Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
A spinal deformity is an abnormality of the alignment, formation, or shape of the spinal column. Traditionally, spinal deformities have been classified into those that predominantly affect the coronal plane (e.g., idiopathic scoliosis) and the sagittal plane (e.g., Scheuermann kyphosis). In reality, spinal deformities are complex and simultaneously affect the sagittal, coronal, and axial plane alignment of the spinal column, and its relationship to the pelvis and thoracic cage. A spinal deformity may result from a pathologic process at a single vertebra level (e.g., spondylolisthesis), or multiple spinal levels (e.g., Scheuermann kyphosis), or it may involve the entire spinal column and pelvis due to compromised postural support mechanisms (e.g., neuromuscular scoliosis).
Multiple facets of human disease may be associated with a spinal deformity depending on its etiology. A spinal deformity may be only one manifestation of an underlying systemic disorder that may affect multiple organ systems. The etiology of spinal deformities is wide ranging and includes congenital, developmental, degenerative, neuromuscular and metabolic disorders, trauma, infection, tumors, and conditions whose precise etiology remains incompletely defined (e.g., idiopathic scoliosis). Radiographs are required to document the presence, severity, and extent of a specific spinal deformity. Higher-level imaging studies (computed tomography, magnetic resonance imaging [MRI]) are used to evaluate neural compression, anatomic detail, and to rule out the presence of coexisting intraspinal anomalies, and anomalies involving other body systems.
The consequences of an untreated spinal deformity for a specific patient depend on many factors, including age, underlying health status, etiology, deformity magnitude and pattern, and the potential for future progression of the spinal deformity. Potential consequences of untreated spinal deformity may include cosmetic issues, pain, neurologic deficit, sagittal and/or coronal plane imbalance, and impairment in activities of daily living. Severe thoracic deformity may impair respiratory mechanics with resultant hypoxemia, pulmonary hypertension, cor pulmonale, or even death.
Detailed history:
What is the presenting or chief complaint (e.g., deformity, pain, neurologic symptoms, impaired function in activities of daily living, cardiorespiratory symptoms)?
If pain is present, describe its location, severity, duration, frequency, and whether it is present during activity or at rest.
When was the spinal deformity first noticed?
Is the spinal deformity progressing in severity?
For pediatric patients: What is the patient’s maturity and growth potential?
Past medical history: Have prior spine treatments or diagnostic studies been performed? Are there any associated or general medical problems? Were there any abnormalities noted at birth or during development?
Medications: include dose, route and frequency for each medication
Allergies: include allergies to medication and nonmedication substances, such as iodine or shellfish
Review of Systems
Family history: Is there a family history of spinal deformity?
Social history: occupation, history of tobacco and alcohol use, or drug abuse
Comprehensive physical examination:
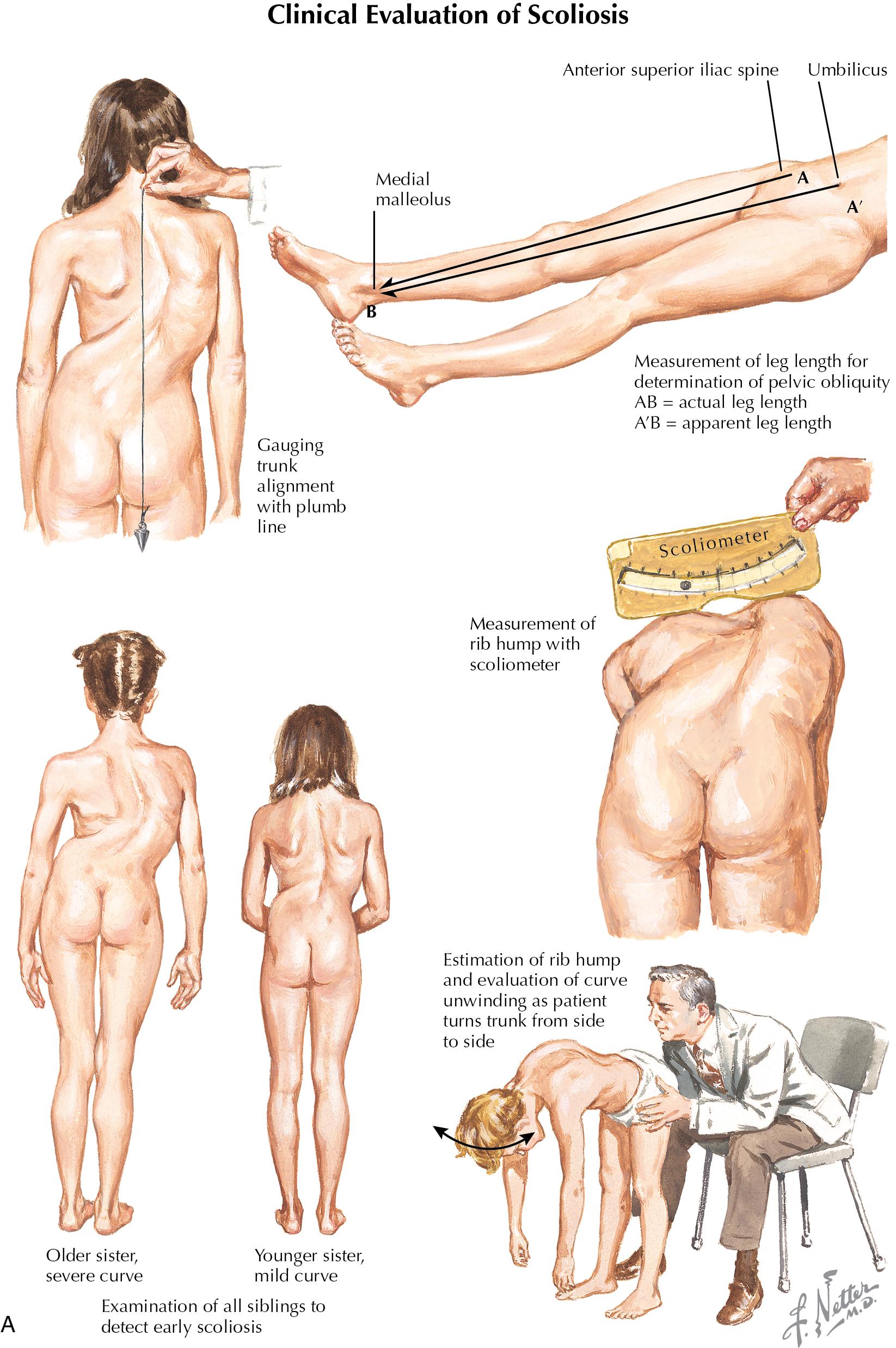
Inspection. The patient must undress and change into a gown so the examiner can fully assess the trunk and extremities. Assess for asymmetry of the neckline, shoulder height, rib cage, waistline, flank, pelvis, and lower extremities. The patient is initially assessed in the standing position and next is bent forward to 90°. The patient should be inspected from both anterior and posterior aspects, and from the side. Note any skin lesions (e.g., midline hair patch, sinus tract, hemangiomas, café au lait pigmentation). Observe the patient’s gait. Observe body proportions and height.
Palpation. Palpate the spinous processes and paraspinous region for tenderness, deviation in spinous process alignment, or a palpable step-off deformity.
Spinal range of motion. Test flexion-extension, side-bending, and rotation. Any restriction or asymmetry with range of motion (ROM) is noted.
Neurologic examination. Assess sensory, motor, and reflex function of the upper and lower extremities, including abdominal reflexes.
Spinal alignment and balance assessment in the coronal plane. Normally, the head should be centered over the sacrum and pelvis. A plumb line dropped from C7 should fall through the gluteal crease.
Spinal alignment and balance assessment in the sagittal plane. When the patient is observed from the side, assess the four physiologic sagittal curves (cervical and lumbar lordosis, thoracic and sacral kyphosis). When the patient stands with the hips and knees fully extended, the head should be aligned over the sacrum. The ear, shoulder, and greater trochanter of the hip should lie on the same vertical line.
Extremity assessment. Measurement of leg lengths, assessment of joint ROM and flexibility in the upper and lower extremities, are performed. Note any contractures or deformities involving the extremities (e.g., cavus feet).
Examination of related body systems. A detailed medical assessment should be performed. Certain spinal deformities are associated with abnormalities in other organ systems, especially the neurologic, renal, and cardiac systems. In specific situations, screening for vision problems, hearing loss, and learning disorders may be required.
Idiopathic scoliosis: no apparent cause or related underlying etiology
Neuromuscular scoliosis: due to neuromuscular disorders such as cerebral palsy, muscular dystrophy, myelomeningocele, Friedreich ataxia, spina bifida, and spinal cord injury
Congenital scoliosis: due to failure of vertebrae to develop normally in utero including failure of formation (e.g., hemivertebra), or failure of segmentation (e.g., congenital bar)
Thoracogenic scoliosis: due to congenital rib fusions or chest wall tethering following thoracic surgery
Syndromic scoliosis: scoliosis in conjunction with a constellation of signs, symptoms or characteristics that are clinically recognizable (e.g., Marfan syndrome, Ehlers-Danlos syndrome, Prader-Willi syndrome, neurofibromatosis, and bone dysplasias)
Posttraumatic scoliosis: e.g., acute, chronic, and post-surgical causes
Postinfectious scoliosis: pyogenic, granulomatous
Scoliosis related to metabolic bone diseases: e.g., osteoporotic compression fractures
Tumor-related scoliosis: spinal cord or vertebral column tumors
Adult degenerative or adult scoliosis: develops in previously straight spines
Scoliosis secondary to anomalies of the lumbosacral joint: e.g., spondylolisthesis
Early onset scoliosis: onset before age 10, regardless of etiology
Adolescent idiopathic scoliosis: onset from age 10 through adulthood
Adult scoliosis: two major types: adult idiopathic scoliosis (idiopathic scoliosis in an adult which began during childhood) and adult de novo or degenerative scoliosis (onset of new scoliosis in adulthood due to degenerative changes occurring in the spinal column). Additional causes of scoliosis in adults include all types of scoliosis that develop earlier in life and continue into adulthood, as well as scoliosis that develops in adulthood from miscellaneous etiologies, including trauma and osteoporosis.
Traditionally, idiopathic scoliosis in pediatric patients was stratified into three groups based on age of onset: infantile (from birth through age 3), juvenile (age 4 through 10), and adolescent (age 10 through adulthood). As the natural history and treatment goals differ for patients less than age 10 compared to adolescent scoliosis patients, the term “early onset scoliosis” has been adopted by specialists worldwide to describe scoliosis with onset before age 10, regardless of etiology.
Early onset scoliosis represents a heterogenous population consisting of patients with congenital, neuromuscular, syndromic, and idiopathic deformities. Unlike adolescent and adult scoliosis, early onset scoliosis occurs in patients with significant remaining growth potential and high likelihood for progressive deformity, and may adversely impact lung development and reduce life expectancy. Evaluation begins with a general medical history (birth, developmental, and family history) including details regarding the patient’s spinal deformity (age at onset or diagnosis, progression, presence or absence of pain, prior treatment). Additional elements to assess include height, weight, nutritional status, achievement of age-appropriate developmental milestones, pulmonary status, and investigation for comorbidities. Depending on deformity etiology, coexisting disorders may involve the neural axis, cardiac, urogenital, musculoskeletal, gastrointestinal, pulmonary, and integumentary systems.
The patient should be examined with the back exposed ( Fig. 6.1 ). First, the patient is examined in the standing position. Second, the patient is examined as he or she bends forward at the waist, with arms hanging freely, knees straight, and feet together. Findings that suggest the presence of scoliosis include:
Shoulder height asymmetry
Scapula or rib prominence
Chest cage asymmetry
Unequal space between the arm and the lateral trunk on side to side comparison
Waistline asymmetry
Asymmetry of the paraspinous musculature
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here