Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
THE ANESTHESIA PRACTITIONER IS OFTEN FACED with a child who has acute kidney injury (AKI) or renal failure. Renal disease requires the practitioner to be vigilant about fluid homeostasis, acid-base balance, electrolyte management, choice of anesthetics, and potential complications. This requires a thorough understanding of the excretory and fluid homeostatic functions of the kidney, particularly in the neonate and younger child. If not managed assiduously, perioperative renal dysfunction can deteriorate into renal failure or multiorgan system failure resulting in significant morbidity or mortality. The anesthesia provider must understand renal physiology, appropriate preoperative preparation, intraoperative management, and postoperative care of the child with renal disease.
The basic functions of the kidney are to maintain fluid and electrolyte homeostasis and metabolism. The first step in this tightly controlled process is the production of the glomerular filtrate from the renal plasma. The glomerular filtration rate (GFR) depends on renal blood flow (RBF), which depends on the systolic blood pressure and circulating blood volume. The kidneys are the best perfused organs per gram of weight in the body. They receive 20% to 30% of the cardiac output maintained over a wide range of blood pressures through changes in renal vascular resistance. Numerous hormones play a role in this autoregulation, including vasodilators (i.e., prostaglandins E and I 2 , dopamine, and nitric oxide) and vasoconstrictors (i.e., angiotensin II, thromboxane, adrenergic stimulation, and endothelin). Congestive heart failure and volume contraction severely limit the ability of the kidney to maintain autoregulation.
When adjusted for body surface area (BSA) or scaled using allometric theory (see Chapter 7 ), both RBF and GFR double in the first 2 weeks of postnatal life and both continue to increase steadily, reaching adult values by 2 years of age (see Figs. 7.11 and 7.12 ). The increases in RBF over time parallel similar increases in cardiac output and decreases in renal vascular resistance. The initial GFR and the rate of increase during the first few years correlate with the neonate's postmenstrual age at birth. For example, the GFR (corrected using BSA or allometry) of a neonate born at 28 weeks gestation is one-half of that of a full-term infant (see Figs. 7.11 and 7.12 ). GFR may be estimated from the serum creatinine concentration and the height of the child according to the following formula :
In the equation, k is a constant that varies with age; 0.413 for infants, 0.55 for children, and 0.7 for adolescent boys. The serum creatinine concentration, especially in the first days of life, reflects the maternal serum creatinine concentration and therefore cannot be used to predict neonatal renal function until at least 2 days after birth.
The kidney regulates the total body sodium balance and maintains normal extracellular and circulating volumes. The adult kidney filters 25,000 mEq of sodium per day, but it excretes less than 1% through extremely efficient resorption mechanisms along the nephron. The proximal tubule resorbs 50% to 70%, the ascending limb of the loop of Henle resorbs about 25%, and the distal nephron accounts for 10% of the filtered sodium load. Several hormones, including renin, angiotensin II, aldosterone, and atrial natriuretic peptide (ANP), and changes in circulating blood volume contribute to maintaining the sodium balance.
Serum osmolality is tightly regulated through changes in arginine vasopressin (AVP) release and thirst. AVP, also called antidiuretic hormone, is synthesized in the hypothalamus and stored in the posterior pituitary, where it is released in response to an increasing plasma osmolality. AVP is also released in response to decreases in the circulating blood volume and hypotension, including responses to nausea, vomiting, opioids, inflammation, and surgery. AVP binds to receptors in the collecting duct, increasing the permeability of the tubules to water and leading to increased water resorption and concentrated urine. Neonates are much less able to conserve or excrete water compared with older children, rendering the fluid management and volume issues important tasks for the anesthesiologist in this young age group.
The regulation of serum potassium is managed by the kidney and depends on the concentration of plasma aldosterone. Aldosterone binds to receptors on cells in the distal nephron, increasing the secretion of potassium in the urine. Neonates are much less efficient at excreting potassium loads compared with adults, and the normal range of serum potassium concentrations is therefore greater in neonates; Table 28.1 provides the normal values. Potassium regulation is affected by the acid-base status; excretion of potassium increases in the presence of alkalosis and decreases in the presence of acidosis. Causes of hyperkalemia and hypokalemia are presented in Tables 28.2 and 28.3 , respectively.
| Age | Serum Potassium Range (mEq/L) |
|---|---|
| 0–1 month | 4.0–6.0 |
| 1 month–2 years | 4.0–5.5 |
| 2–17 years | 3.8–5.0 |
| >18 years | 3.2–4.8 |
| Transcellular Shifts |
| Acidosis |
| β-Adrenergic blockers |
| Insulin deficiency |
| Burns |
| Tumor lysis syndrome |
| Rhabdomyolysis |
| Succinylcholine |
| Decreased Excretion |
| Renal failure |
| Potassium-sparing diuretics |
| Cyclosporine |
| Nonsteroidal antiinflammatory drugs |
| Angiotensin-converting enzyme inhibitors |
| Mineralocorticoid deficiency |
| Adrenal insufficiency |
| Congenital adrenal hyperplasia |
| Hyporeninemic hypoaldosteronism |
| Primary mineralocorticoid deficiency |
| Mineralocorticoid resistance |
| Prematurity |
| Obstructive uropathy |
| Pseudohypoaldosteronism |
| Increased Intake |
| Potassium supplements, oral or intravenous |
| Blood transfusions |
| Potassium-containing antibiotics |
| Transcellular Shift |
| Insulin |
| β-Adrenergic agonists |
| Increased Excretion |
| Vomiting |
| Diarrhea |
| Nasogastric suction |
| Laxatives |
| Diuretics |
| Cisplatin |
| Amphotericin B |
| Renal tubular acidosis |
| Bartter syndrome |
| Corticosteroids |
| Decreased Intake |
| Malnutrition |
| Anorexia nervosa |
The kidney is involved in the regulation of acid-base balance and the response to the stress of illness. The kidney reclaims virtually all of the filtered bicarbonate in the proximal tubule and regenerates bicarbonate (HCO 3 − ) lost in the neutralization of acid generated by the normal combustion of food, especially protein, and the formation of bone. New bicarbonate is the product of cells in the distal nephron that decompose the carbonic acid (H 2 CO 3 ) formed from water (H 2 O) and carbon dioxide (CO 2 ) by carbonic anhydrase. The protons (H + ) that are generated from this process are pumped into the lumen of the collecting duct, where they combine with hydrogen phosphate (HPO 4 2− ) or ammonia (NH 3 ) generated by the catabolism of amino acids, mainly glutamine, in the tubule cells.
Infants, especially neonates, maintain a slightly acidotic blood (pH = 7.37) and decreased plasma bicarbonate concentration (22 mEq/L) compared with older children and adults (pH = 7.39; plasma bicarbonate = 24 to 28 mEq/L). The reduced plasma concentration of HCO 3 − is the result of a reduced threshold or the plasma concentration at which HCO 3 − is incompletely resorbed by the kidney. Neonates maintain acid-base homeostasis but are limited in their ability to respond to an acid load. This is especially true for preterm infants.
The causes of and differences in renal diseases between children and adults are substantive. Depending on the cause of the renal disease, management may be different. Adult renal disease usually results from long-standing diabetes mellitus or hypertension with an associated compromise in cardiovascular function. Children may also have renal failure owing to diseases such as sickle cell disease or systemic lupus erythematosus, but cardiovascular function is far less commonly compromised.
Acute renal failure (ARF) or acute renal insufficiency is defined as an abrupt deterioration in the ability of the kidneys to clear nitrogenous wastes, such as urea and creatinine. Concomitantly, there is a loss of ability to excrete other solutes and maintain a normal water balance. This leads to the clinical presentation of acute renal insufficiency: edema, hypertension, hyperkalemia, and uremia.
Acute kidney injury (AKI) has almost replaced the traditional term acute renal failure (ARF), which was used in reference to the subset of patients who had an acute need for dialysis. With the recognition that even modest increases in serum creatinine are associated with a dramatic increase in mortality, the clinical spectrum of acute decline in GFR is broader. Minor deterioration in GFR and kidney injury are captured in a working clinical definition of kidney damage that allows early detection and intervention and uses AKI in place of ARF. The term ARF is preferably restricted to those with AKI who also require renal replacement therapy. The prognosis of AKI is assessed in part by the use of the RIFLE criteria, which include three severity categories (i.e., R isk, I njury, and F ailure) and two clinical outcome categories ( L oss and E nd-stage renal disease) ( Table 28.4 ).
| RIFLE Factors | GFR Criteria | Urine Output Criteria | |
|---|---|---|---|
| Risk | Increased Cr × 1.5 or decreased GFR >25% | UOP <0.5 mL/kg per hour > 6 hours | High sensitivity |
| Injury | Increased Cr × 2 or GFR decrease >50% | UOP <0.5 mL/kg per hour > 12 hours | |
| Failure | Increased Cr × 3 or GFR decrease of 75% or Cr ≥4 mg/dL Acute rise ≥0.5 mg/dL |
UOP <0.3 mL/kg per hour > 24 hours or Anuria > 12 hours |
|
| Loss | Persistent ARF: complete loss of kidney function > 4 weeks | High specificity | |
| ESKD | End-stage kidney disease (> 3 months) | ||
The term ARF has often been incorrectly used interchangeably with acute tubular necrosis (ATN), which usually refers to a rapid deterioration in renal function occurring minutes to days after an ischemic or nephrotoxic event. Although acute tubular necrosis is an important cause of ARF, it is not the sole cause, and the terms are not synonymous. For the purposes of this chapter, AKI refers to the disease formerly called ARF.
AKI is often multifactorial in origin or the result of several distinct insults. To treat AKI, it is important to understand its causes and pathophysiology. The etiologies of AKI are varied, but can be broadly classified as follows ( Table 28.5 ):
Prerenal, implying poor renal perfusion as the cause
Renal, implying intrinsic renal disease or damage as the cause
Postrenal, implying an obstruction to the excretion of urine as the cause
| Prerenal Failure | Renal Failure | Postrenal Failure |
|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Prerenal insults comprise the majority (up to 70%) of cases of AKI. They usually result from massive losses of extracellular fluid, such as in gastroenteritis, burns, hemorrhage, or excessive diuresis, as well as in cardiac failure and sepsis. The common feature of this condition is diminished renal perfusion. In response to the reduction in RBF, there is a compensatory increase in afferent tone, which decreases the GFR and increases the retention of salt and water. The net effect of these events is a drastic reduction in urine volume, often leading to oliguria and/or anuria. If the underlying problem is recognized early and treated aggressively, progressive renal insufficiency may be averted. Nonsteroidal antiinflammatory drugs, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin receptor blockers can aggravate prerenal azotemia by further reducing glomerular capillary pressure and the GFR.
Parenchymal disease or injury accounts for 20% to 30% of the cases of abrupt onset of AKI. In infants, the common causes include birth asphyxia, sepsis, and cardiac surgery. In older children, the important causes of AKI include trauma, sepsis, and hemolytic uremic syndrome. Prolonged prerenal azotemia may result in overt renal injury. Similarly, intrarenal obstruction to blood flow from thrombi or vasculitis may cause renal failure. Drugs such as aminoglycosides or amphotericin B or other nephrotoxins, including radiocontrast agents, may induce AKI through tubular or interstitial injury as a result of allergic reactions, as can be seen with penicillins. Acute glomerulonephritis is another cause of AKI in children; rarely, pyelonephritis can lead to AKI.
The remaining causes of AKI result from the obstruction to urine flow. These conditions account for less than 10% of all cases of AKI and may involve obstruction of both kidneys. Sudden anuria suggests a postrenal cause for the AKI. The obstruction can occur within the collecting system of the kidney (intrarenal), in the ureter, or in the urethra (extrarenal). Intrarenal obstruction may occur with the tumor lysis syndrome with the deposition of uric acid crystals, from myoglobinuria, hemoglobinuria, or from medications such as acyclovir and cidofovir. Extrarenal obstruction can be caused by stones inspissated in the ureters or from external compression by lymph nodes or a tumor. As with other forms of AKI, prompt recognition and appropriate intervention to relieve the obstruction may facilitate full recovery of renal function and obviate a permanent reduction in renal function.
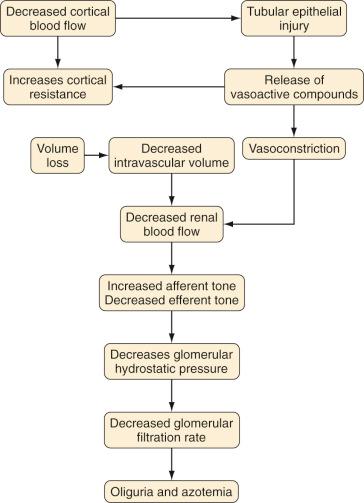
The exact pathophysiology of AKI remains unclear, but several factors have been identified. In the initial phase of AKI, profound renovascular vasoconstriction reduces GFR ( Fig. 28.1 ). Factors known to increase renal vasoconstriction include increased activity of the renin-angiotensin and the adrenergic systems and endothelial dysfunction with increased endothelin release and decreased nitric oxide synthesis. However, therapeutic interventions to vasodilate the intrarenal vasculature, such as prostaglandin and dopamine infusions, ACE inhibitors, calcium channel blockers, and endothelin receptor antagonists, have not significantly reversed established AKI.
Another factor in the pathogenesis of AKI is renal tubule cell injury, the direct result of a nephrotoxic agent or from an ischemic insult ( Fig. 28.2 ). Cellular injury leads to sloughing of the brush border, swelling, mitochondrial condensation, disruption of cellular architecture, and loss of adhesion to the basement membrane with shedding of cells into the tubular lumen. These changes, which occur within minutes of an ischemic event, contribute to the decreased GFR by obstructing the lumen of the tubule. These cellular changes allow the filtrate to leak back into the peritubular blood, reducing the excretion of solutes and the effective GFR.
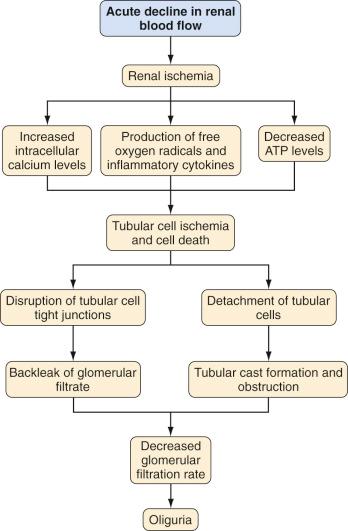
Some of the cellular derangements in AKI, such as a reduction in ATP concentrations, cell membrane injury by reactive oxygen molecules, and increased intracellular calcium concentrations from changes in membrane phospholipid metabolism, lead to cell death. Reactive oxygen molecules also stimulate the production of cytokines and chemokines that play a role in cell injury and vasoconstriction.
Neutrophils that are recruited during reperfusion injury after renal ischemia mediate parenchymal renal damage. Reperfusion injury increases intracellular adhesion molecule 1 (ICAM-1) on endothelial cells promoting the adhesion of circulating neutrophils and their eventual infiltration into the parenchyma. Neutrophils then release reactive oxygen molecules, elastases, proteases, and other enzymes that lead to further tissue injury.
A thorough history and physical examination can yield important insight into the likely causes of AKI. The initial laboratory assessment of a child with AKI should include the measurement of serum urea, creatinine, electrolytes, and a urinalysis. Prerenal azotemia is typically associated with a ratio of blood urea nitrogen (BUN) to creatinine that exceeds 20. In cases of renal parenchymal dysfunction, this ratio is closer to 10. Hematuria and proteinuria are consistently present in AKI, independent of the cause, although the presence of cellular casts, especially red blood cell casts, in the urinary sediment is suggestive of glomerulonephritis. Granular casts are associated with prerenal azotemia.
One test to distinguish prerenal azotemia from established renal failure from ischemia or nephrotoxins is the fractional excretion of sodium (FE Na ). The FE Na is calculated using the following equation:
U Na and S Na are urine and serum sodium concentrations, and U Cr and S Cr are the urine and serum creatinine concentrations, respectively. In prerenal azotemia, the FE Na is usually less than 1% for adults and children and less than 2.5% for infants. In established AKI from ischemia and nephrotoxins, but not acute glomerulonephritis, the FE Na usually exceeds 1%. Administration of diuretics may confound the interpretation of this test.
The initial radiologic assessment of children with AKI is ultrasonography. Renal ultrasound does not depend on renal function and can define the renal anatomy, changes in parenchymal density, and possible outlet obstruction by demonstrating dilation of the urinary tract. Doppler interrogation of the renal vessels provides information on vascular flow. Further radiographic studies, such as voiding cystourethrography, nuclear renal flow scanning, dynamic functional MRI, and abdominal computed tomography (CT), may be indicated in select children and conditions.
Therapeutic interventions in children with AKI should be aimed at the underlying cause and at improving renal function and urine flow. Children with AKI caused by hypovolemia should be fluid resuscitated with at least 20 mL/kg over 30 to 60 minutes with normal saline solution or a balanced salt solution. For children with significant hypotension, an alternative choice is a colloid-containing solution. Children with oliguria caused by hypovolemia usually respond within 4 to 6 hours with increased urine output. Anecdotal reports have supported the use of low-dose dopamine in AKI. A recent clinical trial has demonstrated benefit from dopamine in improving urine output in very low–birth-weight neonates.
Diuretics have been commonly used to treat oliguric AKI. There are several theoretical reasons why mannitol, furosemide, and other loop diuretics may ameliorate AKI. First, diuretics may convert oliguric AKI to nonoliguric AKI. Second, loop diuretics decrease energy-driven transport in the loop of Henle, and this may protect cells in regions of hypoperfusion. However, neither mannitol nor loop diuretics can predictably convert an oliguric patient with AKI to a polyuric patient. Diuretics have not been shown in clinical studies to influence renal recovery, need for dialysis, or survival in patients with AKI. Diuretics should be used only after the circulating volume has been adequately restored and should be stopped if there is no early response.
Dopamine has been widely used to prevent and manage AKI. In low doses (0.5–2.0 µg/kg per minute), dopamine increases renal plasma flow, GFR, and renal sodium excretion by activating dopaminergic receptors. Infusion rates in excess of 3 µg/kg per minute stimulate α-adrenergic receptors on systemic arterial resistance vasculature, causing vasoconstriction; cardiac β 1 -adrenergic receptors, increasing cardiac contractility, heart rate, and cardiac index; and β 2 -adrenergic receptors on systemic arterial resistance vasculature, causing vasodilatation. In a meta-analysis of 24 studies and 854 adult patients, dopamine did not prevent renal failure, alter the need for dialysis, or change the mortality rate. In a randomized clinical trial of low-dose dopamine in 328 critically ill adult patients, dopamine did not change the duration or severity of the renal failure, need for dialysis, or mortality. From these data, the routine use of low-dose dopamine in patients with AKI cannot be supported.
Several other agents that were useful in experimental models of AKI have been investigated but have not shown clinical success. ANP increases GFR in animal models of AKI by increasing renal perfusion pressure and sodium excretion. An initial study demonstrated some benefit with ANP in patients with AKI, especially in those with oliguric AKI, although a subsequent study of 222 adult patients with oliguric AKI failed to detect a difference between patients treated with ANP and placebo in terms of the need for dialysis or mortality. Insulin-like growth factor 1 has been beneficial in animal models of AKI, presumably by potentiating cell regeneration. However, in a multicenter, placebo-controlled trial in adult patients with AKI, insulin-like growth factor 1 failed to speed the recovery, decrease the need for dialysis, or alter mortality. Thyroxine abbreviates the course of experimental AKI but had no effect on the duration of renal failure and actually increased mortality threefold (by suppression of thyroid-stimulating hormone).
In patients with severe AKI, renal replacement therapy through dialysis is life sustaining. The indications for initiation of dialytic therapy are persistent hyperkalemia, volume overload refractory to diuretics, severe metabolic acidosis, and overt signs and symptoms of uremia such as pericarditis and encephalopathy. Many nephrologists recommend dialysis if the BUN value approaches 100 mg/dL or even earlier, especially in the oliguric patient, although this has not proved to alter outcome. A retrospective study that compared early (BUN <60 mg/dL) versus late (BUN >60 mg/dL) initiation of dialysis in adult patients suggested that early initiation improved survival. However, the timing of the initiation of dialysis remains an unresolved question.
Three strategies are available to replace renal function in critically ill children and adults: hemodialysis, peritoneal dialysis, and a variation of continuous replacement therapies, such as continuous venovenous hemofiltration (CVVH), continuous venovenous hemodialysis (CVVHD), and continuous venovenous hemodiafiltration (CVVHDF). None of these strategies has been proven superior to the others. However, in the individual child, one strategy may be more practical than the others. Hemodialysis is technically more difficult than peritoneal dialysis in an infant and hemodynamically unstable children. Continuous replacement therapies appear to cause less hemodynamic instability compared with hemodialysis and offer more predictable solute and fluid removal than peritoneal dialysis. Hemodialysis and continuous replacement therapies require large-bore vascular access to achieve the large blood flows that are necessary to support these strategies.
Although these three strategies differ technically, they share similar principles ( Fig. 28.3 ). All three strategies remove nitrogenous wastes (i.e., urea), excess fluid, and excess solutes, especially potassium. This is achieved by circulating the child's blood over a semipermeable membrane that separates the blood from a salt solution (i.e., dialysate) on the contralateral surface. The movement of solutes across the membranes occurs by diffusion (i.e., solutes move across the membrane along their concentration gradients) and ultrafiltration (i.e., osmotic or hydrostatic pressures). The rate of removal of water and solute waste depends on the characteristics of the membrane (i.e., pore size and selectivity), diffusion, and ultrafiltration.
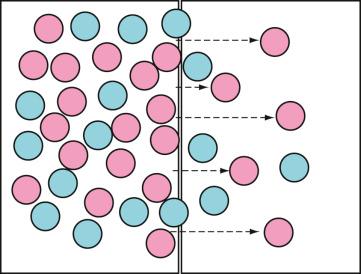
The permeability characteristics and surface areas for the membranes are known for specific dialyzers used in hemodialysis and hemofiltration. The peritoneum serves as the dialysis membrane in peritoneal dialysis and remains physically unalterable, but changes in dialysate composition and length of time the dialysate is exposed to the peritoneal membrane changes the amount of solute and water removed. In all forms of renal replacement therapy, the therapeutic prescription is individualized for the child.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here