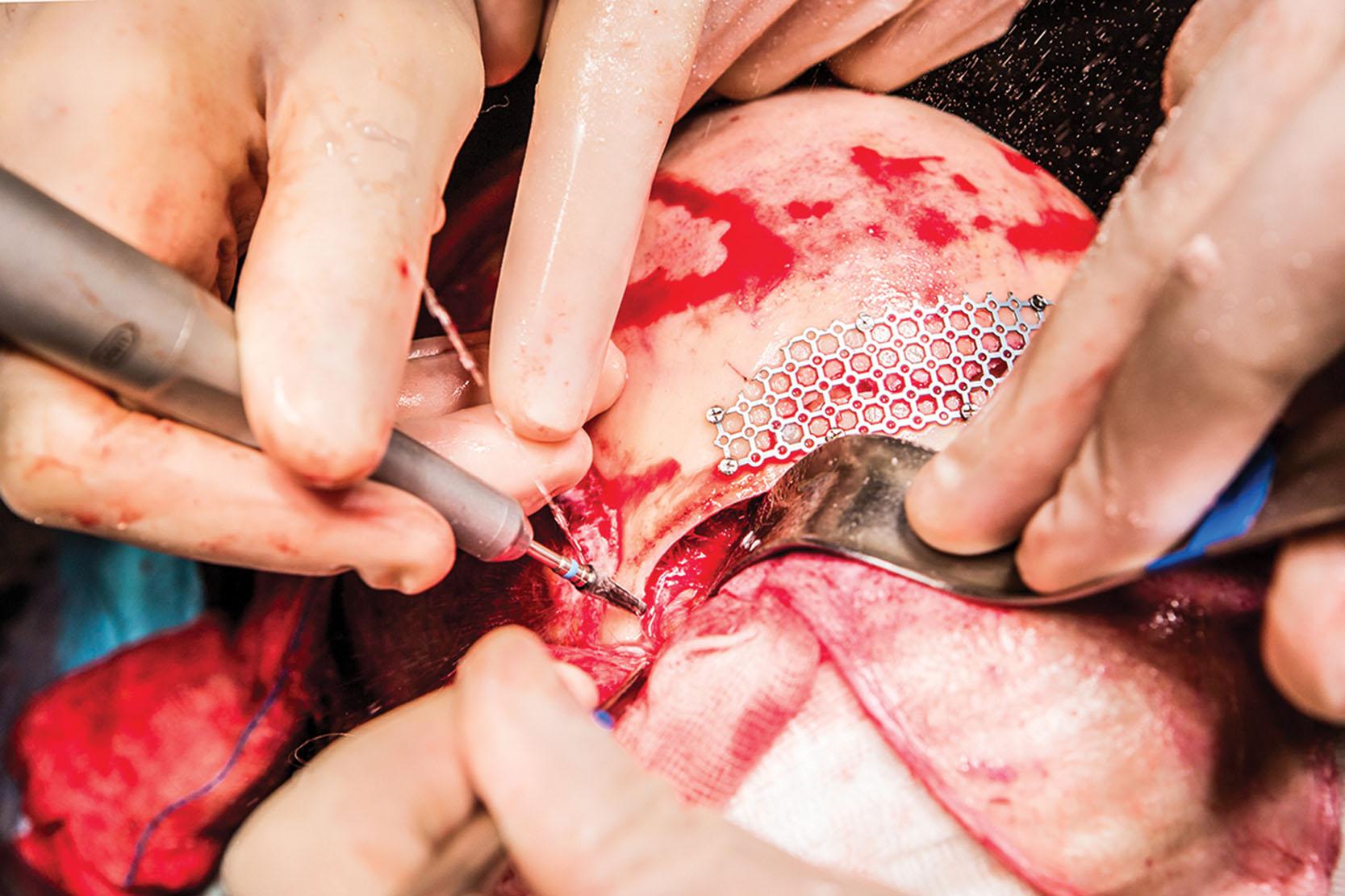
Once all of the recontouring is finished, the anterior wall of the now sculpted frontal sinus is secured using 1.2 osteosynthesis material, either screws or mini-plates, depending on the requirements ( Fig. 17.23 ). This may vary substantially from one case to another according to the sinus characteristics. During this surgical step, properly sealing the sinus is of particular concern, especially in the lower region or closer to the naso-orbital ridge, as is using the correct material to reinforce all the areas with obvious bone gaps that have become excessively weakened after shaving or perforated. In the case of perforation of the anterior wall of the frontal sinus, reconstruction of the defect with a 1.2 titanium mesh is highly recommended ( Fig. 17.24 ).
Once the anterior wall of the frontal sinus has been fixed, the orbits are opened, using a small bone-cutting burr ( Fig. 17.25 ).
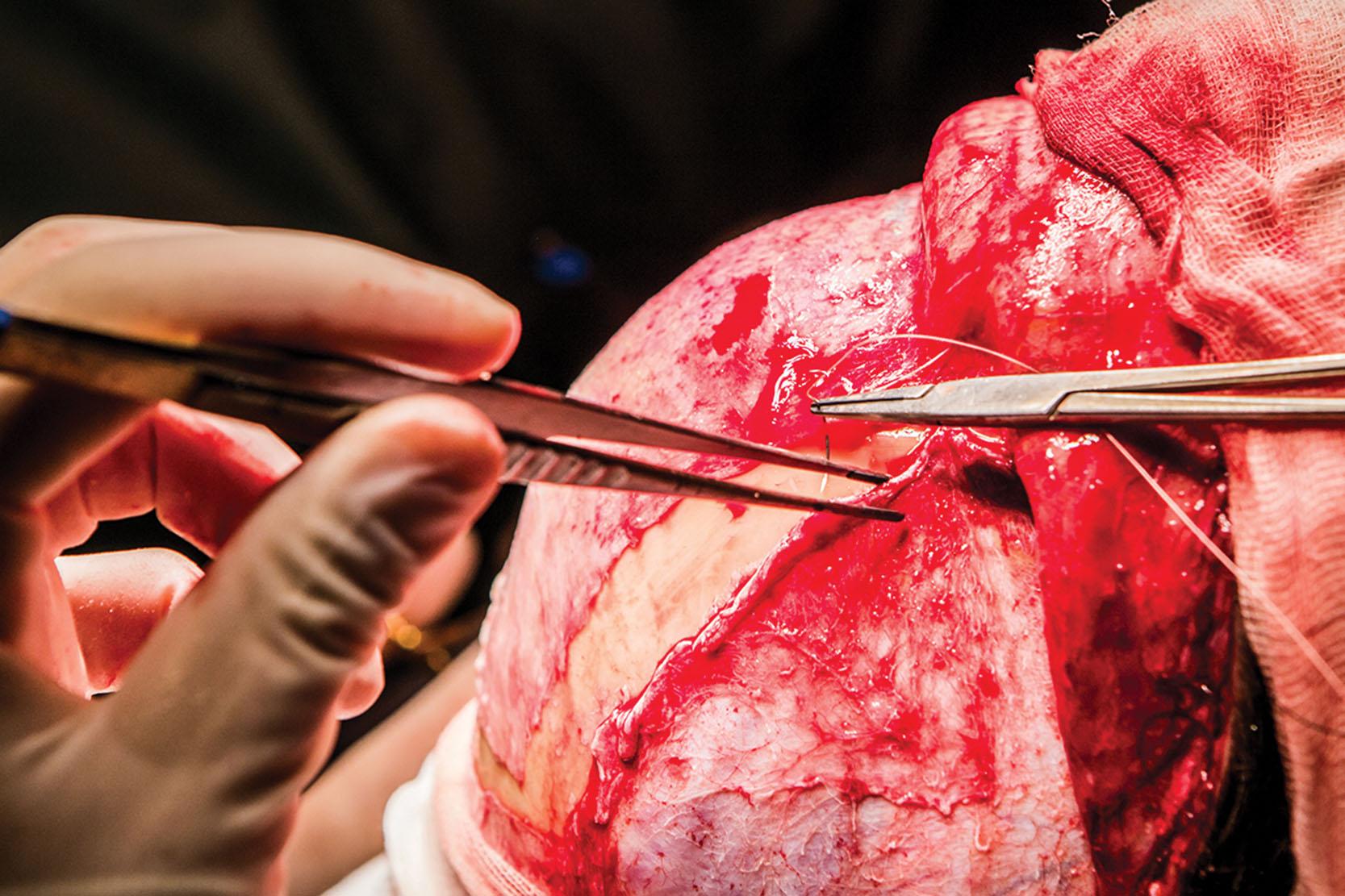
The area is closed in layers, paying special attention to the pericranial flap suture ( Fig. 17.26 ). Whenever a coronal access is used, a drainage device (Redon-type drainage CH-10/3.3 mm, REF. 0028433, Drenofast, Iberhospitex S.A., Barcelona, Spain) is placed that is removed 24–48 hours after surgery.
The hairline is a basic element in the identification of facial gender and, therefore, is often addressed, with the goal of obtaining a satisfactory, natural result.
The main area to treat with a hair transplant is the receding hairline at the temples; however, the central section can also be addressed if the density is poor or if a small advancement (up to 1 cm) of the hairline is desired. This is recommended for patients with an M-shaped hairline, with sufficient hair density, and without active androgenetic alopecia (or with stabilized alopecia due to HT – type II transfeminine hairline; see Fig. 17.6 ). Depending on how the hair follicles are obtained, either follicular unit strip surgery (FUSS) or follicular unit extraction (FUE) can be used:
FUSS – the follicles are obtained from a strip of scalp.
FUE – the follicles are obtained one by one, without any need for an invasive surgical process. This technique usually requires more experience given its technical complexity and generally takes longer.
The new hairline is designed to look natural, paying attention to parameters such as density and unevenness.
The objective of hairline-lowering surgery (HLS) is twofold:
To decrease the overall height of the forehead.
To serve as an access point to reconstruct the fronto-naso-orbital complex (if required).
HLS is recommended for patients with a significantly and disproportionately high hairline (type III transfeminine hairline; see Fig. 17.6 ). A maximum of 2.5 cm of skin is removed and a 2 mm incision (future scar) made above the hairline. Resorbable anchors (Endochor FOREHEAD Lift Mini Device 3.0 mm, Endochor Medical Tibbi Malzemeler TIC. A.S., Türkiye, Istanbul) can be placed to facilitate the advancement and eliminate the tension between the edges of the wound, helping to improve scarring. The lateral extension of the incision is hidden in the hair since advancement in this area is not an objective of the surgery.
In most cases, there are several disadvantages to this technique:
The possibility of leaving a visible scar in a highly exposed part of the face.
The possibility of leaving an excessively short forehead in the center region, which could produce unnatural results.
Potentially limited results if surgical closure of the side temples is attempted due to excessive tension in the scarring area.
In our experience, only 1 out of every 100 patients is a candidate for this type of approach and treatment. However, and despite the almost total lack of relevant bibliographic references, our professional experience suggests that this is the approach most commonly used around the world to treat the hairline in FGCS and may be reflective of a limitation in access to preoperative, intraoperative, or postoperative hair transplantation techniques.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here