Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Endovascular therapy (EVT) has increasingly become the initial clinical option for treating both claudication and critical limb ischemia (CLI). Similar to the evolution of open bypass surgery, EVT began above the knee and has been progressively extended to the infrapopliteal segment, now even including the pedal and arch vessels. Enthusiasm for infrapopliteal EVT was tempered by poor initial results, but advances in technique, equipment, and patient selection have led to improved outcomes and more widespread EVT application. This chapter discusses standard techniques for infrapopliteal EVT and reviews the contemporary results of tibial angioplasty, stenting, and atherectomy.
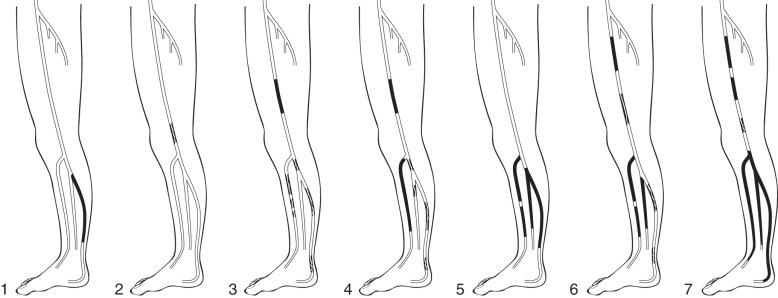
The revised Trans-Atlantic Inter-Society Consensus (TASC II) guidelines provide the current consensus recommendations for EVT. TASC II guidelines do not delineate specific anatomic criteria for infrapopliteal disease and do not formally recommend infrapopliteal EVT, whereas previous TASC guidelines included anatomic criteria for infrapopliteal lesions ( Table 31.1 ). TASC II guidelines mention growing evidence to support EVT for infrapopliteal occlusions in patients with comorbidities in whom in-line flow to the foot can be reestablished. In addition, the guidelines also point out that failed angioplasty does not usually preclude subsequent bypass. Graziani and colleagues also proposed a classification system for patients with CLI secondary to multilevel infrainguinal disease ( Fig. 31.1 ). Arterial lesions were graded class 1 to class 7, indicating progressive disease severity with decreasing transcutaneous oxygen tension (TcPO 2 ).
| Classification | Lesions Characteristics |
|---|---|
| TASC A | Single stenosis <1 cm long in tibial or peroneal vessels |
| TASC B | Multiple focal stenoses of tibial or peroneal vessels <1 cm long |
| One or two stenoses <1 cm long involving the trifurcation | |
| Short tibial or peroneal stenosis with femoropopliteal PTA | |
| TASC C | Stenoses 1–4 cm long in tibial or peroneal vessels |
| Occlusions 1–2 cm long in tibial or peroneal vessels | |
| Extensive stenosis of the trifurcation | |
| TASC D | Occlusion >2 cm long in tibial or peroneal vessels |
| Diffusely diseased tibial or peroneal vessels |
The decision to proceed with infrapopliteal EVT is based on many factors gathered from a complete history, physical examination, laboratory studies, noninvasive imaging, and frequently diagnostic angiography. A surgeon must carefully consider the indication (claudication vs. CLI), disease severity, functional status, age and medical comorbidities, availability and quality of an autologous vein conduit, and prior extremity interventions. EVT is preferred in patients with less severe disease, more comorbidities, shorter life expectancy, and absent suitable autologous vein. Open bypass surgery is more strongly considered for younger, healthier patients, especially when a good autologous vein conduit is available.
Infrapopliteal EVT is best performed through the ipsilateral common femoral artery (CFA) using an antegrade approach. The proximal CFA should be accessed to allow working room between the puncture site and superficial femoral artery (SFA). Accessing the contralateral CFA for an up-and-over approach is also possible, but is probably better reserved for treating lesions above the knee. The antegrade approach has distinct advantages: better wire and catheter control and “pushability” using shorter devices, no routine use of a long sheath, and no requisite crossing of the aortoiliac vessels. Both groins should always be prepared in case an alternative approach is required.
Once the ipsilateral CFA has been accessed, a guidewire is manipulated anteromedially to cannulate the SFA. If this is not possible, the wire can be advanced down the profunda femoris artery, and a short, angled-tip catheter is advanced over the wire. Lateral anterior oblique positioning of the image intensifier helps open the femoral bifurcation. The catheter is withdrawn slowly while puffing contrast until the femoral bifurcation is clearly demonstrated. The catheter tip is steered medially and anteriorly toward the SFA, and the guidewire is advanced into the SFA. The access sheath diameter is typically 5 French, although tibial angioplasty with 0.014- and 0.018-inch platforms can be performed through a 4 French sheath. If an up-and-over approach is used, a long sheath with its tip in the popliteal artery facilitates tibial interventions.
After sheath placement, a diagnostic angiogram is performed through its side port. Lesions above the knee are well delineated in this manner. A short 0.035-inch guidewire is maneuvered into the popliteal artery below the knee, and a 4 or 5 French Glidecath (Medi-Tech, Watertown, MA) is advanced to the end of the wire. Digital subtraction angiography is then used to identify lesions in the trifurcation and distal runoff vessels into the foot. Lateral views of the foot are routinely obtained.
Both transluminal and subintimal approaches can be used for infrapopliteal angioplasty. When choosing a wire for crossing infrapopliteal lesions, several characteristics must be considered, including size (0.035, 0.018, or 0.014 inches), length (180 to 300 cm), coating (bare or hydrophilic), base metal construction (stainless steel, nitinol), stiffness, weight, and tip construction (stiffness, length, coating, shape). Smaller caliber wires (0.014 or 0.018 inches) with a hydrophilic coating and floppy tip are often used to cross tibial lesions. The preferred wires are 0.014-inch, nonhydrophilic, medium-weight with short floppy tips for crossing tibial stenoses. Occlusions, particularly when calcified and long, are more difficult to cross. The V18 wire (Boston Scientific, Natick, MA) is particularly useful for crossing tibial occlusions. Contemporary use of the retrograde pedal approach has increased technical success rates when confronting complicated anatomy.
If difficulty arises when attempting to cross stenotic lesions or occlusions with a particular wire, several additional maneuvers are available to facilitate success. Particularly hard or calcified plaque can cause 0.014- and 0.018-inch wires to coil, especially if they have floppy tips. Upsizing to a 0.035-inch wire may give the additional support needed to navigate across the difficult lesion. Another option is the use of a catheter, such as the hydrophilic Glidecath, which can be advanced to the end of the wire and lend additional support. Crossing catheters, such as the Quick-Cross (Spectranetics, Colorado Springs, CO), feature a firmer, tapered tip, which facilitates lesion crossing. These micro-catheters have also been reinforced with a metallic braid, resulting in increased pushability, such as is seen in the CXI family (COOK, Bloomington, IN). Predilation with a small, 2- to 2.5-mm–diameter coronary balloon may fracture a particularly difficult lesion and subsequently allow passage of a wire or low-profile crossing catheter. Guidewires with dilatable tips are also available for this technique. Devices specifically designed for crossing a chronic total occlusion (CTO) are a more recent development. These devices use different strategies to facilitate lesion crossing, including plaque microdissection (Frontrunner XP CTO Catheter; Cordis, Bridgewater, NJ), fast and bidirectional catheter spinning (CrossBoss CTO Catheter; BridgePoint Medical, Plymouth, MN), and catheter tip deflection capability with spiral wedges to facilitate advancement (Wildcat Catheter; Avinger, Redwood City, CA).
Subintimal angioplasty is a useful technique first described by Bolia and coworkers in 1989 for the treatment of long-segment femoropopliteal occlusions. This technique may also be successfully applied to infrapopliteal lesions ( Fig. 31.2 , see color insert). A wire is used to intentionally create a subintimal dissection plane just proximal to an occlusion. The wire is typically formed into a short J shape and is advanced in the subintimal plane until the occlusion has been passed. If reentry into the true lumen is difficult, it may be facilitated by a special reentry device, such as the Outback LTD (Cordis, Dublin, OH) or the Enteer reentry system (Medtronic, Minneapolis, MN)

Once a stenosis or occlusion has been crossed successfully, balloon angioplasty is possible ( Fig. 31.3 , see color insert). Balloon angioplasty stretches the arterial wall causing plaque fracture and sometimes local dissection, which is usually not flow limiting. Treating long-segment tibial lesions with longer balloons is a useful technique, but some short, focal lesions require a shorter balloon with more directed dilation force. A cutting balloon (Boston Scientific), which features three to four microsurgical blades fixed longitudinally along the outer surface of a noncompliant balloon, is particularly useful for the intimal hyperplasia near graft anastomoses. Creating controlled cuts in the intima theoretically allows less vessel wall disruption, less neutrophil activation, and more controlled balloon dilation. The drug-coated balloon (DCB) is another emerging technology that has been primarily used in markets outside of the United States and has yet to receive US Food and Drug Administration (FDA) approval.

Stenting in the infrapopliteal segment has traditionally been reserved for obviating emergency surgery because of poor angioplasty results, such as a flow-limiting dissection. More recently, drug-eluting stents have been used for the treatment of infrapopliteal disease, with encouraging results. Other infrapopliteal maneuvers, such as atherectomy and cryotherapy, may add more cost than real benefit compared to angioplasty alone.
In 2008, Montero-Baker and colleagues reported that antegrade revascularization failed in up to 62 (17.8%) of 343 limbs with complex total occlusions of the popliteal and/or infrapopliteal vascular territory. Retrograde transpedal access has increased technical success during complex tibioperoneal interventions.
Various authors have published their own series. A total of 881 patients are currently accounted for in peer-reviewed journals. In general terms, all of these papers conclude that transpedal access is safe and effective. Transpedal access was initially used as an adjunctive access site when preceded by unsuccessful attempts at antegrade recanalization. It is noteworthy that CTOs were present in more than 90% of patients with average occlusion lengths greater than 220 cm, demonstrating the effectiveness of this technique since the technical success rate remained greater than 90% with relatively low contrast volume, reasonable procedure times, and low rates of procedural complications. Retrograde access is increasingly used primarily rather than serving as a bailout approach, especially when anatomic difficulties are anticipated.
In essence, the technique has evolved and is based on ultrasound-guided retrograde distal access, although some operators still advocate the use of fluoroscopy to guide access. Once the needle is placed in the intraluminal space, access can be secured with or without a sheath. In cases in which a sheath is used, experienced users advise the use of 4 French or smaller sheaths. Most authors agree that this access can usually be done in a sheathless fashion; the objective is to cross the lesion from below, but deliver therapy in an antegrade fashion once the wire has been snared from above.
The outcome of infrapopliteal EVT depends on many factors, including indication for the procedure, lesion characteristics, runoff status, comorbidities, and technical factors such as dissection or persistent stenosis ( Table 31.2 ). Poorer outcomes appear to be predicted by the following factors: CLI versus claudication, longer lesion length, poor runoff status, comorbidities of diabetes and renal failure, smoking, and untreated intraprocedure flow-limiting dissection and persistent stenosis greater than 30%.
| Author | Year | Number Treated | CLI | Mean Lesion Length | Technical Failures | Primary Patency | Limb Salvage Rate |
|---|---|---|---|---|---|---|---|
| Angioplasty | |||||||
| Giles and colleagues | 2008 | 176 | 100% | NR | 7% | 53%, 1 year 51%, 2 years |
84%, 3 years |
| Conrad and colleagues | 2009 | 155 | 86% | NR | 5% | 71%, 2 years 62%, 3.3 years |
86%, 3.3 years |
| Sadek and colleagues (Single vs. multilevel PTA) |
2009 | 89 | 77% | NR | 9% | 34%, 1 year | 67%, 1.5 years |
| Single level | Single level | ||||||
| 58%, 1 year | 63%, 1.5 years | ||||||
| Multilevel | Multilevel | ||||||
| Peregrin and colleagues | 2010 | 1445 | 100% | NR | 11% | NR | 76%, 1 year |
| Schmidt and colleagues | 2010 | 62 | 100% | 18.3 cm | 5% | 50%, 3 months | 100%, 15 months |
| Subintimal Angioplasty | |||||||
| Ingle and colleagues | 2002 | 70 | 91% | NR | 14% | NR | 94%, 3 years |
| Vraux and Bertoncello | 2006 | 50 | 100% | 78% >10 cm | 18% | 46%, 1 year | 87%, 1 year |
| 42%, 2 years | 87%, 2 years | ||||||
| Tartari and colleagues (SFA only in 27 limbs) |
2007 | 109 | 100% | 59% ≥10 cm | 17% | NR | 87%, 1 year 85%, 2 years |
| Cutting-Balloon Angioplasty | |||||||
| Engelke and colleagues | 2002 | 16 | 31% | NR | 6% | 67%, 1 year | 93%, 10 months |
| Ansel and colleagues | 2004 | 73 | 71% | 2.7 cm | 0% | NR | 89%, 1 year |
| Vikram and colleagues | 2007 | 11 | NR | NR | 18% | 50%, 1 year | NR |
| Drug-Coated Balloon a | |||||||
| Tepe and colleagues | 2008 | 48 | 15% | 7.5 cm | 2% All cases | 80%, 6 months | 96%, 6 months |
| Stenting | |||||||
| Feiring and colleagues | 2004 | 92 | 68% | NR | 7% | NR | 87%, 1 year |
| Bosiers and colleagues | 2006 | 300 | 100% | NR | NR | 76%, 1 year | 99%, 1 year |
| Donas and colleagues | 2009 | 34 | 100% | 6.5 cm stenosis; 7.5 cm occlusion | 3% | 91%, 10 months | 100%, 10 months |
| Randon and colleagues | 2010 | 16 | 100% | 38% ≥10 cm | 13% | 56%, 1 year | 92%, 1 year |
| Drug-Eluting Stent | |||||||
| Scheinert and colleagues | 2006 | 30 | 63% | NR | 0% | 100%, 6 months | 100%, 9 months |
| Feiring and colleagues | 2010 | 130 | 100% | NR | 9% | NR | 88%, 3 years |
| Karnabatidis and colleagues | 2011 | 51 | 100% | 7.7 cm | 0% | 30%, 3 years | NR |
| Rastan and colleagues | 2011 | 82 | 51% | 3.0 cm | 0% | 81%, 1 year | 98%, 1 year |
| Atherectomy | |||||||
| Zeller and colleagues | 2007 | 36 | 53% | 4.6 cm | 2% | 67%, 1 year 60%, 2 years |
100%, 2 years |
| Safian and colleagues | 2009 | 124 | 32% | 3.0 cm | 2.5% | NR | 100%, 6 mo |
Giles and associates retrospectively reviewed 163 consecutive patients (176 limbs) who underwent infrapopliteal EVT for CLI; 102 patients (58%) also had concomitant femoropopliteal angioplasty or stenting, or both ; and 97 lesions (55%) were TASC C or D. Subintimal angioplasty was performed only for complete occlusions that could not be crossed transluminally. The technical success rate was 93%, and 1- and 2-year primary patency rates were 53% and 51%, respectively. The 3-year limb salvage was 84%. On multivariate analysis, predictors of restenosis were TASC D lesions and lack of a bypass target, whereas multilevel intervention was protective. Sadek and colleagues retrospectively reviewed 85 patients (89 limbs) who underwent either single-level tibial (29 limbs) or multilevel (60 limbs) interventions. Overall, 77% of patients had CLI. The technical success rate was 91%, and 12- and 18-month primary patency rates were 34% and 27%, respectively, in the single-level interventions and 58% and 48%, respectively, in the multilevel interventions. The 12- and 18-month limb salvage rates in the single-level interventions were 75% and 67%, respectively, and in the multilevel interventions they were 84% and 63%, respectively. The difference of primary patency and limb salvage between the two groups did not reach statistical significance. Peregrin and associates retrospectively reviewed 1268 patients (1445 limbs) who underwent infrapopliteal angioplasty for CLI. Almost all lesions were classified as TASC D. The technical success rate was 89%, and the primary and secondary limb salvage rates at 1 year were 76% and 84%, respectively. Interestingly, the number of patent infrapopliteal arteries at the end of angioplasty significantly correlated with 1-year limb salvage rates. As the number of patent crural arteries increased from 0 to 3, the 1-year limb salvage rate increased from 56% to 83%. Conrad and colleagues retrospectively reviewed 144 patients (155 limbs) who underwent infrapopliteal angioplasty; 133 limbs (86%) were treated for CLI, and 116 limbs (75%) had TASC C or D lesions. The technical success rate was 95%, and the 24- and 40-month primary patency rates were 71% and 62%, respectively. Multivariate analysis showed poor runoff, CLI, and dialysis as negative predictors of patency. The 40-month limb salvage rate was 86%; negative predictors of limb salvage included dialysis and failure to improve runoff.
Data are also available regarding angioplasty for long-segment infrapopliteal disease. Schmidt and coworkers studied 58 patients (62 limbs) with CLI who underwent infrapopliteal angioplasty for lesions 8 cm or greater in length. The technical success rate, defined by restoration of flow in at least one infrapopliteal vessel, was 95%. At short-term follow-up of 3 months, angiography demonstrated restenosis of less than 50% in 31% of treated arteries, restenosis greater than 50% in 31%, and occlusion in 38%. Clinical improvement (wound healing or improvement of rest pain) was present in 76% of treated limbs. All arteries with restenosis greater than 50% or occlusion were retreated. At 15 months, 77% of limbs showed further clinical improvement, and the limb salvage rate was 100% without bypass.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here