Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The diseases in this chapter have dominant epidermal changes (clinical scaling, pathologic changes of spongiosis and parakeratosis), as opposed to rashes in 3, 4 , which primarily have dermal changes. It has been said by Levine that the diseases in this chapter are “outside jobs,” heavily influenced by external factors or contactants. Those in 3, 4 are “inside jobs” more heavily influenced by internal antigens. This is an interesting way to think of it, though obviously is oversimplified.
(see Fig. 2.1A–G )
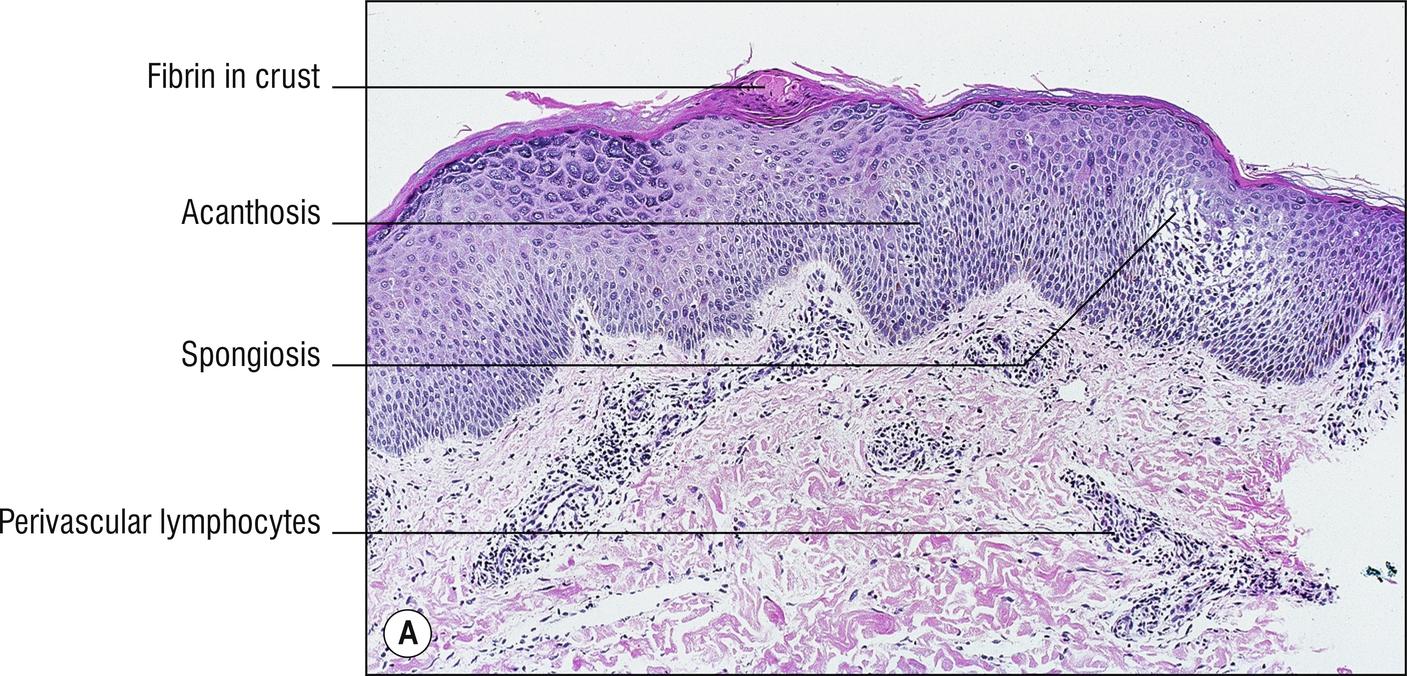
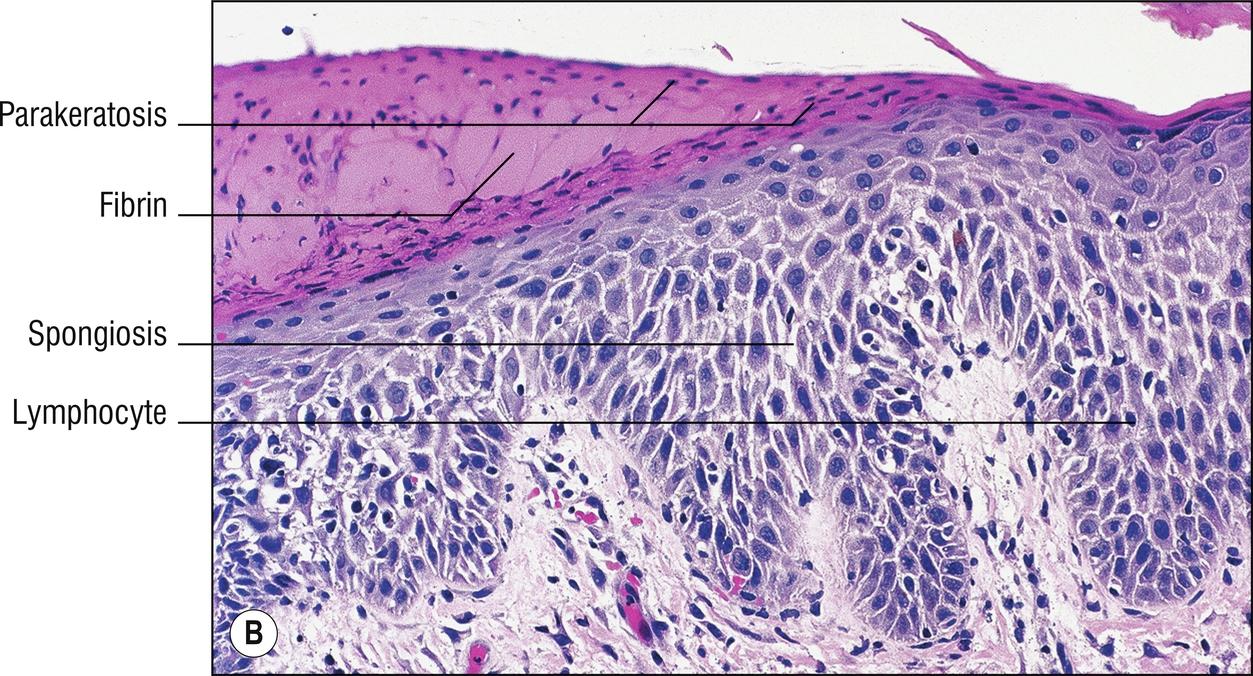
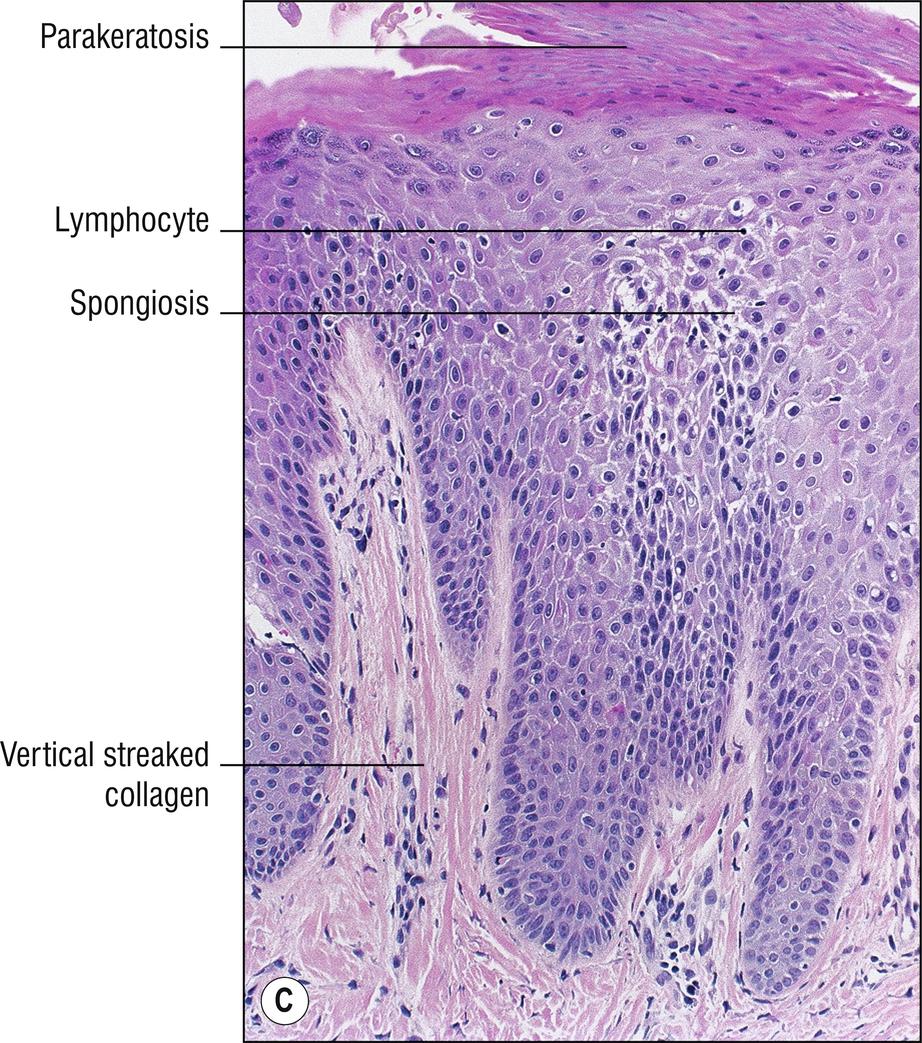
The term “eczema” has been criticized as being confusing, and difficult to define, but it is generally used by dermatologists to refer to a group of diseases characterized by diffuse, ill-defined scaling in their chronic stages, with spongiosis as an important feature histologically. Papulosquamous diseases (1.103) also have prominent scaling, but lesions are more sharply demarcated and more elevated. There is some overlap between the two groups. Clinicians often use the term “dermatitis” as a synonym for eczema, while others use it as a nonspecific term for any inflammatory skin condition (-itis means inflammation of). Patients with eczema often have pruritus (1.114).
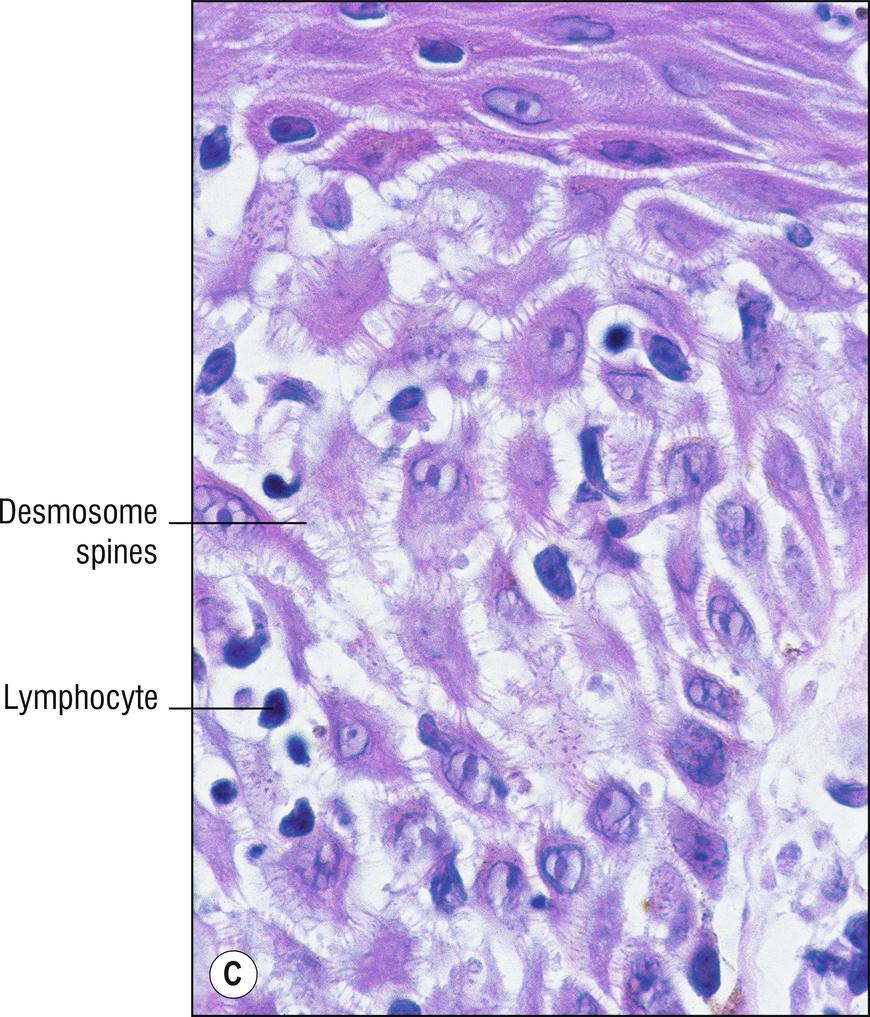
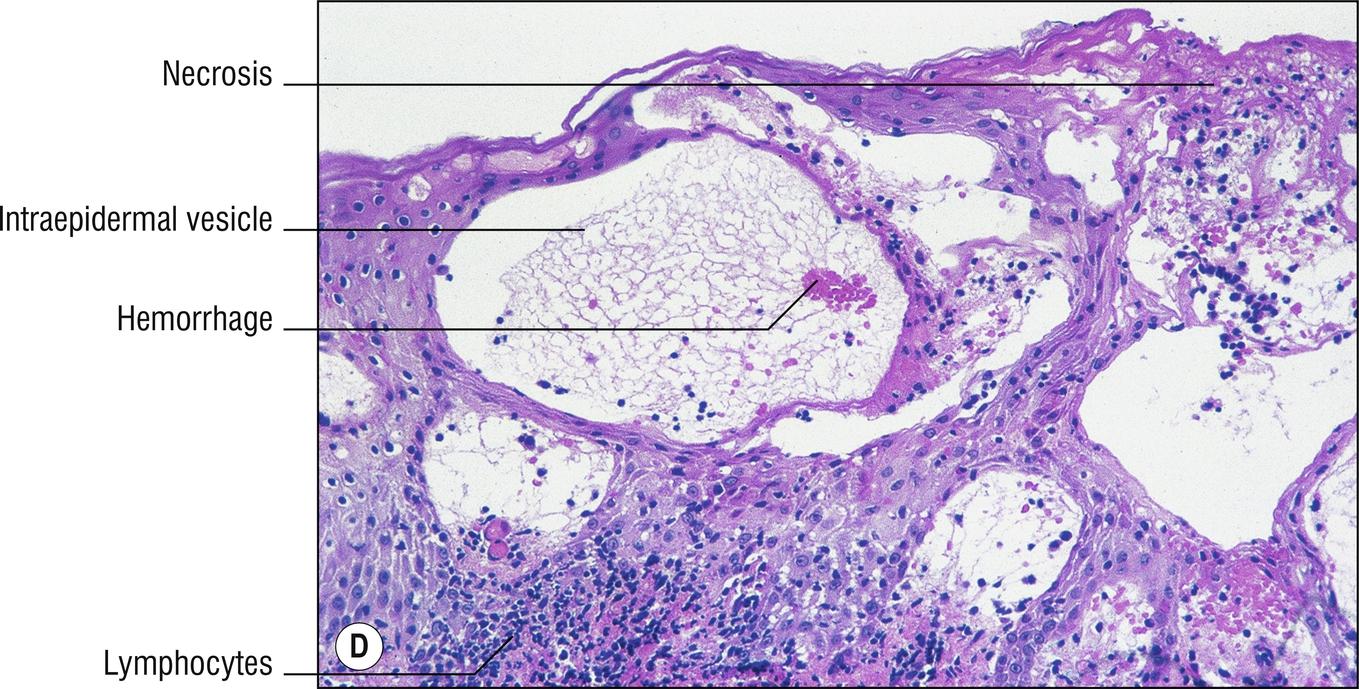
The histologic hallmark of eczema is spongiosis (1.9). Eczema in Greek means “to boil over,” referring to the small intraepidermal vesicles that may occur in eczematous conditions if there is enough spongiosis (intercellular edema). As eczema becomes more chronic, there is a tendency for it to become more acanthotic and less spongiotic. The antiquated terms “ acute dermatitis ” (intraepidermal spongiotic vesicle), “ chronic dermatitis ” (more acanthosis and less spongiosis), and “ subacute dermatitis ” (pathology in between acute and chronic) are best forgotten. In general, eczematous diseases are distinguished clinically rather than histologically, although a few minor helpful features are listed below.
Atopic eczema: onset in children after 3 months of age (more likely to be seborrheic dermatitis prior to that age), extremities , especially antecubital and popliteal, less involvement of the trunk, prominent on the face
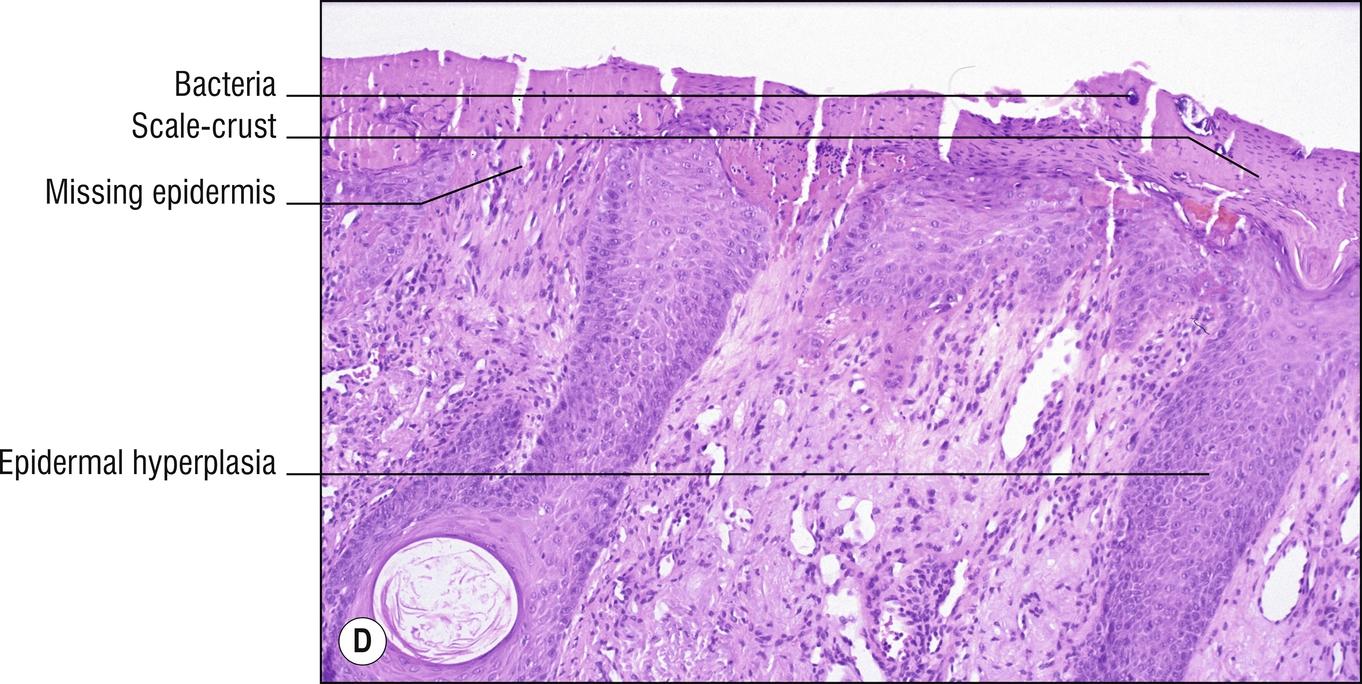
Focal parakeratosis , sometimes with crusting (1.104)
Neutrophils in the stratum corneum if secondarily impetiginized (1.89)
Acanthosis or hyperkeratosis sometimes (1.61, more if clinically chronic)
Spongiosis , sometimes spongiotic vesicles (more if clinically acute)
Superficial perivascular lymphocytes (1.109), occasional eosinophils
in infants (1.44), tends to resolve by adulthood in most cases, associated with asthma or allergic rhinitis , inhalant , and food allergies , often positive scratch tests or RAST tests, elevated serum IgE, no consistent distinguishing histologic features. Atopic means “out of place,” because the rash on the skin is out of place from the allergens that are primarily inhaled or consumed, rather than true allergy to substances in contact with the skin. Compare with contact dermatitis (2.2).
Xerotic eczema (dry skin, xerosis, asteatotic eczema, eczema craquele): no consistent distinguishing features.
Seborrheic dermatitis: dandruff , greasy scale of the scalp (1.124), eyebrows (1.42), eyelids (1.43), paranasal folds , axilla (1.10), or chest (and diaper area in infants), sometimes related to normal flora Malassezia globosa (formerly Pityrosporum ) yeast overgrowth (13.2); hence antifungals have been used as one of the treatments, sometimes associated with neurologic disorders or HIV virus infection (14.12), no distinguishing histologic features except that it is often more psoriasiform (1.118), but with more spongiosis than is usual for psoriasis (2.8). Lesions with overlapping features of psoriasis are sometimes called sebopsoriasis . A heaped-up greasy scaly variant resembling asbestos is tinea amiantacea (not a true tinea, also called tinea fostaine , meaning “false” in French).
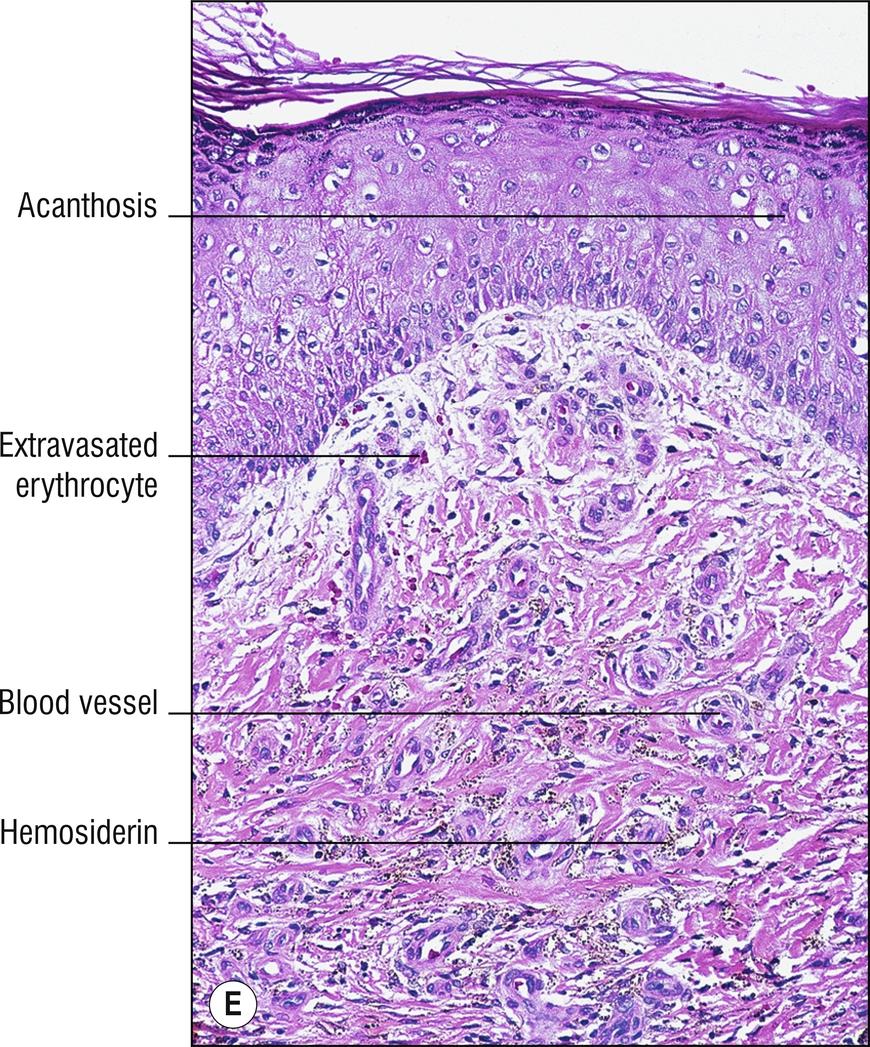
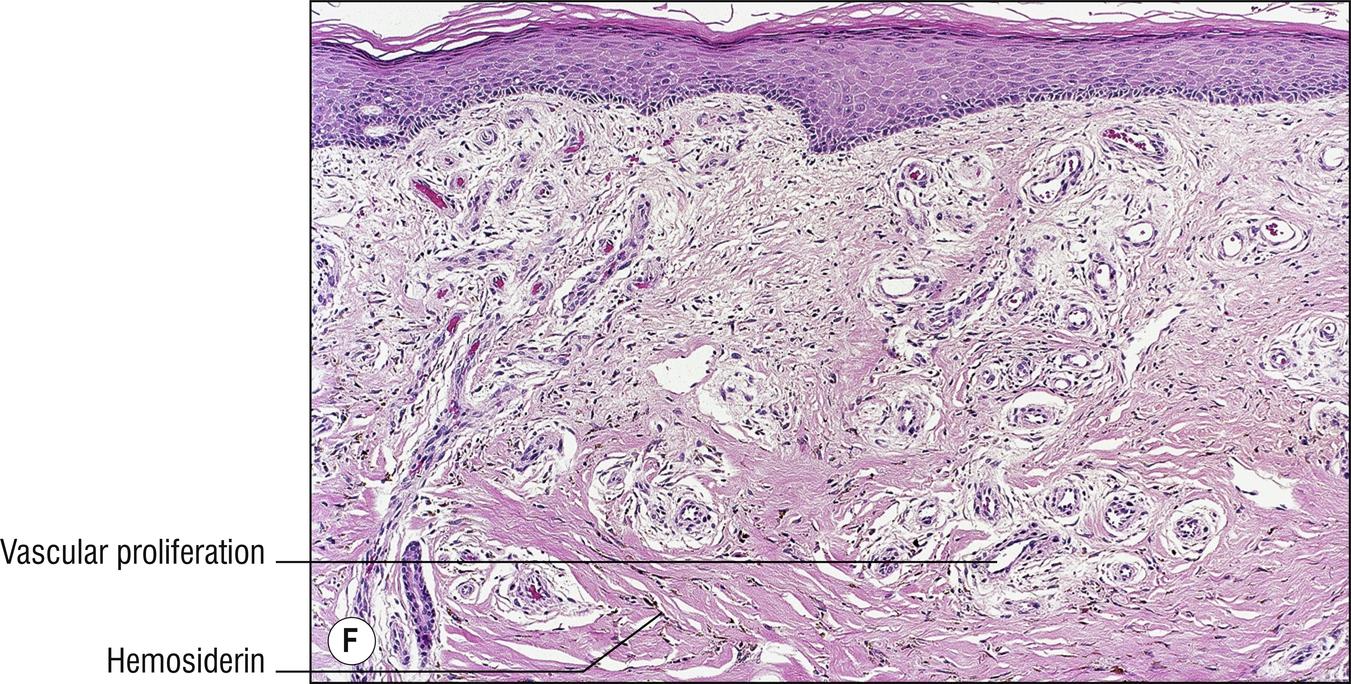
Stasis dermatitis: located on the lower legs (1.67), related to vascular stasis and venous valvular dysfunction, often more pigmented clinically (1.18), prone to develop stasis ulcers (1.142), more dilated papillary dermal small blood vessels and more hemosiderin (1.58); more fibrosis or sclerosing panniculitis in older lesions (16.9).
Acroangiodermatitis (pseudo-Kaposi sarcoma): variant of stasis dermatitis in which vascular proliferation is exuberant enough to be impressive clinically, sometimes resembling Kaposi sarcoma histologically (25.9).
Contact dermatitis: often included in the eczema group, and is discussed in more detail under 2.2.
Dyshidrotic eczema: scaling and microvesicles appear on the hands , fingers (1.56), toes, and acral skin (so named because “abnormal sweating” was previously thought to be related), often with “ tapioca-pudding ” grouped vesicles , more likely to show spongiosis and vesicles.
Id reaction: papules or spongiotic vesicles (often like dyshidrosis) erupt in a remote site such as the palms as a resulting reaction to a predominant rash elsewhere, such as tinea pedis (poorly understood, poorly documented immunologic phenomenon).
Papular eczema, follicular eczema: clinical terms for eczema that presents as tiny papules, resembling folliculitis (1.47), more common in pigmented races.
Neurodermatitis: this is a poor clinical term used when “neurosis” is thought to play a prominent role, excoriations often prominent, primary unmanipulated lesions usually not found, no distinguishing histologic features.
Nummular eczema: clinical term for rounded or annular (1.5) coin-shaped plaques (from same stem word as for numismatists, coin collectors), mostly on extremities, often with more crusting and spongiosis.
Wiscott–Aldrich syndrome, Omenn syndrome, and some other immunodeficiencies: often have clinical eczematous lesions and similar histology.
Vitamin deficiencies and metabolic disorders such as phenylketonuria, zinc deficiency (17.1), essential fatty acid deficiency, pellagra, Hartnup’s disease, biotin deficiency: may present with scaly, red skin like eczema, and have similar histology, but some may have more psoriasiform hyperplasia (1.119) or pale epidermis (1.99).
Keratolysis exfoliativa (lamellar dyshidrosis): a variant of palm and sole eczema (1.99) which has a peculiar advancing edge of peeling stratum corneum with central clearing, which patients cannot resist pulling off, and with relatively little or no erythema or inflammation.
Tinea (13.1): KOH prep, PAS stain, or culture positive.
Other eczematous diseases (1.29), papulosquamous diseases (1.103), and contact dermatitis (2.2).
Other spongiotic diseases (1.132), intraepidermal vesicular diseases (1.147), and perivascular dermatitis (1.109).
Langerhans microabscesses (pseudo-Pautrier microabscesses, monocyte microabscesses) occur commonly in the epidermis in eczema and contact dermatitis, positive for CDla or CD68, and can be confused with mycosis fungoides (24.1) and Langerhans cell histiocytosis (24.18).
Contact dermatitis is defined as a reaction to topical substances, and can be subdivided into irritant or true allergic (primarily type IV delayed hypersensitivity). It should not be confused with atopic dermatitis (2.1), which is a more systemic allergic problem. Common contactant allergens include neomycin, fragrance, preservatives in creams, rubber, nickel, formaldehyde, plants such as poison ivy, and many others. A careful history and allergy patch tests may be clinically useful to determine the cause. Juvenile plantar dermatosis is irritant contact dermatitis of the feet, often thought to be due to irritant contact dermatitis from moisture or occlusion by sweaty tennis shoes. Diaper dermatitis is usually an irritant contact dermatitis from feces and urine, but sometimes is due to Candida . Intertrigo is a term used for dermatitis in intertriginous areas such as the axilla (1.10) or groin (1.55) that is mostly an irritant contact dermatitis due to excessive moisture and friction, but some cases can be due to candidiasis (13.4) or erythrasma (12.5). Angular cheilitis ( perleche ) is sort of an intertrigo of the angles of the mouth, which is often associated with redundant folds that retain moisture, or poorly fitting dentures. Chronic actinic dermatitis ( persistent light reactor ) represents a persistent photocontact dermatitis. After chronic antigenic stimulation, the inflammation can become atypical, developing into actinic reticuloid , with Pautrier-like abscesses resembling cutaneous T-cell lymphoma (24.1), since the suffix -oid means resembling a reticulosis (an old name for lymphoma). Actinic reticuloid will often have factor XIIIa + multinucleated cells in the dermis, with plasma cells, eosinophils, and lymphocytes expressing a low CD4:CD8, sometimes less than one (normal is two). Histology and differential diagnosis for contact dermatitis is similar to eczema (2.1). Severe contact dermatitis and phytophotodermatitis (plant allergy in the presence of ultraviolet light, 1.110) may cause necrotic keratinocytes (1.86).
(see Fig. 2.3A–D )
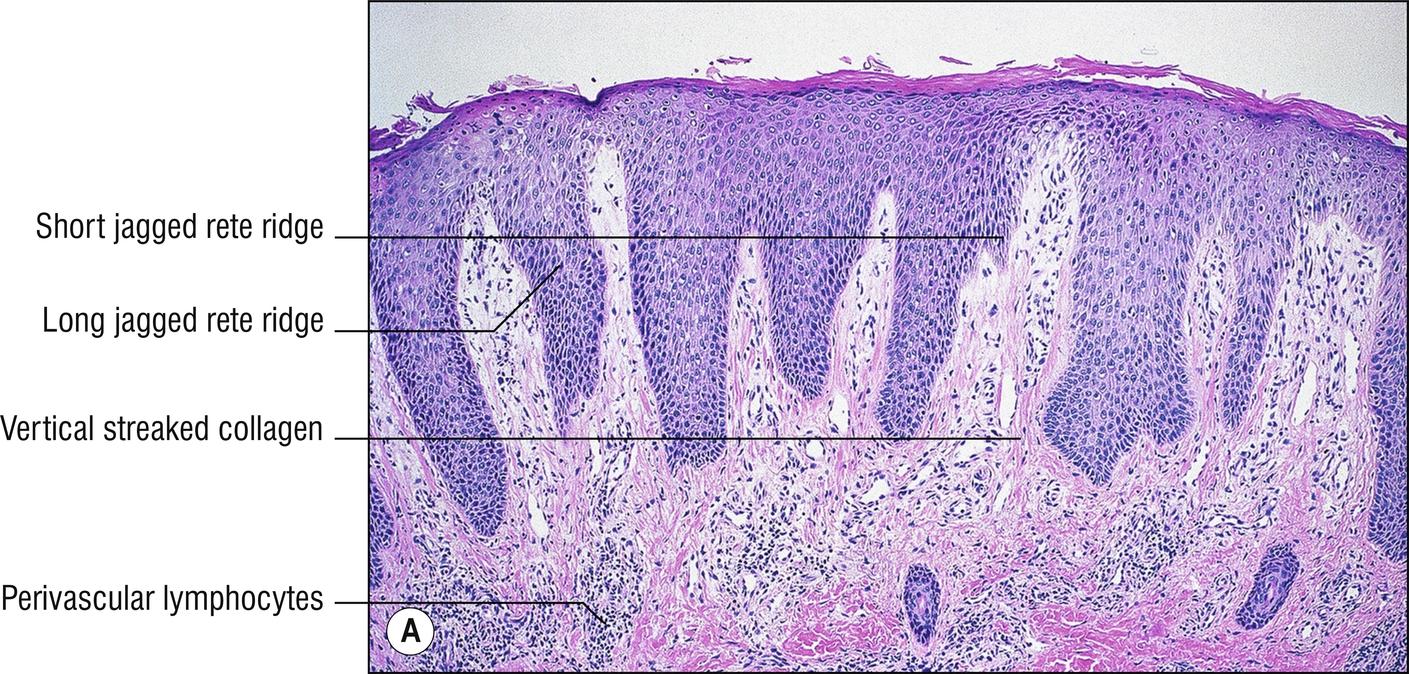
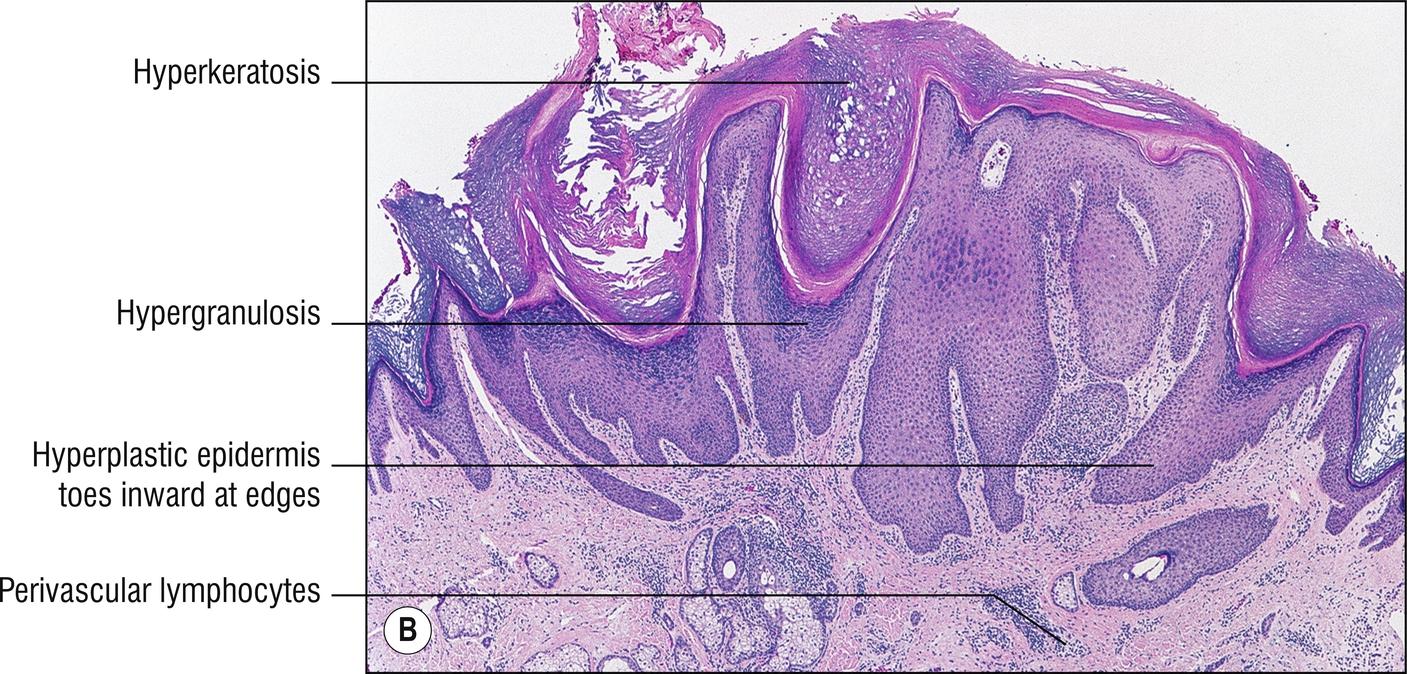
Lichen simplex chronicus (LSC) is a scaly, erythematous plaque that represents lichenified (thickened) skin due to simple chronic rubbing or irritation. It is lichenoid clinically, not histologically (1.72). Prurigo nodularis (picker’s nodule) is the same basic process, except that it is a localized nodule instead of a plaque. When many smaller papules are present, the less frequently used designation is prurigo simplex. In all of these patients, excoriations may be prominent also. Both conditions are end-stage lesions that usually start out as some kind of eczema, neurodermatitis, arthropod bite, folliculitis, or some other nuisance that causes the patient to pick or scratch an area of pruritus (1.113).
Hyperkeratosis with focal parakeratosis (1.104)
Hypergranulosis (1.60)
Impressive irregular acanthosis
Vertical orientation of collagen in dermal papillae
Perivascular lymphocytic infiltrate (1.109)
Prominent fibroblasts sometimes, occasionally multinucleated fibroblasts are seen (Montgomery giant cells) but they may also be seen in any chronic disorder
Enlarged nerves, occasionally, according to some authorities
Corn or callus: compact hyperkeratosis and acanthosis.
Frictional lichenoid dermatitis: papules or plaques of the elbows or knees from chronic friction. Lymphocytes more perivascular than lichenoid (it is lichenoid clinically, 1.72).
Acanthoma fissuratum (“granuloma” fissuratum): epidermal hyperplasia from chronic rubbing of spectacles on nose or post-auricular areas.
Other papulosquamous diseases (1.103) with hyperplasia of epidermis (1.61) or pseudoepitheliomatous hyperplasia (1.116).
Psoriasis (2.8): genetic inheritance, characteristic distribution of lesions, sharper clinical lesion demarcation, confluent (not focal) parakeratosis with neutrophils in mounds in stratum corneum, regular clubbed rete ridges that are not as pointed, no vertical orientation of collagen in dermal papillae unless chronically rubbed.
Pemphigoid nodularis: Prurigo nodularis features related to scratching itchy lesions of pemphigoid (6.1), often without blistering.
Epidermolysis pruriginosa: Epidermolysis bullosa dystrophica with prurigo changes (6.6).
Look for the primary lesions or conditions mentioned above, especially itchy ones (1.114).
(see Fig. 2.4 )
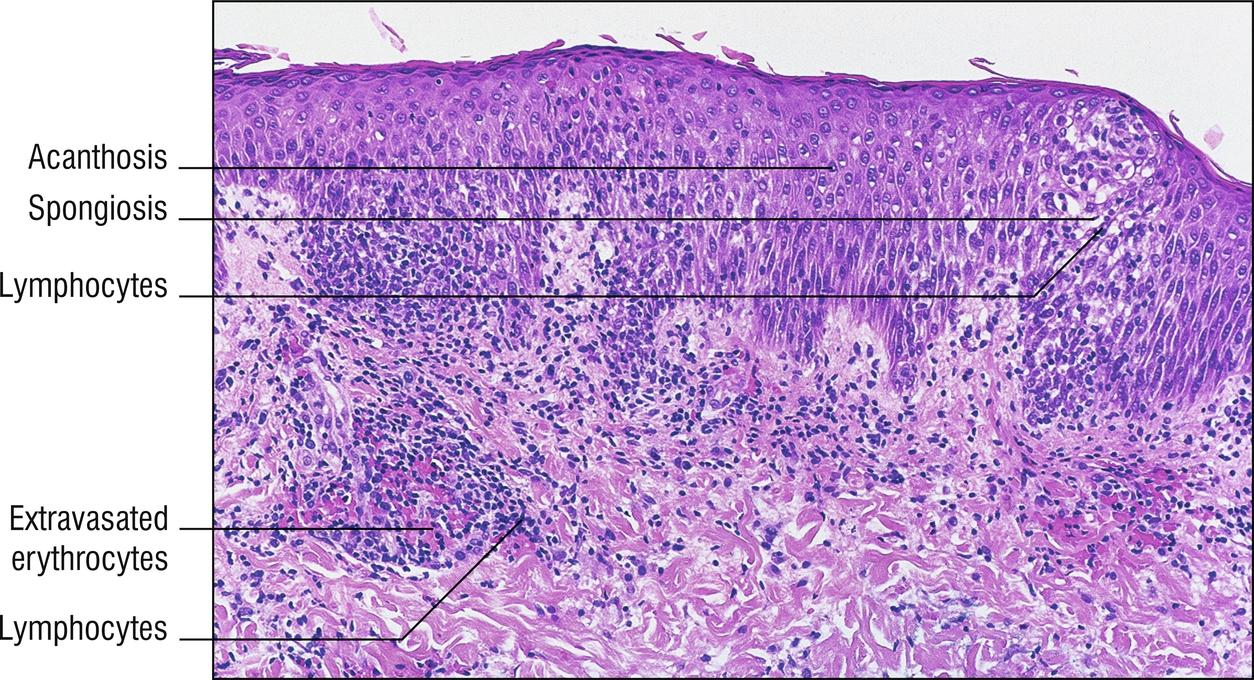
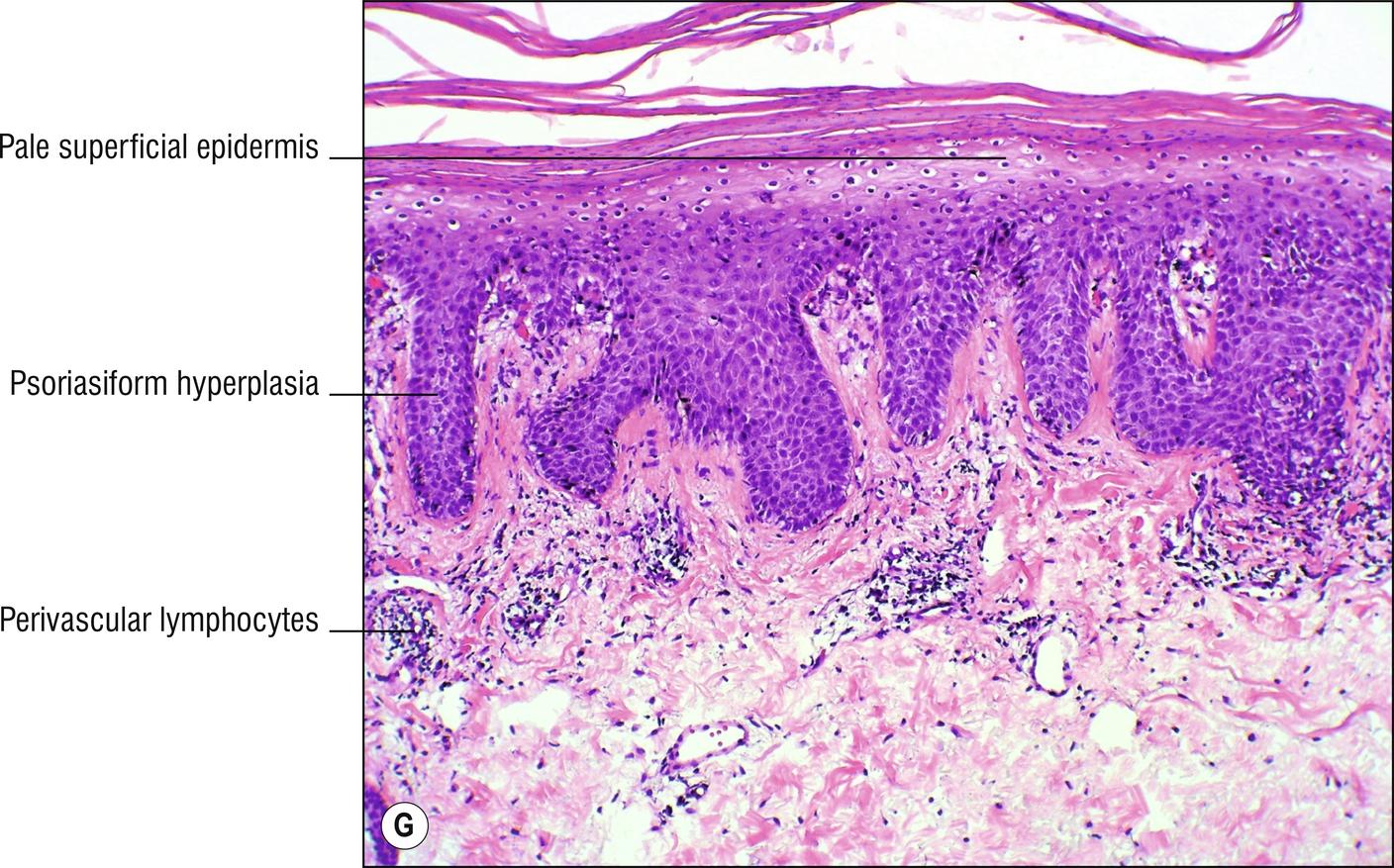
Common, papulosquamous , sometimes papulovesicular, sometimes pruritic (1.114), eruption of older children and young adults , beginning with an initial larger lesion (the herald patch ), often annular (1.5) and resembling tinea , often oval-shaped plaques in a “Christmas tree” distribution on the trunk (1.141), skin lesions resolve in 6 weeks. “Pityriasis” is an old term for flaky skin conditions with bran-like scale (from Greek “pityron”). “Rosea” just means red, but most rashes are red, frankly. PR has been considered possibly to be related to an infectious agent, but a large number of proposed etiologies have remained unproven. Sometimes drugs can cause a PR-like eruption.
Focal parakeratosis, sometimes in mounds (1.104)
Mild acanthosis sometimes (1.61)
Spongiosis (1.132); rarely spongiotic vesicles (1.147)
Perivascular lymphocytes ; rarely eosinophils (1.36)
Dyskeratosis sometimes (1.27)
Focal extravasated red blood cells sometimes (1.40)
The mnemonic SAMPLER has been used: Spongiosis, Acanthosis, Mounds of Parakeratosis, Perivascular Lymphocytes, Extravasated red blood cells.
Mostly is a clinical diagnosis. Not biopsied except in unusual cases.
Eczematous diseases (1.29), papulosquamous diseases (1.103).
Other diseases with spongiosis (1.132) or perivascular dermatitis (1.109).
Secondary syphilis (12.13): positive serology or stains for organisms.
Parapsoriasis (2.9): persists, does not resolve in 6 weeks.
Tinea (13.1): KOH prep, PAS stain, or culture positive.
PR-like rashes occur with some drugs (3.5) and with some forms of epidermodysplasia verruciformis (14.1).
(see Fig. 2.5 )
Uncommon, linear scaly plaque (1.73), sometimes hypopigmented (1.150), usually on one extremity of children , resolves in months to years.
Focal parakeratosis (1.104)
Mild acanthosis, sometimes psoriasiform (1.119)
Spongiosis
Dyskeratotic keratinocytes sometimes
Focal basal layer liquefaction sometimes (1.64)
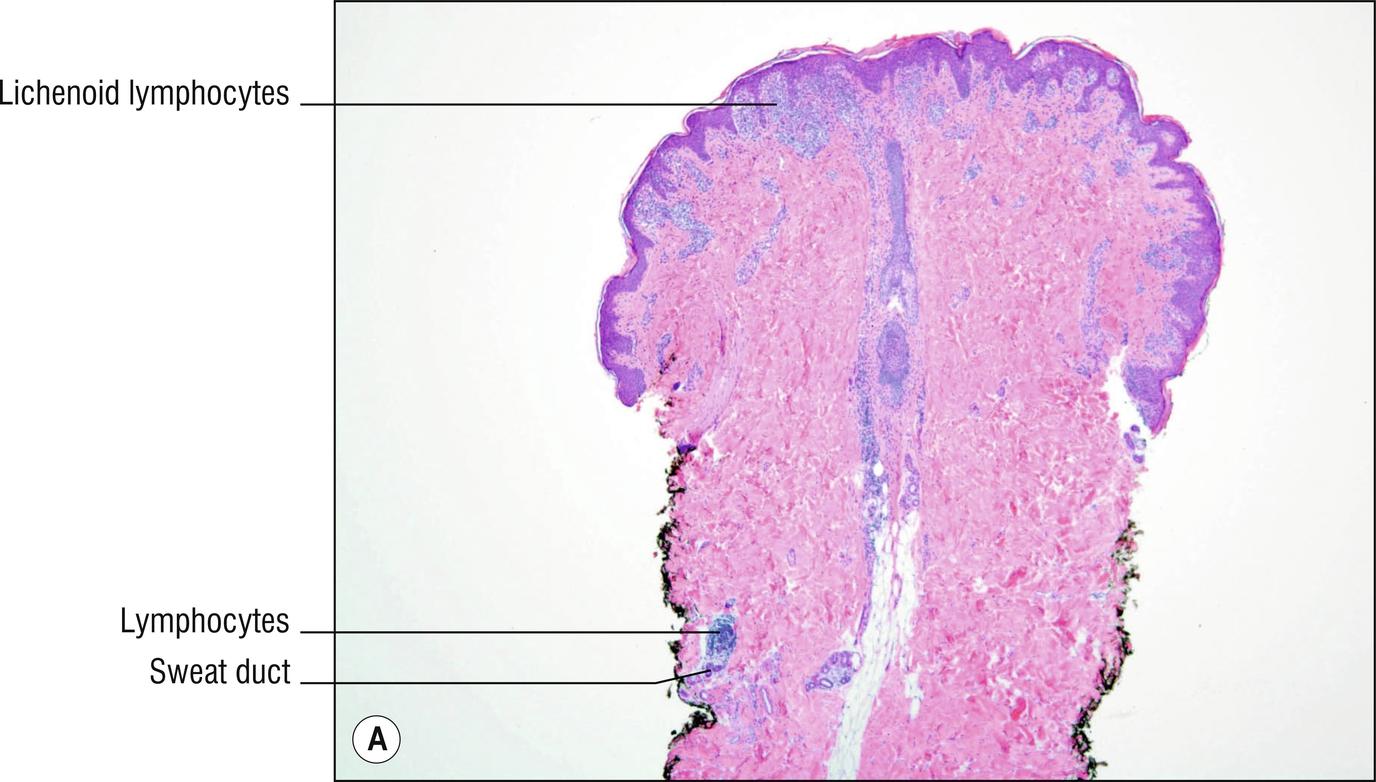
Perivascular (1.109) or lichenoid lymphocytes , often with inflammation around follicles and especially around sweat ducts ( syringocentricity )
“Eczema” (2.1) and other spongiotic diseases (1.132): rarely linear.
Other diseases with dyskeratotic keratinocytes (1.27): rarely linear.
Of other lichenoid diseases (1.72), linear lichen planus might be most difficult to distinguish (2.11) unless there are multiple other lesions.
Epidermal nevus (18.1): also linear, more likely to be congenital, persists indefinitely, more papillomatosis and acanthosis, less spongiosis or dyskeratosis unless irritated.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here