Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Extraanatomic procedures were developed as alternatives to direct aortofemoral bypass for patients deemed to be at high risk for direct aortic surgery or for those presenting with a “hostile” abdomen, an infection of the native aortoiliac arterial system, or prior prosthetic replacement of the aortoiliac system. The first extraanatomic procedure to be described for treatment of aortoiliac occlusive disease was the femoral-femoral bypass, which was first reported by Freeman in 1952. In 1962 Vetto provided the first comprehensive description of a significant number of cases with an analysis of clinical outcomes. Axillofemoral bypass was first reported by Blaisdell and Louw in 1963, and by 1968 growing experience supported this option as a safe alternative to direct aortic reconstruction. The feasability of thoracofemoral bypass was first reported in 1961, but it was not until the 1980s and 1990s that retrospective reviews reported long-term outcomes for patients treated with this approach. Balloon thromboembolectomy was introduced by Fogarty and colleagues in 1963, with reports of its utility for treatment of aortoiliac embolism appearing soon thereafter.
Prophylactic antibiotics. Extraanatomic bypass is nearly always performed with prosthetic material, either expanded polytetrafluoroethylene (ePTFE) or polyester. Infection of these grafts is associated with a high risk of loss of life or limb. Thus preexisting infection should be treated to the extent possible before placing the grafts, and antibiotics administered to reduce the risk of secondary graft infection.
Risk assessment. Cardiac, pulmonary, and renal function should be assessed and optimized.
Emergent or urgent intervention. Arterial embolectomy is implicitly an urgent or emergent procedure in most cases, so preoperative care is usually limited to volume resuscitation, transfusion, and other measures to optimize organ function. Mortality related to arterial embolectomy remains high, due to advanced age and associated comorbidities, particularly cardiac disease.
Injury to the axillary and subclavian arteries, veins, and brachial plexus. The axillosubclavian artery is characteristically less robust than the femoral artery, and injury from dissection, clamp placement, or sutures tearing through the artery is more likely. Injury could conceivably require transection of the clavicle, sternotomy, or thoracotomy to facilitate repair. The axillary artery and vein and brachial plexus may also be injured during tunneling of the axillofemoral graft.
Disruption of the axillary artery anastomosis. The axillary artery anastomosis should be placed as medial (adjacent to the clavicle) as possible and to allow some redundancy in the axillary end of the axillofemoral graft. This will minimize the risk of “axillary pullout,” or disruption of the axillary anastomosis with arm abduction. The axillofemoral graft should also be placed in the midaxillary line to reduce the risk of kinking during torso flexion.
Bladder or bowel injury. Bladder or bowel injury is possible when tunneling a femoral-femoral graft if the graft is placed in the retrofascial space or if the patient has a suprapubic hernia, particularly if there has been previous surgery in this area.
Iatrogenic injury during embolectomy. Embolectomy leads to arterial perforation, rupture, and dissection. The catheter should not be “forced” when advancing it, (i.e., if the catheter meets with resistance, it should be withdrawn a significant distance and then readvanced and rotated somewhat to try to “give a different look” to the catheter tip). The surgeon must learn to get tactile information from both hands, (i.e., a sense of resistance when advancing the catheter and drag on the catheter when withdrawing with the balloon inflated), and a sense of the resistance to inflation using the syringe. Pulling back on an overinflated balloon can do irreparable damage in the short term and produces significant vasospasm, particularly in the infrapopliteal arteries.
Femoral-femoral bypass depends on the ability of one “donor” iliac artery to supply enough blood flow to perfuse both the donor and the “recipient” legs ( Fig. 29-1 ). Oblique, groin-crease incisions may be used, but longitudinal groin incisions centered over the femoral arteries and beginning approximately at the inguinal ligament provide the most flexibility and are preferred by most surgeons. Incision length depends on patient habitus. Anastomoses to the common femoral artery may extend onto the deep or superficial femoral artery and may occasionally be made directly to the deep or superficial femoral arteries. This decision is most often made after exposure, inspection, and palpation of the femoral arteries, but it is also predicted by complete preoperative imaging. The extent of dissection to control femoral arteries and the use of vascular clamps, silicone elastomer (Silastic) vessel loops, or occasionally balloon catheters are dictated by the site of anastomosis, surgeon preference, and whether there has been previous surgical exposure of the femoral arteries.
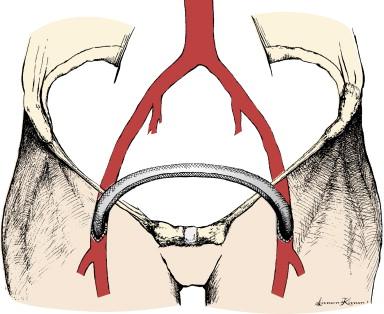
Most femoral-femoral grafts are placed in the immediately prefascial subcutaneous position. The tunnel should begin in line with the planned arteriotomy to be used for anastomosis and should be made in a continuous arc, avoiding abrupt right-angle turns to reduce the risk of graft kinking and subsequent thrombosis. The tunnel can be made bluntly with index fingers from both sides, with fingers meeting in the midline. A large clamp, such as a curved DeBakey aortic clamp, or uterine packing forceps may be used to complete the tunnel, but the surgeon must be careful not to perforate the fascia or a hollow viscus in an unsuspected hernia. The same clamp may be used to pull the graft from one side to the other, taking care that the graft does not twist during passage. Some surgeons prefer larger-diameter grafts, but there is no evidence that grafts larger than 6 mm in diameter perform better hemodynamically or that patency is improved with larger-diameter grafts. A 6-mm-diameter, externally supported ePTFE graft is an acceptable choice, but there is also no evidence that external support or the use of ePTFE as opposed to polyester is associated with better outcomes.
Systemic heparin or another suitable anticoagulant is administered, and in most cases a longitudinally oriented or slightly oblique arteriotomy is created in a convenient place for anastomosis. Making the anastomosis on a more distal portion of the femoral system, such as the deep or superficial femoral artery, may be dictated by local anatomy and may reduce the tendency of the graft to kink in the sagittal plane in patients with protuberant abdomens. As with most end-to-side anastomoses, arteriotomies are made about three times as long as the graft diameter. The graft ends are spatulated by placing a curved hemostat on the graft and then using a scalpel to cut the ePTFE graft along the inside of the hemostat curve. An end-to-side graft to artery anastomosis is then created using running 5-0 or 6-0 polypropylene or CV-5 or CV-6 polytetrafluoroethylene (PTFE) suture. The donor-side anastomosis is usually performed first, although either side may be completed first and the anastomoses may be performed simultaneously if there are two surgeons. For at least one anastomosis, preferably the recipient side, the suture is not tied to complete the anastomosis until the clamps and vessel loops have been briefly released to fill the graft with blood and to allow expulsion of air and thrombus or other debris.
A sterile, handheld continuous wave Doppler probe is used to interrogate outflow on both donor and recipient sides and to ensure that flow is qualitatively better on the recipient side, as evident by a higher Doppler frequency shift, with the graft open than with the graft clamped. Anticoagulant may then be reversed, the wounds may be closed with running subcutaneous absorbable suture, and the skin may be closed with staples in most cases.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here