Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Eczema is a non-infective inflammatory skin condition that shows itching, redness, papulation and scaling. Eczema represents a reaction pattern to a variety of stimuli, some of which are recognized but many of which are unknown. Eczema and dermatitis mean the same thing and may be used interchangeably.
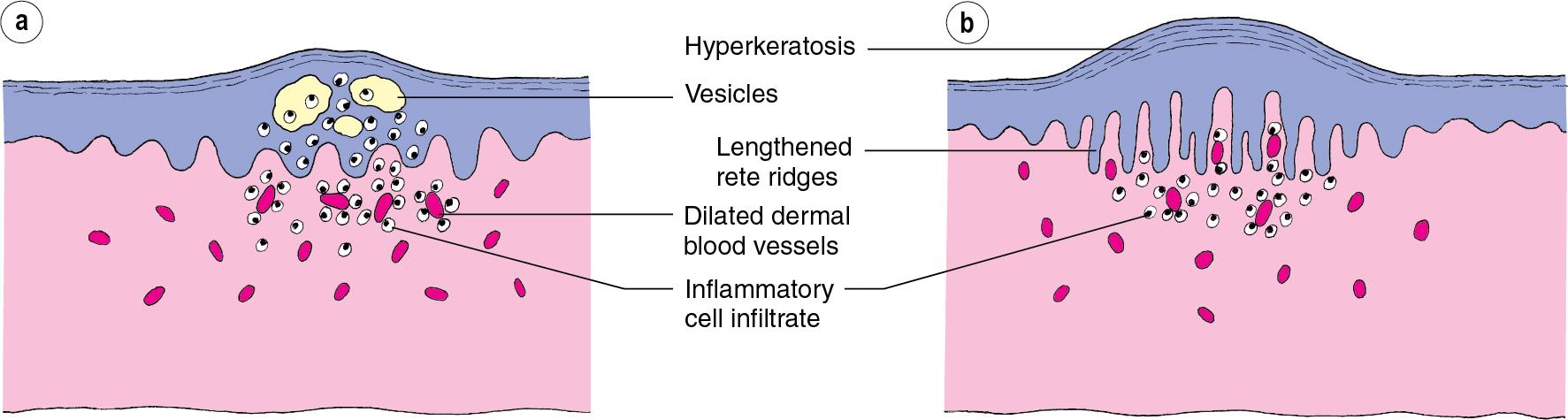
The eczemas represent a wide spectrum of conditions with varying prevalence and pathogenesis ( Table 19.1 ), clinical features ( Table 19.2 ) and management ( Table 19.3 ). The current classification of eczema is unsatisfactory in that it is inconsistent. However, it is difficult to provide a suitable alternative as the aetiology of most eczemas is not known. Different types of eczema may be recognized by morphology, site or cause. A division into endogenous (due to internal or constitutional factors) and exogenous (due to external contact agents) is convenient ( Table 19.4 ). However, in clinical practice, these distinctions are often blurred and, not infrequently, the eczema cannot be classified. A further division into acute ( Fig. 19.1 ) and chronic ( Fig. 19.2 ) eczema can be made in many cases according to the morphology of the eruption.
| ‘The eczemas’ | Prevalence | Sex predisposition | Pathogenesis |
|---|---|---|---|
| Atopic eczema | 10%–30% children; 2%–10% adults | Equal | Large genetic contribution, with dominant role of mutations in gene encoding filaggrin. Allergic responses play a role in disease flares. |
| Allergic contact dermatitis | 20% of the adult population are allergic to at least one contact allergen (most common nickel and fragrance, but increasingly methylchloroisothiazolinone) | Females more common | Not thought to have a large genetic component. Environmental exposure to allergenic chemicals is causative. |
| Seborrhoeic dermatitis | 5% prevalence, but lifetime incidence much higher | Males more common | Linked to overgrowth of natural yeast commensals (e.g. Malassezia furfur ) and sebum production. Exacerbated in HIV and Parkinson’s disease. |
| Discoid eczema | 0.1%–9.1% | Younger (<30 years) patients more commonly females; older patients more commonly male | Unclear, some may be triggered by local skin infections. |
| Venous eczema | Common amongst the 15% adults who suffer venous insufficiency | Equal | Venous hypertension, often due to valvular incompetence, leads to lower leg tissue oedema and extravasation of erythrocytes. This leads to chronic inflammation and itch. |
| Asteatotic eczema | Moderate–severe disease is uncommon, but mild disease is probably common | Equal | All skin dries with age, but low humidity, exposure to soaps, poor nutrition and impaired renal function are implicated in precipitating this condition. Probably mediated by defects in stratum corneum composition. |
| Irritant contact dermatitis | Estimated 1%–2% population | Females more common | Epidermal damage is central. Acute toxicity to keratinocytes (e.g. bleaches) or chronic damage to barrier by removal of lipids (e.g. solvents and detergents) account for different patterns of onset. Water exposure induces barrier disruption. |
| Pompholyx eczema | Estimated 0.1% population | Equal | Usually coexists with atopic eczema. Rarely, may be associated with tinea infections. Sweating is also a frequent exacerbator. |
| Juvenile plantar dermatosis | Rare | Boys more common | Typically arises in individuals with atopic background in winter. Exacerbated by occlusive footwear and following friction to the feet. |
| ‘The eczemas’ | Age of onset | Symptoms | Pattern |
|---|---|---|---|
| Atopic eczema | >50% under 2 years | Severe itch, often precluding sleep | Prominent involvement of flexures, but can be widespread. Often also the face and hands. Usually spares nose. Erythema, papules and scaling. Secondary excoriations, lichenification and infection may also be seen. |
| Allergic contact dermatitis | Most cases in adults, increasing prevalence in children | Itch, occasionally painful during severe reactions | Often well demarcated to area of allergen exposure (e.g. unilateral). However, often also hard to distinguish from atopic eczema. Certain sites show increased predisposition (e.g. face, genitals, hands, chronic wounds). |
| Seborrhoeic dermatitis | Infancy (<3 months) and adulthood (40–60 years) | Nil or minimal itch | Infancy—usually scalp involvement (cradle cap); plus variable skin (often flexures) and napkin area involvement; adult—usually scalp with variable face (eyebrows, nasolabial folds) and sternal involvement. |
| Discoid eczema | Most commonly after 50 years | Severe itch | Round (disc shaped) patches of eczema, usually confined to the legs and sometimes arms. |
| Venous eczema | Elderly | Itch | Usually bilateral, confined to the lower legs, with evident signs of venous hypertension. |
| Asteatotic eczema | Elderly | Mild–moderate disease often not itchy | Initially, involves lower legs with criss-crossed cracks and fissures in generalized dry skin. Can spread to other areas. |
| Irritant contact dermatitis | Any age, but infants and elderly more common | Itch and sometimes pain in acute cases | Restricted to area of irritant exposure. Often hard to distinguish from allergic contact dermatitis. Certain sites show increased predisposition (e.g. hands, finger webs). |
| Pompholyx eczema | Young adults most common | Severe itch arises at the onset of vesiculation, which gradually resolves typically over the course of a week and then leads to scaling and often fissuring. This may be a cyclical problem. | Classically, vesicles arise on the lateral margins of the fingers. However, more severe cases may involve the palms and soles. |
| Juvenile plantar dermatosis | 3–13 years | Discomfort due to cracking. Itching less prominent | Dryness and scaling restricted to the ball of the feet and plantar surface of toes. |
| ‘The eczemas’ | Treatment principles | Complications | Prognosis |
|---|---|---|---|
| Atopic eczema | Avoidance of triggers (including irritants and allergens), reparation of skin barrier (emollients), anti-inflammatories (topical corticosteroids, topical calcineurin inhibitors) and anti-infectives (as indicated) | Skin infections (bacteria e.g. Staphylococcus aureus ; virus e.g. Herpes simplex; fungus e.g. Malassezia furfur ) | Generally improves with age. |
| Allergic contact dermatitis | Avoidance of causative allergen | Secondary spread of eczema to non-exposed sites or systemic reactions may arise in severe cases. | Resolves completely with allergen avoidance. Occupational allergic contact dermatitis may require career change. |
| Seborrhoeic dermatitis | Mild topical corticosteroids are used in the acute stages, but maintenance treatment is with anti-yeast therapy (imidazoles) as shampoo or creams and emollients. | Not usually secondarily infected | Infantile disease usually resolves, whereas adult disease is usually relapsing and remitting. |
| Discoid eczema | Topical corticosteroids and calcineurin inhibitors are usually effective. Sometimes phototherapy or systemic treatment may be required. | Secondary infections are seen (usually Staphylococcus aureus ) | |
| Venous eczema | Topical corticosteroids help the acute inflammation, but maintenance treatment requires the venous incompetence to be addressed (e.g. compression). Daily emollients are helpful. | Venous ulceration is not a direct complication of the venous eczema, but may arise following trauma through scratching in atrophied skin. Prevalence of allergic contact dermatitis is increased in venous eczema. | Without correction of the underlying vascular defects, gradual deterioration is seen. |
| Asteatotic eczema | Intense emollient therapy. Corticosteroids are not required. | Responds well to treatment. | |
| Irritant contact dermatitis | Avoidance of irritants if possible, regular emollient use and short term corticosteroid application are likely to be helpful. | Often difficult to treat. Occupational irritant contact dermatitis may require career change. | |
| Pompholyx eczema | Potent topical corticosteroids at the outset of vesiculation are beneficial. Potassium permanganate soaks may also be beneficial. More severe cases may need intermittent systemic treatment. | Following vesiculation, the onset of fissures may be complicated by secondary infection. | Often prolonged problems for several years, but disease remission usually follows. |
| Juvenile plantar dermatosis | Emollient and breathable shoewear are helpful. | Infection may arise in fissures. | Generally improves with age. |
| Type | Variety |
|---|---|
| Exogenous (contact) | Allergic, irritant Photoreaction |
| Endogenous | Atopic Seborrhoeic Discoid (nummular) Venous (stasis, gravitational) Pompholyx |
| Others | Asteatotic (eczema craguelé) Lichen simplex (neurodermatitis) Juvenile plantar dermatosis |


Acute eczema almost always arises as a flare in those with a background of long-standing eczema, but can arise de novo in those exposed to a potent irritant. In acute eczema, epidermal oedema (spongiosis), with separation of keratinocytes, leads to the formation of epidermal vesicles ( Fig. 19.3 a). Dermal vessels are dilated, and inflammatory cells invade the dermis and epidermis. Clinically, acute eczema presents as a sudden onset of intense redness, itching and often pain arising over 24–48 hours. Frequently the individual notes that there is involvement beyond the typical sites of recurrent eczema. As described histologically, acute epidermal oedema is identified clinically as vesiculation, dilation of dermal vessels as redness. In severe cases, the vesiculation can become exudative.
Sudden acute flares of eczema can be triggered by viral infection (including Herpes simplex virus; eczema herpeticum) and bacterial infection (including Staphylococcus aureus ), and appropriate microbiological sampling should be taken and treatment commenced as indicated. Other causes include exposure to potent irritants (such as powerful detergents) and allergens (see p. 46).
Management of acute eczema requires urgent assessment of the potential cause and appropriate treatment for infection as indicated. However, in acute cases, it is also important to instigate effective anti-inflammatory treatment once infection is under treatment or has been excluded. Typically, this would involve topical corticosteroids (usually potent or super potent, guided by age and body site) or oral corticosteroids in severe cases. Continued regular application of greasy emollients is also important. Further detail is described in the relevant sections relating to the underlying cause.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here