Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Although they are relatively rare, tumors that involve the eyelids and orbit are a therapeutic challenge because of the complex anatomy and diversity of pathologic processes that occur in this region. A systematic approach to evaluation and management and a thorough understanding of the pathologic processes of these tumors are required to optimize outcome. Within the eyelid, benign lesions include cutaneous keratosis and papillomas, inclusion and dermoid cysts, and cysts arising from the obstruction of sebaceous and sweat glands. In addition to these lesions, benign sweat gland tumors such as syringomas, myoepitheliomas, and sebaceous adenomas can also occur in the eyelids. The most frequently seen malignant lesions of the eyelids is basal cell carcinoma, accounting for over 90% of all eyelid malignancies, followed by squamous cell carcinomas, sebaceous cell carcinoma, melanomas, Merkel cell carcinomas, and sweat gland carcinomas.
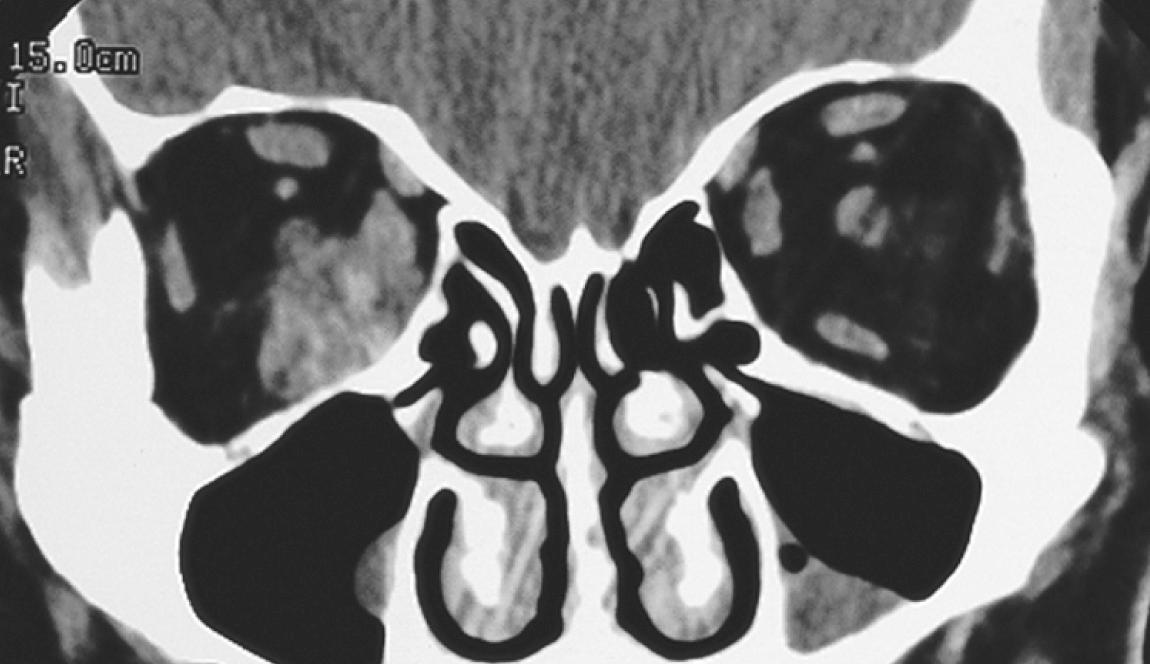
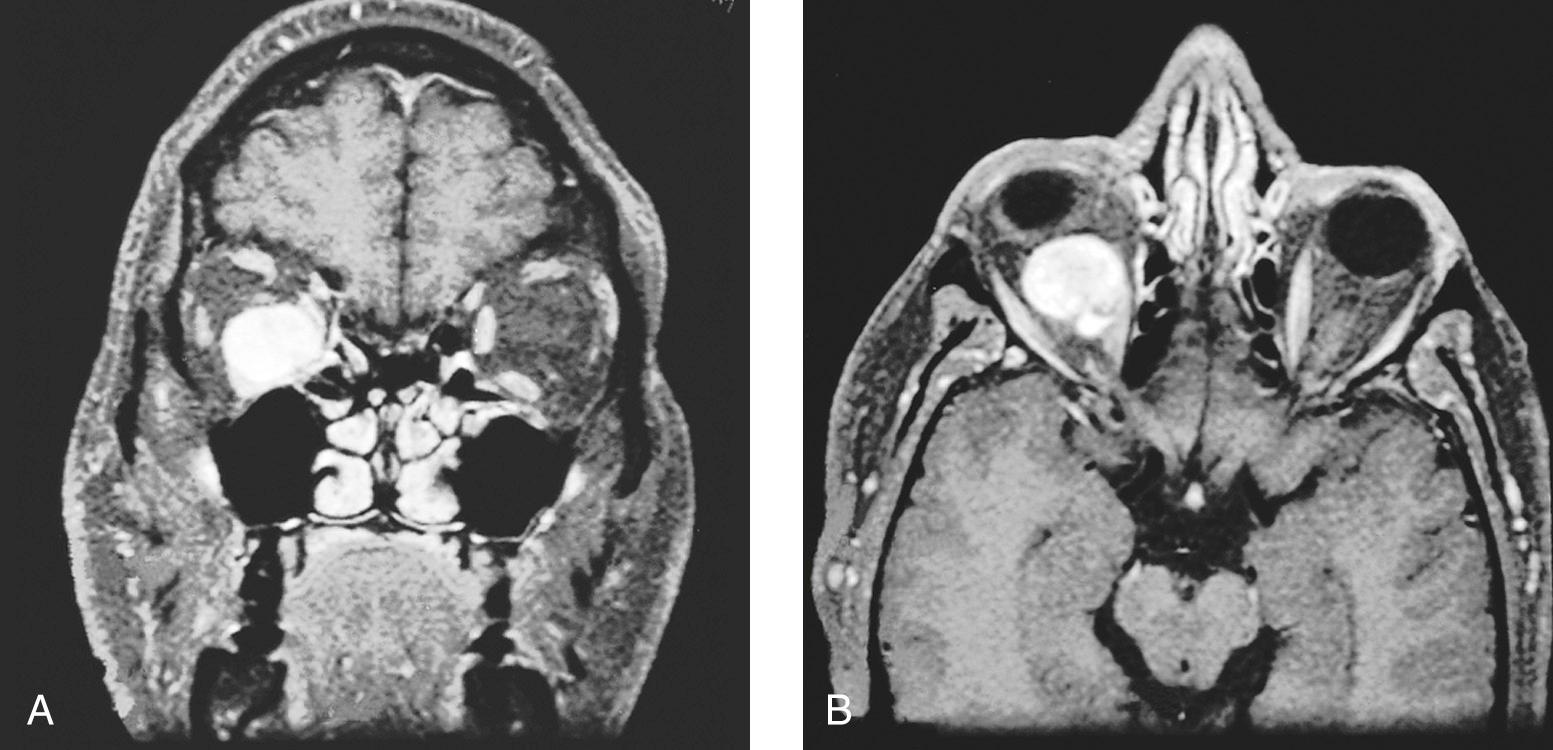
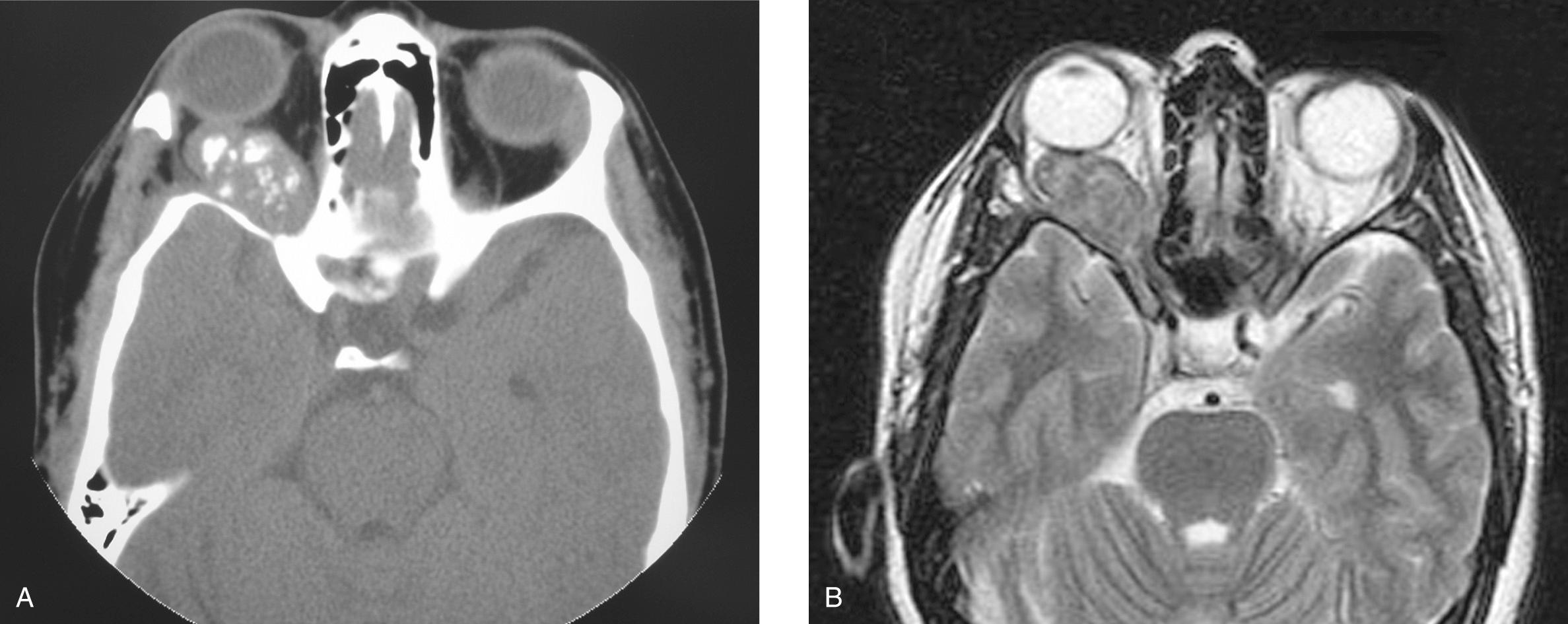
Benign processes represent the most common orbital lesions. An orbital pseudotumor typically presents with eyelid edema, conjunctival chemosis, pain, and rarely visual loss. It sometimes can be misdiagnosed as a neoplasm on the basis of both clinical examination and imaging studies ( Figs. 4.1 and 4.2 ). The most common malignant tumors involving the orbit are extensions of primary tumors from adjacent structures, including the skin, paranasal sinuses, intracranial tumors, and metastasis. Primary malignant orbital tumors represent a small proportion of cases. Despite their rarity, they comprise a wide spectrum of diseases arising from the nerves and nerve sheaths, extraocular muscles, lacrimal gland and lacrimal drainage system, orbital bones, and soft tissues, including lipomas, fibromas, hemangiomas, and their malignant counterparts. The most common primary malignant intraocular tumor is uveal melanoma in adults and retinoblastoma in children, and these can extend into the orbit. Lymphoma and metastatic tumors also can occur in the orbit and need to be included in the differential diagnosis. Clinical examples of some malignant tumors of the eyelid ( Figs. 4.3 through 4.10 ), conjunctiva ( Fig. 4.11 ), and orbit ( Figs. 4.12 through 4.14 ) are shown here.
Evaluation of eyelid and orbital tumors centers on an adequate history and physical examination. Orbital neoplasms may cause changes in appearance (such as lid retraction, entropion, ectropion, ptosis, proptosis, or a change in the position of the globe) or function (e.g., diplopia, blurry vision, or epiphora). Examination should focus on assessment of the position of the lid and globe, as well as their function. Functional examinations should include assessment of the opening and closing of the lid, extraocular movement, globe position, pupillary function, vision, and visual fields. Additional specialized ophthalmic examination may be used to look for change in intraocular pressure (tonometry); the anterior chamber or iris (slit lamp examinations); and the vitreous, retina, or optic disc (funduscopic examinations). The lacrimal system also may be examined to assess for obstruction or involvement of the nasolacrimal duct. In addition, assessment of ocular tumors should include a thorough evaluation of the sinonasal cavity, given the predilection of these tumors for orbital extension.
Radiographic imaging is essential to assess the extent of the tumor within the orbit and extension into the paranasal sinuses, cranial cavity, and infratemporal fossa. A computed tomography (CT) scan is preferred for assessment of bone involvement, whereas magnetic resonance imaging (MRI) is more accurate for defining soft tissue disease and perineural extension. Accurate assessment of invasion of the extraocular muscles, lacrimal gland, or lacrimal drainage system is crucial for surgical treatment planning. The orbital periosteum is a strong barrier to tumor infiltration, and its involvement as demonstrated by imaging studies is an important factor in planning reconstructive surgery to support the globe ( Figs. 4.15 through 4.19 ). A positron emission tomography scan often can demonstrate a clinically occult metastatic tumor in the orbit.


The vast majority of eyelid and orbital lesions (>80%) are inflammatory or benign neoplasms, and identifying the ones that might be malignant often poses a challenge for head and neck surgeons. Familiarity with common benign conditions that can mimic malignancies facilitates identification of malignant processes. In the eyelids, benign conditions such as inflammatory lesions (chalazia), seborrheic keratosis, pilomatrixoma, papillomas, and epidermoid inclusion cysts usually can be differentiated from malignancies by their clinical presentation. Many of these conditions require conservative surgical excision, which can be performed transcutaneously or transconjunctivally, depending on the location of the lesion.
Orbital lesions present a more complex diagnostic conundrum. Because the orbit is a confined space, different lesions in the orbit have similar presentations, including proptosis, chemosis, diplopia, and blurry vision. Imaging sometimes helps differentiate benign from malignant conditions. Idiopathic orbital inflammation, also known as orbital pseudotumors, include a broad category of nonspecific idiopathic inflammatory lesions in the orbit. These tumors can have a diverse clinical presentation, and their diagnosis is based on a combination of clinical, radiologic, and histopathologic findings after careful exclusion of specific systemic and local diseases. True benign neoplasms, including neurogenic tumors and hemangiomas, commonly arise from the lacrimal glands, adnexal structures, and soft tissues of the orbit. The management of these lesions is dictated by size, location, and symptoms.
Basal cell carcinomas (BCC) represent the most common eyelid malignancy, accounting for 90% to 95% of all cases, followed by squamous cell carcinomas (5%–10%) and other malignancies (e.g., sebaceous cell carcinoma, Merkel cell carcinoma, and melanomas). Local progression of these cancers may extend to involve the orbit or globe by direct extension or perineural invasion. Squamous cell carcinomas have a higher risk of orbital invasion compared with BCC. Mohs micrographic surgery is effective in controlling small basal cell carcinoma and superficial squamous cell carcinoma of the eyelids, with local control rates above 95%. Lesions at the medial canthus are often excised incompletely, leading to a high risk for local recurrence. Local recurrence is also more common in squamous cell carcinoma than in basal cell carcinoma, and it occurs in up to a third of patients. Metastasis to the regional lymph nodes from basal cell carcinoma occurs very rarely unless the tumor is large or has recurred multiple times. Squamous cell carcinomas, deeply invasive tumors, and those with perineural invasion also have a higher propensity of spread to the regional lymph nodes. Local recurrence is as high as 30% in sebaceous gland carcinoma of the eyelids due to late diagnosis and skip lesions. As with squamous cell carcinoma, these tumors need assessment of regional lymph nodes and consideration for sentinel lymph node biopsy.
Melanoma of the eyelids is relatively rare compared with basal cell and squamous cell carcinoma. The pathogenesis of cutaneous malignant melanoma of the eyelids involve melanocytes in blue-eyed, fair-skinned persons with a history of sun exposure. Surgical management of melanoma requires wide margin of excision and paraffin confirmation of margins, as frozen section is inaccurate in up to 30% of cases. Outcomes depend on histologic features of Breslow thickness, ulceration, mitotic figures, and perineural or lymphovascular invasion. Lesions that are determined to be a Clark's level IV or greater, Breslow thickness 1.5 mm or more, or greater than AJCC stage T2b are associated with a worse prognosis.
Given the relative abundance of sebaceous glands, it is not surprising that the eyelid is a common site for the development of sebaceous gland carcinomas. These tumors arise from meibomian glands in the tarsus, glands of Zeis in the eyelids, and secretory glands in the caruncle. They can have a varied presentation and often are misdiagnosed, most commonly as a chalazion. Sebaceous gland carcinomas are aggressive neoplasms with a high propensity for pagetoid spread and multifocal involvement with skip areas, making their management quite difficult. Conjunctival involvement is common (in up to 80% of cases) and can be associated with unilateral blepharoconjunctivitis. Lymphatic spread can occur in up to 30% of advanced cases. Local progression can extend onto the bulbar conjunctiva, requiring exenteration of the globe.
Lacrimal gland neoplasms account for 2% to 5% of all orbital tumors. These tumors are equally divided between benign and malignant neoplasms and epithelial and lymphoproliferative lesions. These neoplasms usually present with fullness of the lateral upper eyelid and proptosis and often are palpable. Typically, these symptoms have a limited effect on extraocular movement until the lesion becomes advanced. The most common benign epithelial neoplasms of the lacrimal gland are pleomorphic adenomas. They are similar to salivary tumors in that they can have a heterogeneous radiographic appearance, including the presence of cystic spaces. Adenoid cystic carcinoma is the most common epithelial lacrimal gland cancer, accounting for 30% to 40% of cases, followed by carcinoma ex-pleomorphic adenoma, adenocarcinoma, and mucoepidermoid carcinoma. In general, the behavior of these tumors mimics that seen for corresponding salivary gland cancers. For example, adenoid cystic carcinomas have a high propensity for perineural invasion and metastasis.
The most common primary malignant intraocular neoplasm in adults is uveal melanoma. The highest concentration of melanocytes is in the uveal tract (i.e., the iris, ciliary body, and choroid), which is by far the most common site of origin for primary ocular melanomas. Uveal melanomas may originate from preexisting pigmented lesions, including choroidal nevi and melanosis oculi (nevus of Ota). It has been predicted that 3% of uveal melanoma patients have germline mutations in BRCA -associated protein-1 (BAP1), which comprise a cancer hereditary syndrome that includes mesothelioma, renal cell cancer, and gastric cancer, among others. The choroid is the site of origin for approximately 80% of all uveal tract melanomas, with females typically diagnosed on routine examination and a diagnosis in males being prompted by visual symptoms. These tumors are pigmented, extend into the vitreous cavity, and may show a propensity for growth along nerves, although it can also extend into the sclera and potentially into the orbit. The diagnosis can be made by ophthalmoscopy, and the extent of the tumor can be defined by imaging studies (i.e., ultrasound, CT, and MRI).
Primary intraocular uveal melanomas have a divergent clinical course compared with cutaneous melanomas. These tumors typically spread hematogenously, primarily to the liver. Management of these tumors has been a subject of considerable debate. Two large-scale prospective randomized trials (the Collaborative Ocular Melanoma Study) have compared treatment options for small, medium, and large melanomas. The trial including large choroidal melanomas showed that the addition of preoperative radiation therapy did not improve patient outcome. For medium-sized choroidal melanomas, it was demonstrated that metastatic rates were comparable for I 125 brachytherapy and enucleation, thereby offering an eye-preserving alternative in management. In general, smaller choroidal melanomas are typically observed and treated with plaque brachytherapy if there are signs of growth. Only 2.1% to 2.4% of uveal melanoma patients have radiographic or clinical evidence of distant disease at the time of treatment; however, they carry a significant lifetime risk of systemic disease recurrence. Overall survival ranges from more than 85% for smaller tumors to 70% to 85% for medium-sized tumors and less than 50% for larger tumors, even with aggressive treatment.
Retinoblastoma is the most common primary intraocular malignancy in children, with approximately 5000 cases occurring annually worldwide. Up to 80% of cases of retinoblastoma are diagnosed before the age of 3 years, with 20% to 30% being bilateral. Cone photoreceptors in the retina are thought to be the origin of retinoblastomas. Retinoblastomas typically involve the retina and vitreous, leading to the common presentation of white pupil (leukocoria or loss of red reflex) and strabismus (due to the loss of central vision). Funduscopically, these tumors appear as white to tan lesions and may detach the retina and can be associated with dislodged tumor into the subretinal space or vitreous (“seeds”).
The study of familial retinoblastoma has provided valuable insight into cancer pathogenesis. The landmark “two-hit” model proposed by Knudsen suggests that two genetic events are required for the development of retinoblastoma. In the inherited form of the disease one hit (mutation in the RB1 gene) is present in all cells (germline), and a mutation in the second copy of the RB1 gene is acquired in retinal cells (somatic), leading to their malignant transformation. In contrast, in cases of sporadic retinoblastoma, both hits must occur in a single cell for retinoblastoma to develop. It is for this reason that retinoblastoma develops at a younger age in patients with the inherited form of the disease, with a higher frequency of multifocal and bilateral retinal involvement. The RB1 gene was cloned from children with familial retinoblastoma carrying a deletion at 13q14.2. The Children's Oncology Group version of the International Classification of Retinoblastoma groups eyes into the following categories: A (<3 mm); B (>3 mm or macular or juxtapapillary location or subretinal fluid); C (presence of localized subretinal and/or vitreous seeds less than 6 mm from the tumor); D (presence of diffuse subretinal and/or vitreous seeds greater than 6 mm from the tumor); or E (no visual potential of the globe or the presence of any of the following: tumor in the anterior segment, tumor in or on the ciliary body, neovascular glaucoma, vitreous hemorrhage obscuring the tumor or significant hyphema, phthisical or prephthisical eye, orbital cellulitis-like presentation). The use of systemic chemotherapy has largely been replaced by ophthalmic artery chemosurgery (intraophthalmic arterial chemotherapy), which has the benefit of delivering a high, localized dose to the eye while reducing the complications associated with systemic exposure. Focal treatment including laser and cryotherapy can be used as primary or adjunctive treatments. Familial retinoblastomas often are discovered early. In contrast, most sporadic retinoblastomas (>75%) appear with advanced disease (group E) and often require extensive local treatment or enucleation. In some parts of the world, particularly Asia and Africa, retinoblastoma presents late with extraocular disease extending into the orbit, posing a particular treatment challenge.
Rhabdomyosarcomas are the second most common primary intraorbital tumors in children, typically presenting before the age of 15 years. More than 95% of orbital rhabdomyosarcomas are of the embryonal type (especially the botryoid variant). These tumors manifest as rapidly growing retrobulbar masses that can cause effects on the ocular appearance and function by pressure or direct invasion. The presence of two pathognomonic translocations (t(2;13)(q35;q14) or t(1;13)(p36;q14)), resulting in the formation of oncogenic fusion proteins PAX3-FOXO1 (FKHR) and PAX7-FOXO1 (FKHR), respectively, are present in 80% to 85% of cases of embryonal rhabdomyosarcomas and can be identified by molecular-cytologic analyses. In the past, the outcome of patients with rhabdomyosarcoma was quite poor despite aggressive treatment. The findings from four consecutive Intergroup Rhabdomyosarcoma Study Group (IRSG) cooperative trials have significantly enhanced outcome, especially for patients with locoregionally advanced disease. These trials have helped define a risk-adapted treatment strategy based on the histologic subtype, primary site, extent of disease (International Society of Pediatric Oncology [SIOP] stage, International Union Against Cancer [UICC] stage, or IRSG stage), and extent of resection. All patients with rhabdomyosarcoma require chemotherapy, and surgical excision of the primary tumor is recommended whenever possible if it does not cause major functional or cosmetic deficits. When complete excision of the tumor is not possible, adjuvant radiotherapy is recommended, with the dose modified on the basis of chemotherapeutic treatment response. A 5-year survival rate of more than 70% has been achieved in recent trials for patients with localized rhabdomyosarcoma. However, the outcome for patients with metastatic disease remains poor.
Other tumors of the orbit include those arising from soft tissues and bone such as liposarcomas, malignant schwannomas, hemangiopericytomas, chondrosarcomas, and osteosarcomas. However, these tumors are rare, and the general principles of management are the same as those for such tumors that appear elsewhere in the body.
Invasion of the orbit by local extension from malignancies of the paranasal sinuses, skin, and nasopharynx form the most common malignancies invading the orbit. These tumors include diverse histopathologic entities such as squamous cell carcinomas, minor salivary gland carcinomas, sinonasal undifferentiated tumors, esthesioneuroblastomas, sarcomas, and lymphomas. Management of the orbit in these cases depends on the overall stage of the tumor, the extent of orbital invasion, and available treatment alternatives.
As with other anatomic sites, the treatment of eyelid and orbital neoplasms is dictated by tumor type, location, extent, and patient factors. Although surgery is the mainstay for most primary eyelid malignancies, radiation may be used in select cases. Because radiation in this area can incur a small risk of ocular surface disturbance and potentially corneal ulceration, excision is preferred for amenable tumors. To minimize injury to the cornea, lens, and lacrimal gland, a gold-plated lead eye shield generally is used. However, tungsten eye shields provide better protection from electrons than do lead shields and are preferred. Radiation with a treatment dose of 60 Gy offers excellent local control in more than 90% of patients with cutaneous malignancies of the eyelids. As the size of the lesion increases, the anticipated disfigurement of surgery versus a lower local control rate by radiation should be weighed when deciding on a treatment modality. Larger lesions (>4 cm) are best treated with surgery, sometimes followed by postoperative radiation.
The use of radiation in the periorbital and orbital regions requires special considerations because of the high radiosensitivity of structures in the anterior and posterior chambers of the globe. Radiation planning for orbital tumors always should attempt to exclude the cornea, lens, retina, and pituitary gland. Intensity-modulated radiation therapy or a proton beam plan can help exclude extraorbital normal structures while maintaining therapeutic efficacy.
Both brachytherapy and charged-particle radiation with helium ions or protons have been used effectively to treat uveal melanomas. Brachytherapy delivers a tumoricidal dose of 70 to 100 Gy to the tumor apex. A margin to include the thickness of the sclera (~1 mm) along with an additional 1 mm of tumor thickness is planned. A 2-mm margin surrounding the perimeter of the tumor also is included in the treatment field. The optimal dose rate has not been clearly defined; most treatment is delivered during a period of between 4 and 7 days. More recent experience suggests that the optimal minimal tumor dose rate is likely between 0.7 and 1 Gy per hour using episcleral plaques. The 5- and 10-year local recurrence rates are 11.5% and 15.8%. The efficacy of plaque brachytherapy versus proton beam has not been directly compared, but they are believed to be relatively equal in their efficacy. However, proton beam is superior at controlling peripapillary lesions, although it may result in higher anterior segment toxicity, which is particularly pertinent to ciliary body and anteriorly located tumors.
Surgical treatment planning for excision of malignant lesions of the eyelids must include an appropriate plan for reconstruction of the surgical defect. Most lesions of the upper or lower eyelid can be repaired with use of local tissues. However, more advanced lesions require complex reconstructive procedures. The important issues in reconstructive surgery of the eyelids include prevention of exposure keratopathy resulting from the inability to close the eyelids (lagophthalmos); inadequate drainage of the lacrimal secretions, leading to epiphora; eversion or exposure of the conjunctiva; and impairment of peripheral visual fields because of excessive closure of the palpebral fissure. For more complex reconstructions, the reader is advised to consult more detailed textbooks of oculoplastic surgery. Complex reconstructive procedures are best handled by adequately trained and experienced oculoplastic surgeons.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here