Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
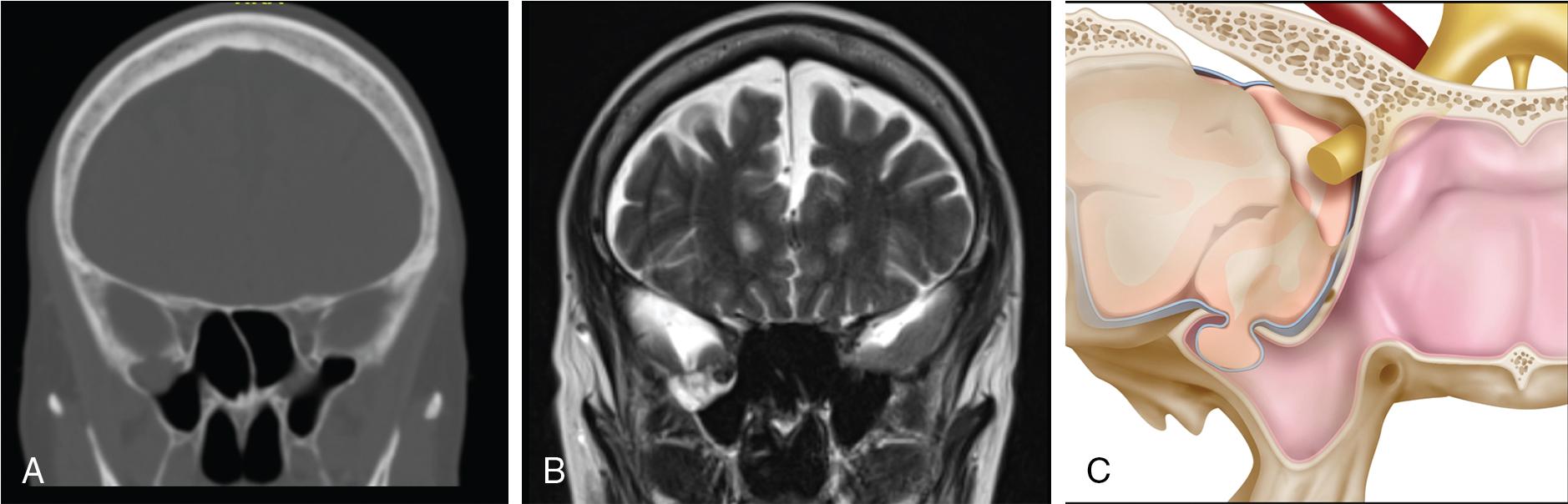
The most common locations for skull base defects of the middle cranial fossa (MCF) are the lateral sphenoid sinus or the thin tegmen of the temporal bone. Defects in the MCF skull base allow a direct communication between the intracranial compartment and sinonasal cavity or middle ear ( Fig. 34.1 ). This conduit not only allows intracranial contents, cerebrospinal fluid (CSF), or the herniation of brain and meninges (i.e., meningoencephalocele) to egress through the defect , but also provides a route for sinonasal microbiologic pathogens to enter the sterile intracranial space. Minimally invasive endoscopic repair has largely replaced open craniotomy for defects of the MCF extending into the nasal cavity, though lateral defects are still commonly treated with middle fossa craniotomy, transmastoid approach, or a combined approach. Goals of successful endoscopic repair include identification of the location of MCF skull base defect, removal of causative pathology, and reconstruction of the skull base to prevent CSF leak. Additional goals include minimizing perioperative morbidity and maintaining long-term normal sinonasal physiology.
The MCF is centrally located in the skull base floor and is composed of the sphenoid bone and two temporal bones ( Fig. 34.2 ). Anteromedially, it is bound by the limbus of the sphenoid, a bony ridge above the optic canals. Anterolaterally, it is bound by the lesser wings of the sphenoid. The petrous portion of the temporal bone forms the posterolateral border, and the dorsum sella forms the posteromedial boundary. The floor of the MCF is formed by the body and greater wing of the sphenoid as well as the squamous and petrous parts of the temporal bone. The tegmen is a thin lamina of petrous temporal bone that covers the tympanic and mastoid cavities. It is composed of the tegmen tympani; the roof of the tympanic cavity; and the tegmen mastoideum, the roof of the mastoid cavity.
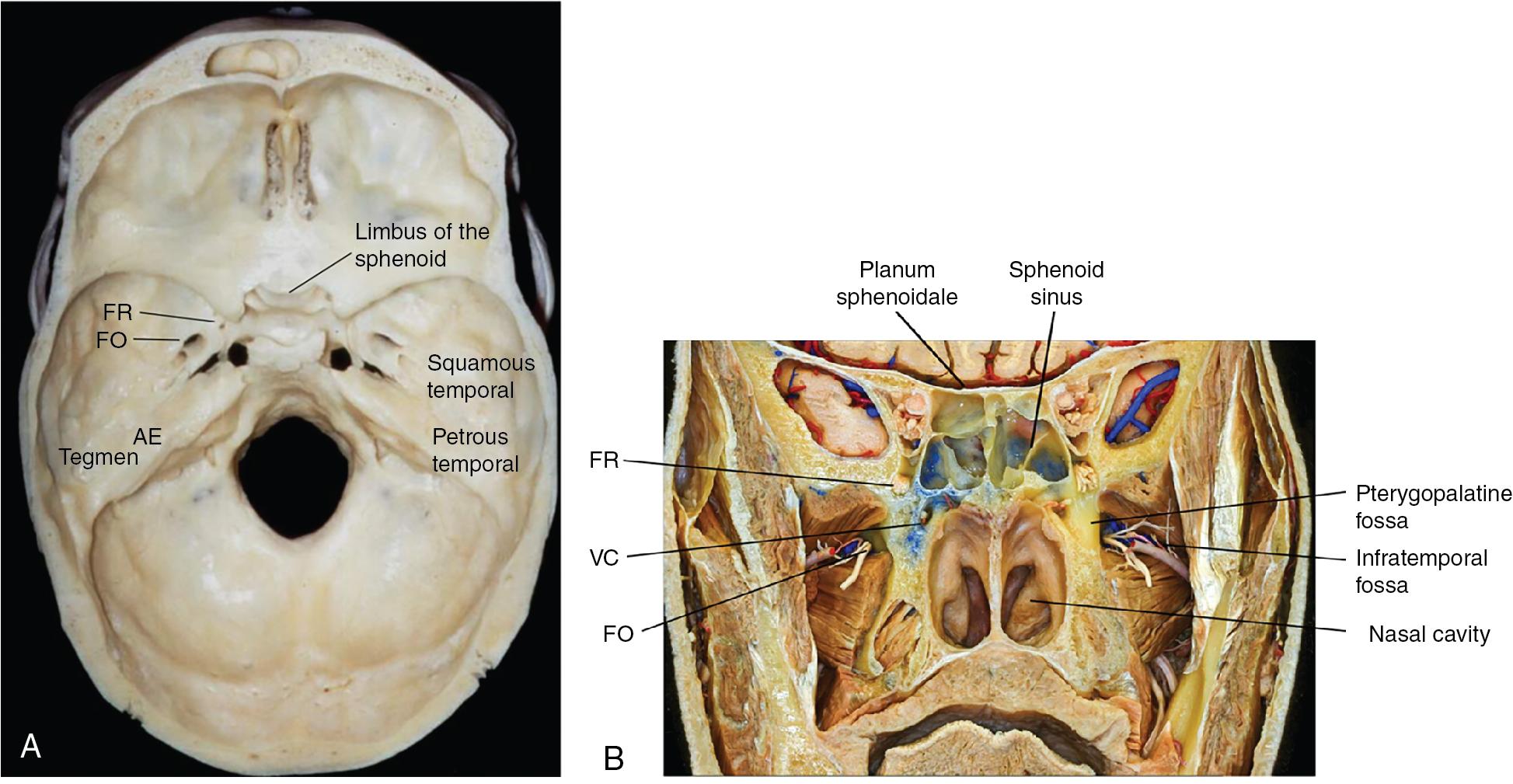
The central portion of the MCF forms the sella turcica and contains the pituitary gland. Anteroinferior to the sella is the sphenoid sinuses, a paired, aerated mucosa-lined cavity that drains into the sphenoethmoidal recess and nasal cavity through the paired sphenoid ostia. Of note, the ostia are positioned approximately in the upper third of the anterior face of the sphenoid sinus, relatively close in height to the planum sphenoidale. Variants of the sphenoid sinus anatomy include asymmetrically sized sphenoid sinuses, eccentric position of the intersinus septations (including over the vertical segment of the internal carotid artery), and multiple partitions (partial or complete) creating more than two sphenoid sinus cavities. Multiple anatomic variations of the sphenoid sinus pneumatization are described. In patients with sellar pneumatization, the preservation of air anterior and inferior to the sella creates the typical rounded appearance of the sella in the sphenoid sinus (80%). Presellar pneumatization is defined by the presence of an air space only on the anterior surface of the sella. The lack of a rounded, inferior air space results in a flat appearance of the sella (20%). In the conchal variant, the sella is encased in clival bone and is not directly visible upon opening of the sphenoid sinus (<1%). An important additional variant relates to the degree of lateral pneumatization of the sphenoid sinus air space. Patients with elevated intracranial pressure (ICP) with far lateral pneumatization (beyond V2) may be at heightened risk for development of a skull base defect in this region. The lateral part of the MCF is formed by the greater wings of the sphenoid bone and the squamous and petrous parts of the temporal bones and supports the temporal lobes of the brain.
The MCF has several important fissures that allow the natural passage of important structures to adjacent spaces such as infratemporal and pterygopalatine fossa, which are paired spaces located on either side of the anterolateral middle cranial base. The pterygopalatine fossa opens laterally through the pterygomaxillary fissure into the infratemporal fossa and medially through the sphenopalatine foramen to the nasal cavity. The foramen rotundum, which contains the maxillary division of the trigeminal nerve (V2) opens into the pterygopalatine fossa. The vidian canal, which carries mostly parasympathetic innervation to the lacrimal gland, nasal cavity, and palate, opens through the pterygoid process below and medial to the foramen rotundum. The foramen ovale, which contains the mandibular division of the trigeminal nerve (V 3 ), opens into the infratemporal fossa.
The causes of osseodural MCF defects may be divided into congenital, acquired, and spontaneous. Acquired defects are most common and include acute trauma, iatrogenic injury, neoplasia, and infection. , Defects may also have multifactorial causes such as chronically elevated ICP compromising skull base structurally weakened by remote trauma or prior infection.
Tumors commonly occurring in the middle fossa are meningiomas or schwannomas arising from meninges or cranial nerves, respectively. Chordomas and chondrosarcomas are rare and may arise from the bone and cartilage. Other tumors, such as nasopharyngeal carcinoma, esthesioneuroblastoma, lymphoma, and systemic metastasis, can originate from extracranial tissues and secondarily invade the MCF structures. Lateral MCF defects may be secondary to chronic otitis media with or without cholesteatoma, head trauma with temporal bone fracture or previous otologic surgery or may occur spontaneously. Importantly, the majority of previously classified central and lateral “spontaneous” meningoencephaloceles are now understood to represent a secondary manifestation of elevated ICP.
Congenital defects of the tegmen tympani develop ventral to the geniculate ganglion and may be caused by incomplete ossification of the tegmental process of the otic capsule or inadequate closure of the petrosquamous suture. It was originally thought that ventrally located congenital defects were caused by incomplete fusion of precursor sphenoid wings to the basisphenoid and presphenoid, leading to the formation of the lateral craniopharyngeal canal of Sternberg. , Maximilian Sternberg described the course of the canal as originating between the lesser sphenoid wing and sphenoid body posteriorly, running along the lateral wall of the sphenoid sinus, medial to foramen rotundum, medial to the vidian canal, and ending anteriorly at the vaginal process of the nasopharynx. He noted that a persistent canal is almost ubiquitously present in the skulls of 3 to 4 year-old children and in approximately 4% of adult skulls. , However, radiographic and anatomic studies have found that the location of spontaneous CSF leaks occur lateral to foramen rotundum and thus are not caused by a true Sternberg’s canal. , It is widely accepted that the development of CSF leaks in this region is the result of lateral recess pneumatization, attenuated sphenoid sinus recess roof and skull base, and the development of arachnoid pits from underlying intracranial hypertension (IIH). True congenital encephaloceles are rare in developed countries and may be related to neural tube defects and inadequate folate supplementation. They may be transtemporal or transsphenoidal and associated with coexisting abnormalities of the face, optic system, and brain. The vast majority of congenital lesions are diagnosed and repaired at birth.
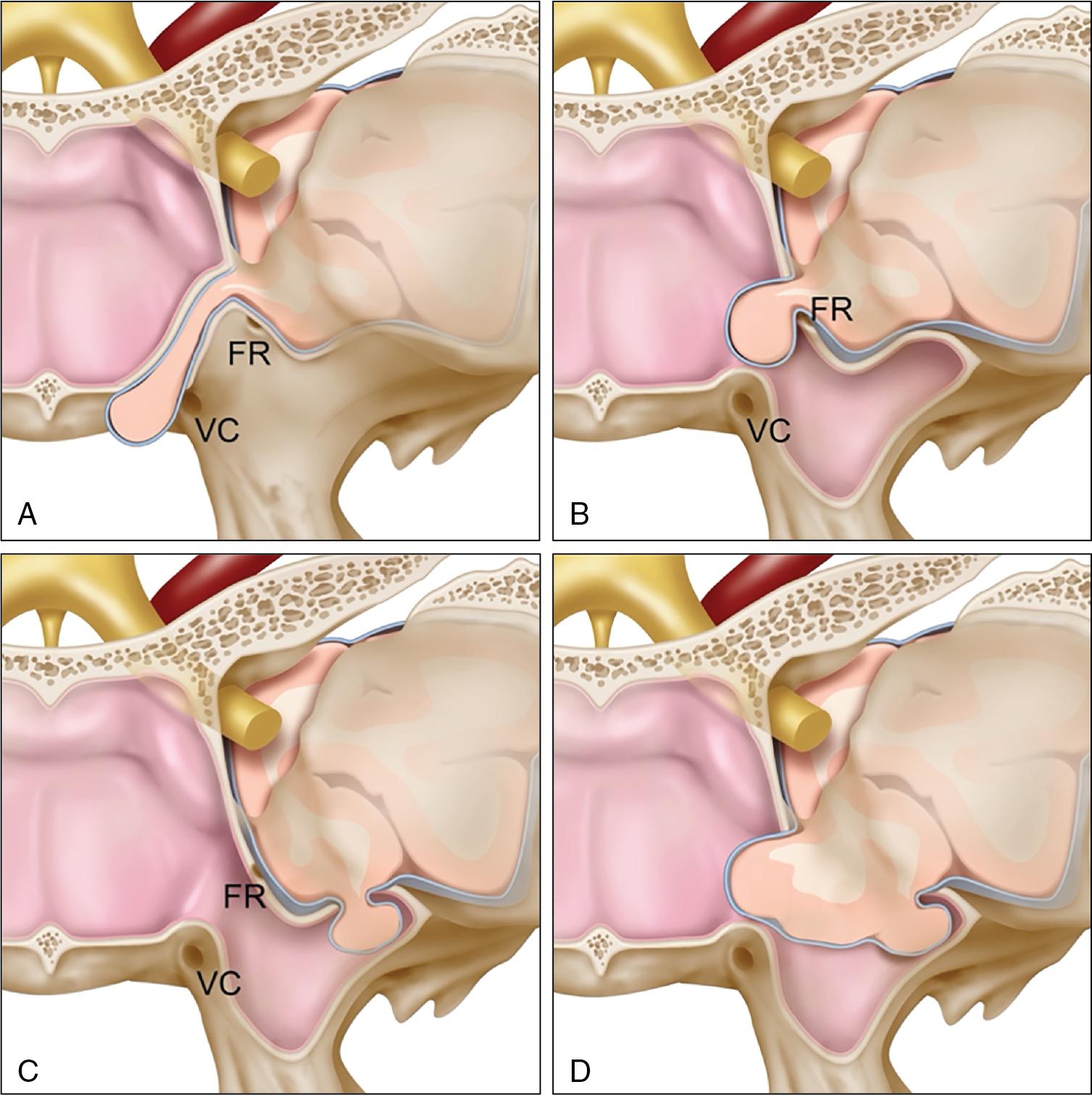
The most commonly reported locations for development of meningoencephaloceles are the cribriform plate, lateral recess of the sphenoid sinus, and tegmen tympani. Less frequent locations are the roof of the eustachian tube, midline sphenoid sinus, and posterior temporal bone. Further study of defects in the lateral recess of the sphenoid sinus have been identified at four main anatomic locations. Type 1 is an ideal Sternberg’s canal defect that begins medial and superior to foramen rotundum and passes medial to the vidian into the nasopharynx ending at the level of the vaginal process ( Fig. 34.3 A). Type 2 begins medial to foramen rotundum and passes into the sphenoid sinus ( Fig. 34.3 B). Type 3 starts lateral to the foramen rotundum and herniates into the sphenoid sinus ( Fig. 34.3 C). Type 4 herniates through an enlarged foramen rotundum into the sphenoid sinus and is located both medial and lateral to the foramen rotundum ( Fig. 34.3 D).
The presentation and patient demographics of the skull base defect depend largely on the location and cause. Meningoencephaloceles may be found incidentally or may present with vague symptoms, including nasal congestion or obstruction, CSF rhinorrhea, or headache from mass effect. Skull base defects enabling temporal lobe herniation may be particularly susceptible to seizure, a phenomenon that is unique to the MCF. Seizures are presumed to be related to either traction effect and irritation of the glial tissue herniating through the skull base defect or by coexisting cortical dysplasia. Tumors of the MCF may present with mass effect or cranial nerve involvement, leading to ptosis or impaired ocular motility.
An osseus defect is often accompanied by compromised dural integrity, resulting in CSF leak. CSF leaks manifest as clear, unilateral otorrhea or rhinorrhea and are often the only presenting symptom to indicate an underlying pathology. The open conduit from a CSF leak may allow intracranial migration of sinonasal microbiologic pathogens, potentially resulting in meningitis, encephalitis, or brain abscess formation. , Patients with a tegmen dehiscence may report aural fullness, hearing loss, tinnitus, imbalance, and headaches. Clinical examination may reveal a clear middle ear effusion, otorrhea, rhinorrhea, or pulsatile movement of the tympanic membrane.
Patients with “spontaneous" CSF leaks are often noted to have elevated ICP, usually attributed to idiopathic IIH. Such a strong correlation exists between spontaneous CSF leak and IIH that the literature recognizes many spontaneous CSF leaks as a clinical variant of IIH. Classically, these patients are often women of middle age with an elevated body mass index (BMI) and exhibit radiographic sequelae such as empty sella, flattening of the posterior globes, or transverse sinus stenosis.
Obesity is thought to increase intraabdominal and intrapleural pressures, which decrease venous return from the brain, resulting in elevated CSF pressure. Over many years, chronically elevated ICP may lead to erosion and thinning of the skull base. Similarly, it is thought that ICP spikes during apneic events associated with obstructive sleep apnea (OSA) contribute to skull base erosion over time. , BMI was found to have a linear relationship between ICP and is significantly higher in patients with spontaneous CSF leaks compared with those with other CSF leak causes. Additionally, spontaneous leaks have been associated with a higher rate of encephalocele formation, presumably secondary to increased ICP that remodels the weak and thinner bone of the skull base.
There are two common clinical presentations of IIH. In patients with actively elevated ICP, classic symptoms at presentation include headaches, blurry vision, and pulsatile tinnitus. Interestingly, internal decompression may mitigate any ICP-type symptoms in patients with herniation of meningoencephalocele contents into an open airspace (e.g., sphenoid sinus) or active CSF rhinorrhea.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here