Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
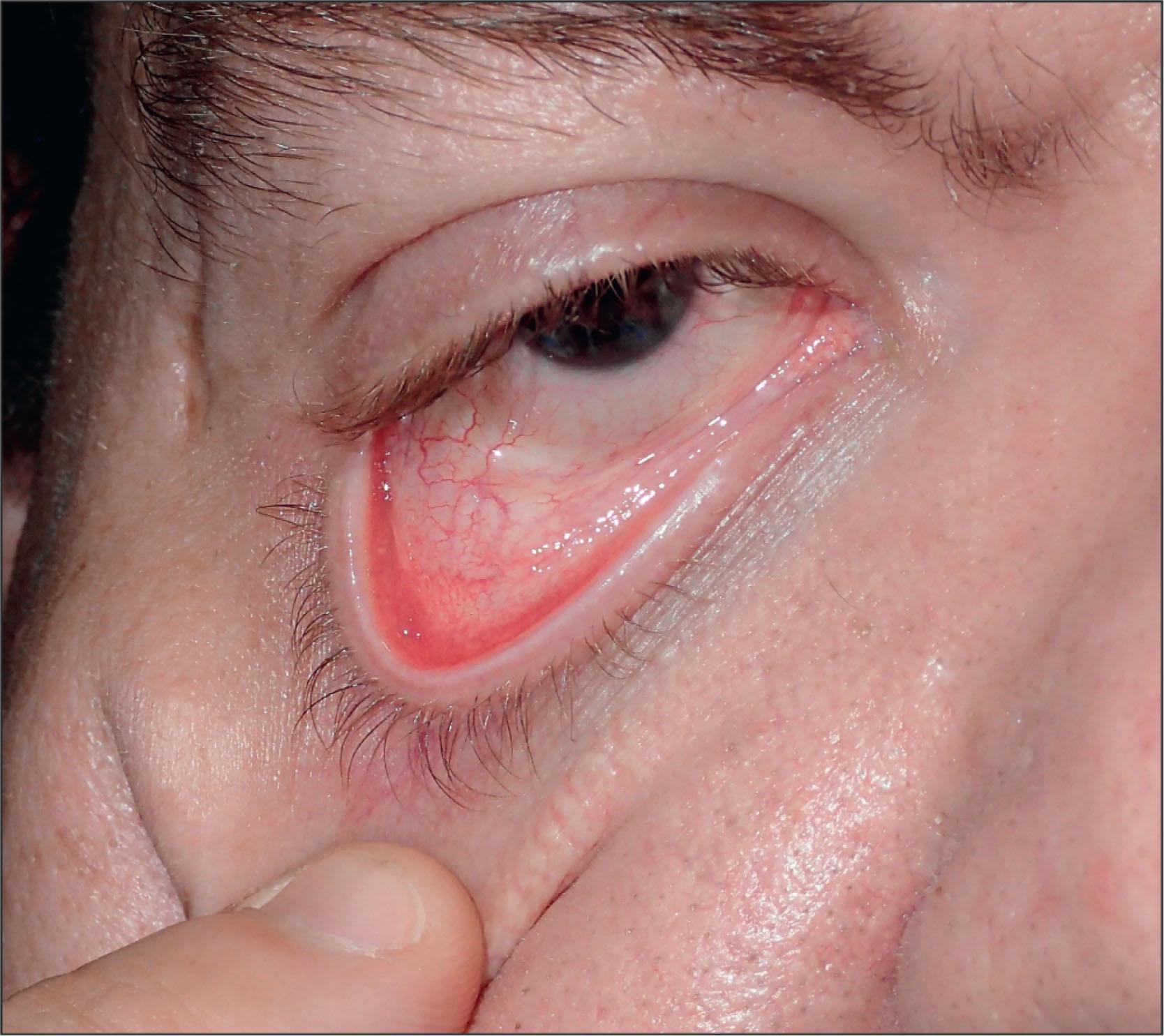
Ectropion is an outward rotation of the eyelid margin from the eye.
Ectropion may result from progressive age-related eyelid laxity, vertical skin shortening, orbicularis muscle weakness from facial nerve palsy, or mechanical force on the eyelid from a scar or tumor.
Lower-eyelid ectropion results in epiphora, palpebral and conjunctival surface irritation and keratinization, and corneal exposure with potential corneal ulceration and scarring.
Surgical correction aims to reestablish proper eyelid margin apposition against the ocular surface.
The most important surgical procedures include horizontal eyelid tightening, skin grafts, and in cases of facial palsy, lateral tarsorrhaphy or posterior lamellar shortening.
Epiphora.
Conjunctival erythema.
Exposure keratopathy.
Ocular surface pain.
Ectropion is an outward rotational displacement of the eyelid margin that is frequently encountered in clinical practice. This eyelid malposition most commonly affects the lower eyelid but can also occur in the upper eyelid. Clinically, it is important to identify the etiology of ectropion to properly select a surgical intervention that addresses the underlying anatomical defect.
A thorough ocular history should be taken before physical examination. The surgeon should specifically ask about a history of facial palsy, previous periocular surgery, and prior facial trauma. Patients with long-standing blepharospasm or hemifacial spasm may have significant eyelid laxity from repeated mechanical pulling on the eyelids with their fingers in an attempt to open the eyes. Common symptoms reported by patients with ectropion include eye irritation and redness caused by ocular surface exposure and tearing as a result of reflex hypersecretion from corneal exposure, punctal malposition, or laxity-induced lacrimal pump dysfunction. With long-standing ectropion, the exposed palpebral conjunctiva may become keratinized, leading to symptoms of chronic redness, discharge, and bleeding.
When performing the ophthalmic examination, it is important to carefully assess eyelid laxity, eyelid margin appearance, medial and lateral canthal tendon integrity, orbicularis muscle tone, anterior and posterior lamellar characteristics, and lower-eyelid retractor anatomy ( Box 12.6.1 ).
Full ocular history
General ocular examination
Examination of specific eyelid changes
Eyelid laxity
Horizontal eyelid laxity
Medial canthal tendon laxity
Lateral canthal tendon laxity
Lacrimal puncta evaluation
Anterior lamellae inspection
Orbicularis muscle tone
Eyelid masses
Inferior eyelid retractor laxity
The lower eyelid naturally apposes the globe when the eye is open and throughout the entire blinking cycle. When pulled downward and released, a normal eyelid quickly recoils back to its normal position against the globe. In the presence of diminished tone or excessive laxity, the eyelid recoils slowly or requires the eye to blink one or more times to return to position. If needed, a measurement of laxity can be taken between the ocular surface and the downward-pulled eyelid (lower-eyelid distraction test). Normally, the eyelid cannot be distracted more than 6 mm from the ocular surface in younger individuals, 20–40 years of age, and more than 7.4 mm in older individuals aged 60–80 years ( Fig. 12.6.1 ).
Lateral traction is applied to the lower eyelid, and the total amount of inferior punctal displacement from the medial canthal angle is measured. A shift in inferior punctal position by more than 1–2 mm with traction indicates medial canthal laxity. Rarely, patients with marked dehiscence may require tendon repair, a procedure that is difficult because of the lacrimal drainage system. Disinsertion or rupture of the medial canthal tendon can result from previous trauma or medial canthal surgery.
The normal lateral canthal angle maintains an acute confluence that is positioned 1–2 mm medial to the lateral orbital rim. Laxity is present when the lateral canthus demonstrates medial displacement, rounding of the angle, or thinning of the canthal skin. Additionally, laxity is confirmed when eyelid traction in the medial direction displaces the lateral canthus nasally by more than 1–2 mm.
In the normal eyelid, puncta are not visible on passive external evaluation, and they are directed toward the ocular surface into the tear meniscus. Visualization of the puncta before eyelid distraction suggests medial eyelid ectropion. Chronic ectropion with punctal malposition can result in punctal stenosis or obliteration secondary to scarring.
Vertical shortening of the lower-eyelid anterior lamella (skin and orbicularis muscle) with eversion of the eyelid margin can result from actinic skin damage, facial trauma, and chronic eyelid malposition (involutional or paralytic), in addition to prior surgical procedures, including blepharoplasty. In mild cases, vertical tension lines in the eyelid skin can be visualized, and manual elevation of the cheek skin improves the ectropion by diminishing the downward tension. Limitation of superior migration of the eyelid margin in up gaze and eversion of the margin when opening the mouth widely also indicate a shortage of skin in the anterior lamella.
The resting orbicularis muscle tone allows the lower eyelid to remain well apposed to the ocular surface. Adequate muscle tone is also required for proper lacrimal pump function. Orbicularis muscle weakness is assessed during forced eyelid closure. Lagophthalmos results from the exaggerated horizontal eyelid laxity caused by orbicularis weakness. Additional signs of facial nerve palsy, including brow ptosis, diminished forehead rhytids, reduced nasolabial folds, and smile asymmetry, should be evaluated.
Eyelid masses, such as neoplasms or cysts, can physically displace the lower-eyelid margin as a result of both mass effect and the gravitational force on the mass shifting the eyelid margin down and away from the globe ( Fig. 12.6.2 ). It is important to thoroughly inspect the conjunctival surfaces and fornices in addition to a careful examination of the anterior lamellar tissue for any cicatricial changes caused by local neoplastic infiltration.

Inspection of the posterior lower eyelids allows visualization of the relationship between the tarsal plate and the lower-eyelid retractors. Laxity of the eyelid retractors may be associated with ectropion, especially in the setting of severe horizontal laxity. Profound retractor attenuation may lead to excessive conjunctival redundancy and poor definition of the inferior fornix.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here