Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Severe upper extremity and hand injuries have significant morbidity and economic impact. Recovery may be long and complicated, placing the patient and his or her livelihood at risk.
Significant improvements in the surgical outcomes of mutilating upper extremity injuries have been the result of not only the wide dissemination of microsurgical techniques but also the maturing of surgical strategies. Management now focuses on reconstruction of global hand function instead of individual fingers and structures. Large soft tissue defects that would have required prolonged healing times and dressings or the need for immobilization with regional flaps can now be reconstructed early in a single stage with free tissue transfer, reducing morbidity and often the cost of care.
The aim of emergency microsurgery of the upper extremity should be, in mutual agreement with patients, to restore reasonable hand function such that patients are able to resume their regular lives as soon as possible.
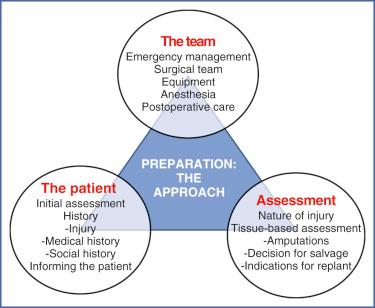
This chapter aims to provide the microsurgeon a framework for which to (a) prepare his or her team, (b) assess the upper extremity and (c) efficiently reconstruct a patient's hand to restore function and livelihood.
Critical arterial repai r—restoration of arterial inflow only, without which the injured part will not survive
Revascularization —restoration of arterial inflow and venous outflow
Major replantation —replantation of amputations proximal to the radiocarpal joint
Replantation —reattachment of a completely amputated body part, including restoration of arterial inflow and venous outflow
Reconstruction —repair and/or restoration of a body part with the goal of returning form and function
The approach should begin with accurate patient assessment (person and injury), setting realistic surgical goals (starting with the end in mind), and a well-prepared team of nurses, anesthetists and surgeons ( Fig. 2.1 ).
In microsurgical emergencies, one does not choose the patient, the injury nor the time at which the repair, replantation or reconstruction must be done. The patient may present with a localized hand injury or be moribund with multitrauma sustained in an accident. The decision to salvage the limb must be balanced with lifesaving measures.
Although the principles of microsurgery remain the same, the approach in emergencies is more rigorous. There is an acute need for swiftness and efficiency with clear and practical decisions. An unprepared surgeon may add to the morbidity of the patient with hesitation and poor decision making. This may arise from a lack of confidence, leading to an overconservative approach. Conversely an overconfident surgeon may attempt overly ambitious surgery, which can lead to a prolonged recovery period with multiple repeat procedures.
When faced with a complex injury of the upper extremity, it is imperative to form a plan that has the end result in mind. This will help to focus energy and surgical choices toward a specific goal without waste. The best outcome for an individual patient should be the guiding principle. Crucial factors such as handedness, occupation and time to recovery have to be kept in mind, and this is specific to any patient. Critical points in the pattern of injury need to be elucidated because these will determine indications for surgery and the sequence of operation. Last, but not least, the availability of a well-trained surgical team equipped in managing bone, soft tissue and neurovascular injuries of the upper extremity is absolutely necessary, without which the operation is doomed to failure.
The emergency microsurgery process starts at the prehospital and emergency department stage. Paramedics, along with emergency physicians and nurses, should be familiar with handling patients with upper extremity amputations and mutilating injuries.
The first step is to stabilize any hemorrhage without compromising the limb further. Moist dressings should be applied to the stump to provide firm pressure without desiccation of tissues. Massive hemorrhage can be controlled with prudent use of a tourniquet, for which position and time of application must be prominently marked. Tourniquet time should not exceed 2 hours.
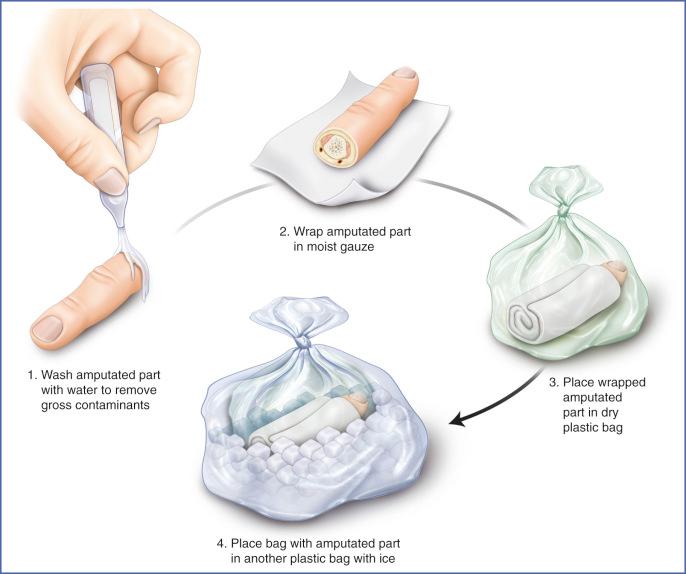
The next step is preservation of the amputate (amputated segment). Any devascularized body part should be preserved in a cold environment, reducing the warm ischemia time and increasing chances of reconstructive success ( Table 2.1 ). In an amputation this would comprise wrapping the amputate in a gauze moistened with normal saline, placing this in a waterproof plastic bag, and placing this bag in a container or another bag with ice ( Fig. 2.2 ). The aim is to avoid maceration or ice crystallization of the amputate. It must be remembered that the more muscle that is present in the amputate or devascularized part, the shorter the ischemia time.
| Level of amputation | Cold ischemia time (hours) | Warm ischemia time (hours) |
|---|---|---|
| Digit | 24 | 12 |
| Wrist to mid-forearm | 16 | 8 |
| Proximal forearm to lower-third arm | 14 | 7 |
| Proximal to mid-arm | 12 | 6 |
| Tissue | ||
| Skin and subcutaneous tissue | 12 | 6 |
| Muscle | 8 | 2 |
| Bone | 24 | 3 |
A basic history and examination should be performed and findings conveyed in a clear manner to the reconstructive surgeons ( Box 2.1 ). This will help the surgeons determine whether the part is salvageable and what preparations need to be done (eg, recall of a second team for multiple finger amputations). It is extremely helpful when pictures are taken and transfer of these images to medical colleagues across a secure network is possible.
Time of injury to establish ischemic time
Mechanism
Level of injury
Radiographic findings for the stump and amputate
Coexisting injuries
Hemodynamic status
Age
Handedness
Occupation and hobbies
Medical history (including diabetes and vascular diseases)
Current treatments and allergies
Tetanus status
Smoking history
From what time is the patient fasted for surgery?
Emergency personnel should not make a decision regarding the feasibility of replantation or limb salvage and should not have a discussion with the patient. The final decision making rests with the specialist reconstructive surgery team, and conflicting opinions can create confusion.
All crucial steps can be achieved by close communication and collaboration between the emergency department and the reconstructive surgery departments, including cross-department lectures, discussions and interaction.
Replantation and reconstruction should only be done in specialized centers with trained teams of doctors and nurses. Where possible there should be at least two experienced fully trained hand and reconstructive microsurgeons. This allows for a multiteam approach.
The residents and nurses should be formally trained in microsurgery. A valid training program consists of supervised establishment of basic skills, regular assessments and skills upgrades. As has been shown, all rotating residents in a reconstructive microsurgery residency program can be trained to be competent in the principles of microsurgery at low cost and effort.
Upper extremity injuries and amputations can happen at any time of the day, and surgeries are often long, especially in the case of multiple fingers or major limb replantation. Therefore in addition to the on-call team a standby team should be available to help with these procedures and enable a rotating roster of fresh well-rested surgeons. A specialist unit would also ensure that any secondary surgeries to improve function and appearance can be performed as necessary.
Magnifying loupes are essential for surgery of the upper extremity. There are many models available on the market, and the compromise is between magnifying power and field of view. Higher-power loupes are also heavier. A working distance of about 40 cm is comfortable for most surgeons. As a rough guide a magnification of 2.5 times (×) is sufficient for debridement and dissection of injured parts, flaps and grafts. Repair of fine structures should be done with 4× magnification. Repair of most nerves and vessels less than 2 mm should be performed with an operating microscope. This should have the capability of at least 5× to 24× magnification and two ports for surgeon and assistant. Familiarity with the microscope by all team members is best achieved in a systematic fashion and not during surgery. The entire surgical team from doctors to nurses should be familiar with the functioning of the microscope, and the microscope should be regularly maintained to ensure optimal performance at all times.
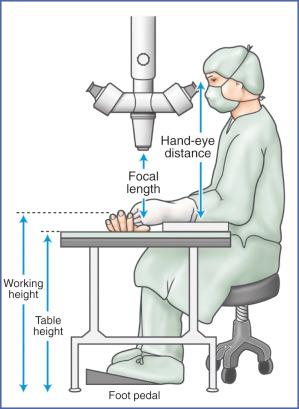
Basics of microscope etiquette include primary control of the microscope by the first surgeon, proper posture and comfortable hand position with a platform for resting the wrists. The first surgeon should always maintain control over zoom and focus of the microscope, positioning it in the position whereby he or she can achieve the best surgical outcome. This should be done with consideration to the assistant, informing the assistant of any shift in position and confirming that the assistant has adequate view of the field. Both surgeon and assistant should be seated upright comfortably and securely on a height-adjustable nonmobile stool, with ankles, knees and hips at 90 degrees and foot pedals within easy access ( Fig. 2.3 ). Finally, hand positioning is key to achieving good microsurgical outcomes. Rolled sterile dressing towels can be placed under the forearms and wrists to ensure minimal large muscle group interference with the delicate movements of the surgeon's fingers while manipulating the microinstruments.
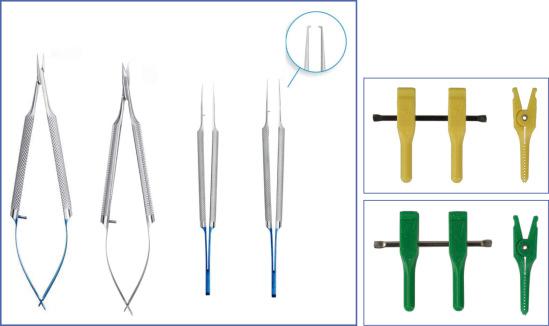
Microsurgical instruments should consist of (but are not limited to) microneedle holders, jeweler's forceps, vessel dilators, straight and curved microscissors and noncrushing microvessel clamps ( Fig. 2.4 and Table 2.2 ). In addition, irrigation systems with blunt tips (eg, syringe with a plastic cannula tip) should be available to aid in keeping the microsurgical field clear and avoiding tissue desiccation. Bipolar coagulators and/or microvessel clips are required for dealing with points of bleeding and side branches of vessels. Suction and sponges to mop up excess fluid are useful for keeping the surgical field dry. All instruments should be kept in excellent working condition and replaced regularly if required. A poorly functioning instrument can be of great frustration to the surgeon and can be responsible for suboptimal outcomes. In fact, changing a pair of jeweler's forceps is equivalent to the price of a suture, making a poorly functioning instrument a double cost liability.
| Item | Purpose |
|---|---|
| Microneedle holder (nonratcheted) | Manipulation of the microsuture |
| Jeweler's forceps (3 pieces) | Gentle handling of the soft tissue |
| Vessel dilator | Nontraumatic dilation of vessels |
| Microscissors—straight | Cutting microsuture |
| Microscissors—curved | Tissue dissection |
| Microvessel clamps (30-gauge) | Noncrushing stabilization of vessel ends |
Monofilament sutures ranging from 8-0 for larger vessels (eg, brachial artery) to 11-0 for distal digital neurovascular structures should be on standby for repair of vessels of differing diameters, depending on the level of injury ( Table 2.3 ). A moist gauze or pot of saline should be on hand to allow regular and convenient cleansing of instruments by the surgeon.
| Suture (monofilament) | Needle (µm) | Typical vessels |
|---|---|---|
| 8-0 | 130 | Radial, ulnar |
| 9-0 | 100 | Palmar |
| 10-0 | 75 | Digital |
| 11-0 | 50 | Children |
A well-trained anesthesia team accustomed to handling microsurgical procedures is a must in any upper extremity replantation and reconstruction center. It is of utmost importance to establish good communication with the anesthesia team the moment a replantation or microsurgical reconstruction is considered. This will enable:
minimal delay in getting the patient transferred to the operating theatre from the emergency department,
forewarning of a probable prolonged operation,
preparation of the relevant anesthetic agents and equipment, in particular the need for regional anesthesia, which helps with analgesia and sympathetic vascular blockade intra- and postoperatively,
conveyance of the patient's clinical status and whether invasive monitoring and/or blood transfusions are required,
essential padding for pressure points, including the occiput, sacrum and elbows, along with urinary catheterization.
Microsurgical procedures are often long, and once the patient is under anesthesia, he or she is relatively stable from an anesthetic point of view. The wise surgeon will keep the anesthetist engaged with timely questions as to the physiologic points that will directly affect an anastomosis. These are the patient's body temperature, adequate fluid filling seen by dilute urine in the catheter bag, adequate pain control seen by a normal pulse rate and blood pressure, and regular checks of estimated blood loss. Junior anesthetists should be warned not to give vasoconstrictors. Postoperatively the anesthetist can help with pain management and, in cases of massive trauma, help in intensive care management.
This is performed by well-trained nursing staff, doctors and relevant equipment. Postoperative care is just as important as the operation itself. Without adequate monitoring and a clear microsurgical protocol, even the most elegant of reconstructions can be doomed to failure.
In the immediate postoperative period the patient is preferably nursed in a microsurgical intensive care or high-dependency unit where trained nursing staff can help monitor both patient and reconstructed extremity. The on-call resident doctors also play a role in regular monitoring and should be taught to recognize early signs of trouble, such as decreasing temperature, color and turgor. Equipment such as warmers, handheld Doppler and dermal temperature monitoring should be available as required. If there is any sign of circulatory compromise, dressings should be loosened for inspection and redone as required. If vascular impairment cannot be rectified at the bedside, surgical facilities must be available for an immediate return to the operating room. More on postoperative monitoring is discussed later in this chapter.
Assessment of the patient should follow basic trauma life support principles. Although the hand surgeon is rarely the first physician to encounter the patient, it is important to bear in mind that there may be coexisting injuries in addition to that of the upper extremity. Patients with major amputations or mutilating limb injuries are often victims of major trauma and may have life-threatening injuries requiring more emergent treatment than that of the hand. The basic tenet of optimizing life before limb must not be forgotten.
General investigations such as blood tests and chest radiographs should be performed as required, and in particular, group and crossmatch of blood should be established in case blood transfusions are needed.
After ensuring that the patient's critical functions of airway, breathing and circulation are intact, a secondary survey should be performed. Once it is clear that the patient is stable, focus should turn to the upper extremity injury in question. The history taking should be efficient but should not miss essential information.
The time of injury must be established so as to precisely assess the ischemia time.
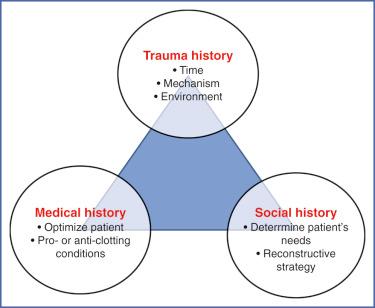
Knowledge of the mechanism gives an understanding of the extent and nature of injury and the contamination present. This helps define the extent of debridement and the need for grafts.
The environment in which the injury took place determines the likely tissue contaminants.
The patient's medical history must be ascertained, with the objective of optimizing preexisting conditions. It will also influence surgical decisions. Patients with diabetes have poor healing capabilities and are in a hypercoagulable state with elevated procoagulants and abnormal vascular endothelium. Hypertensive and hyperlipidemic patients may have brittle, calcified atherosclerotic vessels that, although more prevalent in the lower limb, can occur in the upper extremity. Patients with bleeding disorders or those on anticoagulants have a higher risk of large hemorrhage and postoperative hematoma formation and may require correction before surgery. A current history of smoking may be associated with poor replantation or microvascular outcomes. Heavy use of alcohol and preexisting psychiatric conditions should be included in the history because they help determine suitability for salvage.
In addition to occupation a thorough social and family history help guide surgical strategy. Jobs or hobbies requiring dexterous use of the hands (eg, manipulation of a musical instrument or surgery) have an obvious critical need for functioning fingers. On the other hand, manual laborers and the self-employed in many countries may not have the luxury of a prolonged absence from work and may opt for terminalization of a distally amputated digit rather than risk a protracted recovery period. Women, for social and esthetic reasons, may prefer replantation even without an obvious functional result.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here