Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The rate of ectopic pregnancy in the United States has remained fairly constant since the early 2000s and is approximately 6.6 in 1000 pregnancies in women aged 15 to 24.
Risks of ectopic pregnancy include age, smoking, pelvic inflammatory disease, infertility, and prior tubal surgery. After tubal sterilization, the risk of ectopic pregnancy if a pregnancy occurs is about 30%, reaching 50% if the sterilization technique was tubal desiccation.
Human chorionic gonadotropin (HCG) trends can help diagnose ectopic pregnancies. About 85% of women with an ectopic pregnancy have serum HCG levels lower than in normal pregnancy. In early pregnancy the normal HCG doubling time is 1.4 to 3 days, with 85% of pregnancies demonstrating a 66% HCG increase every 48 hours. An HCG rise less than 53% in 48 hours is 99% sensitive for an abnormal pregnancy.
Ectopic pregnancies can be managed surgically with salpingectomy or salpingostomy. Randomized trial data suggest there is no difference in overall subsequent pregnancy outcomes between women who are treated by salpingostomy versus salpingectomy.
Asymptomatic persistent ectopic pregnancy can be treated expectantly or with methotrexate (MTX). The success of MTX depends on the size and age of the gestation and the initial HCG level. After the methotrexate injection, the HCG level should fall at least 15% between days 4 and 7 and at least 15% weekly thereafter.
Ectopic pregnancy occurs when the fertilized ovum/developing blastocyst implants at a site outside the endometrial cavity. It was probably first described in the year 963 by Albucasis, an Arab writer. In 1876, before the initiation of surgical therapy, the mortality rate from ectopic pregnancy was estimated to be 60%. The first successful operative treatment of ectopic pregnancy was performed in 1883 by Lawson Tait in England. In 1887, he reported that he had performed salpingectomy on four women with ectopic pregnancy and that they all survived.
The incidence of ectopic pregnancy has been estimated to be between 1% to 2% of all pregnancies . Although the incidence of ectopic pregnancy increased sixfold between 1970 and 1992, it has remained stable since then. In the United States in 1989, the annual ectopic pregnancy rate per 10,000 women aged 15 to 44 was 15.5, similar to that in Finland but higher than the rate in France. The last national data reported by the Centers for Disease Control and Prevention (CDC) showed that the overall incidence of ectopic pregnancy had plateaued to approximately 20 in 1000 pregnancies in the early 1990s. The current incidence of ectopic pregnancy is difficult to estimate from available hospitalization and insurance records because the number of ectopic pregnancy cases requiring inpatient hospital treatment has decreased. The incidence varies among different countries, with rates as high as 1 in 28 and 1 in 40 pregnancies reported in Jamaica and Vietnam, respectively. The risk of ectopic pregnancy associated with assisted reproductive technology is increased compared with the general population, with rates from 0.8% to 8.6 %. Data from the National Assisted Reproductive Technology Surveillance System from 2001 to 2011 showed that the rate of ectopic pregnancy declined from 2% to 1.6% out of 553,577 pregnancies in the United States ( ).
There has been an increasing trend toward treating ectopic pregnancy conservatively (without resorting to salpingectomy) and on an ambulatory basis without overnight hospitalization. With earlier detection of ectopic pregnancy, a steadily increasing percentage of women with this problem are now being treated before tubal rupture occurs, by outpatient laparoscopic procedures or by medical treatment with methotrexate. An analysis of both hospital discharge data and an ambulatory medical care survey revealed that the estimated number of hospitalizations for ectopic pregnancy in the United States declined from nearly 90,000 in 1989 to about 45,000 in 1994. However, in 1992, about half of all women with ectopic pregnancy in the United States were treated as outpatients, and the estimated number of total ectopic pregnancies in this year was 108,000, for a rate of 19.7 per 1000 reported pregnancies. Thus in the United States in 1992, about 2 of every 100 women who were known to conceive had an ectopic gestation. The increased incidence of ectopic pregnancy is thought to be due to two factors: (1) the increased incidence of salpingitis, caused by increased infection with Chlamydia trachomatis or other sexually transmitted pathogens; and (2) improved diagnostic techniques, which enable the diagnosis of unruptured ectopic pregnancy with more precision and earlier in gestation, before asymptomatic resolution of the pregnancy occurs.
The rate of ectopic pregnancy increases with increasing age . However, because of the lower pregnancy rate in older women, overall only about 11% of ectopic pregnancies in the United States occur in women aged 35 to 44, whereas more than half, 58%, occur in women aged 25 to 34 years. Most ectopic pregnancies occur in multigravid women. Only 10% to 15% of ectopic pregnancies occur in nulligravid women, whereas more than half occur in women who have been pregnant three or more times. In the United States, the rates of ectopic pregnancy are similar in each section of the country, but the rates are higher for nonwhite women compared with white women. About 3% of all reported pregnancies in nonwhite women aged 35 to 44 in the United States are ectopic.
Even with the increased use of surgery and blood transfusions and earlier diagnosis , ectopic pregnancy remains a major cause of maternal death in the United States today. From the last CDC report , 6% of pregnancy-related mortality during the period of 1991 to 1999 was due to ectopic pregnancies . In the United States, 876 deaths were attributed to ectopic pregnancy between 1980 and 2007. Ectopic pregnancy is the most common cause of maternal death in the first half of pregnancy. The ectopic pregnancy–to–mortality ratio has declined by 57% from the period 1980 to 1984 to 2003 to 2007, from 1.15 to 0.5 ( ). The mortality ratio was 6.8 times higher for African American women than for white women and 3.5 times higher for women older than 35 years compared with women younger than 25 years. Of the 76 deaths among women hospitalized with ectopic pregnancy between 1998 and 2007, 70% of the ectopic pregnancies were located in the fallopian tubes. Unmarried women of all races have a 1.7 times greater chance of dying of ectopic pregnancy than married women. Overall the risk of death from ectopic pregnancy is about 10 times greater than the risk of childbirth and more than 50 times greater than the risk of legal abortion.
The major cause of mortality from ectopic pregnancy is blood loss. Most cases of mortality (70%) result from gestations in the tube, and the other 30% are interstitial cornual or abdominal gestations. Because the overall incidence of ectopic pregnancy occurring in these latter locations is slightly less than 4%, interstitial and abdominal ectopic pregnancies have about a five times greater risk of being fatal. About three-fourths of the women with fatal ectopic pregnancies initially developed symptoms and died in the first 12 weeks of gestation. Of the remaining one-fourth who developed symptoms and died after the first-trimester, 70% had interstitial or abdominal pregnancies. Patient delay in consulting a physician after development of symptoms accounted for one-third of the deaths, whereas treatment delay resulting from misdiagnosis contributed to the half the deaths.
The major factor contributing to the risk of ectopic pregnancy is salpingitis. Salpingitis results from infectious causes such as pelvic inflammatory disease (PID) or inflammatory causes such as endometriosis. Its morphologic sequelae account for about half of the initial episodes of ectopic pregnancy. However, in about 40% of cases the cause cannot be determined and is presumed to be a physiologic disorder resulting from the delay of passage of the embryo into the uterine cavity. Ovulation from the contralateral ovary has been implicated as a cause of the delay of blastocyst transport, and it has been suggested that contralateral ovulation occurs in about one-third of tubal pregnancies, although this has not been confirmed.
Another possibility in the etiology of ectopic pregnancy is a hormonal imbalance; an elevated circulating level of either estrogen or progesterone can alter normal tubal contractility. An increased rate of ectopic pregnancies has been reported in women who conceive with physiologically and pharmacologically elevated levels of progestogens . The latter condition can be produced locally with a progestogen-releasing intrauterine device (IUD) and systemically with progestin-only oral contraceptives. Iatrogenic, physiologically increased levels of estrogen and progesterone occur after ovulation induction and the use of assisted reproductive technology (ART) with either clomiphene citrate or human menopausal gonadotropins, and an increased rate of ectopic pregnancies has been reported in women conceiving after each of these treatment modalities.
Another possible cause is an abnormality of embryonic development. Although aneuploidy has been found to be prevalent in ectopic pregnancies, it may not be higher than the normal rate of aneuploidy and is unlikely to be a cause of ectopic pregnancies. Inherited genetic abnormalities most probably are not a cause of ectopic pregnancy either. Also, there is no increased incidence of ectopic pregnancy among first-degree relatives.
Several epidemiologic studies have indicated that cigarette smoking is associated with about a twofold increased risk of ectopic pregnancy, even when the data were controlled for the presence of other risk factors. The risk of ectopic pregnancy was directly related to the number of cigarettes smoked per day, with a fourfold increased risk noted among women who smoked 30 or more cigarettes per day. Known risk factors for ectopic pregnancy, presented as odds ratios and attributable risk, are depicted in Table 17.1 ( ).
| Odds Ratio | Attributable Risk * | |
|---|---|---|
| Probable salpingitis | 2 | |
| Confirmed salpingitis | 3.5 | |
| History of tubal surgery | 3.5 | 0.18 † |
| Smoking | 0.35 | |
| Ex-smoker | 1.5 | |
| 1-9 cigarettes per day | 2 | |
| 10-19 cigarettes per day | 3 | |
| ≥20 cigarettes per day | 4 | |
| Age (years) | 0.14 | |
| 30-39 | 1.5 | |
| ≥40 | 3 | |
| Spontaneous abortion | 3 | 0.07 |
| Elective abortion | 2 | 0.03 |
| IUD history | 1.5 | 0.05 |
| Previous infertility | 2.5 | 0.18 |
* From Auvergne registry data (Bouyer J, Coste J, Shojaei T, et al. Risk factors for ectopic pregnancy: a comprehensive analysis based on a large case-control, population-based study in France. Am J Epidemiol. 2003;157:185).
† Risk attributable to history of genital infection and tubal surgery together is 0.33.
The major causes of ectopic pregnancy are discussed in more detail next.
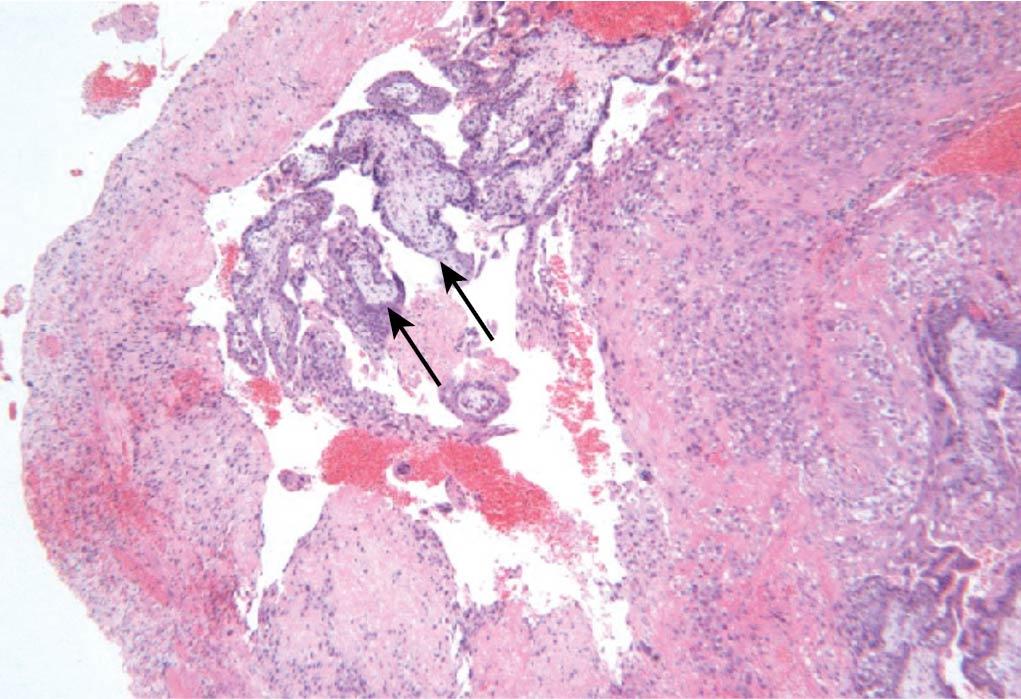
Disruption of normal tubal anatomy from infection, surgery, congenital anomalies, or inflammatory disease such as endometriosis is a major cause of ectopic pregnancy. The agglutination of the plicae (folds) of the endosalpinx produced by salpingitis can allow passage of sperm but prevent the normal transport of the larger morula. The morula can be trapped in blind pockets formed by adhesions of the endosalpinx. In their 20-year longitudinal study, Weström and colleagues found that nearly half (45.3%) of the women with ectopic pregnancy had a clinical history or histologic findings of a prior episode of acute salpingitis ( ). This is in agreement with the 40% incidence of prior salpingitis found on histologic examination by several groups of investigators in women with ectopic pregnancy ( Fig. 17.1 ).
Weström and colleagues prospectively followed 900 women aged 15 to 34 years who had laparoscopically confirmed acute salpingitis and found that the subsequent ectopic pregnancy rate was 68.8 per 1000 conceptions, yielding a sixfold increase in the risk of ectopic pregnancy . The risk of ectopic pregnancy after acute salpingitis increased both with the number of episodes of infection and with the increasing age of the women at the time of infection. The odds ratios for ectopic pregnancy after two and after three or more episodes of chlamydial infection were 2.1 and 4.5, respectively. Data also suggest that a history of chlamydial infection results in the production of PROKR2 protein, which creates a microenvironment that predisposes to tubal implantation.
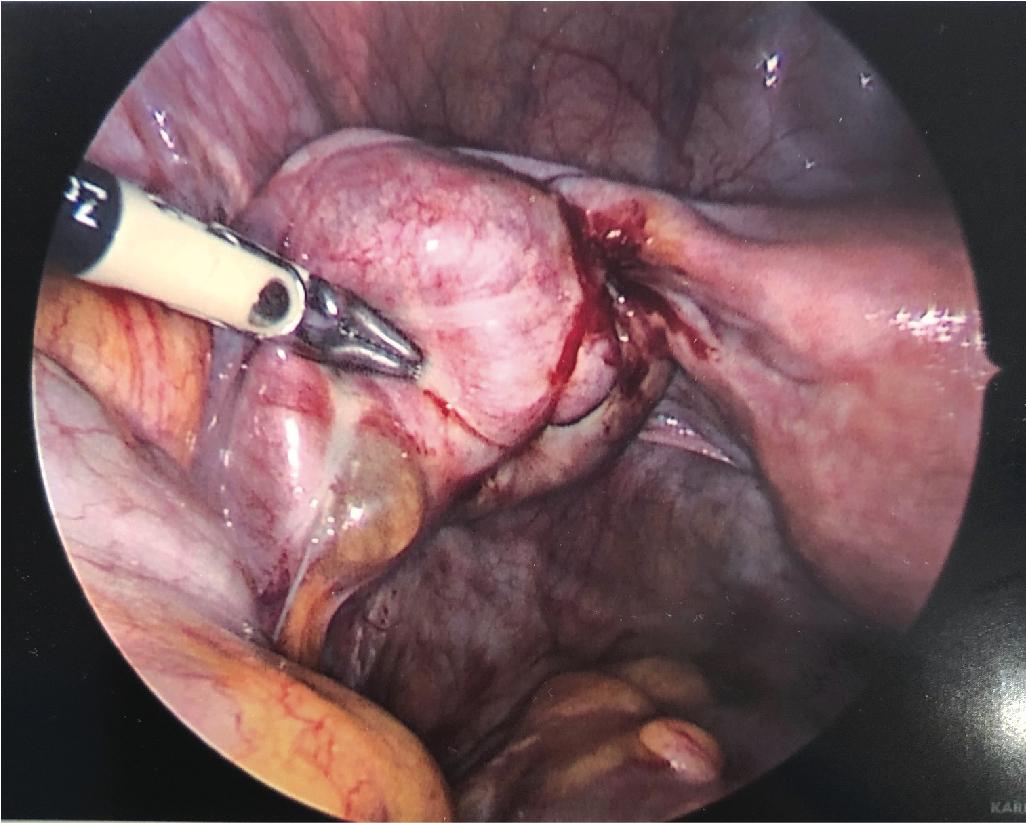
Inflammation and adhesions of the fallopian tubes as a result of conditions such as endometriosis are risk factors for ectopic pregnancy. Fig. 17.2 portrays an example of endometriosis resulting in a left ovarian endometrioma, tubal inflammation, and adhesions, with subsequent clubbed tube and hydrosalpinx. Compared with women without endometriosis, women with endometriosis had two times the risk for ectopic pregnancy (relative risk, 1.9; 95% confidence interval [CI], 1.8 to 2.1) ( ).
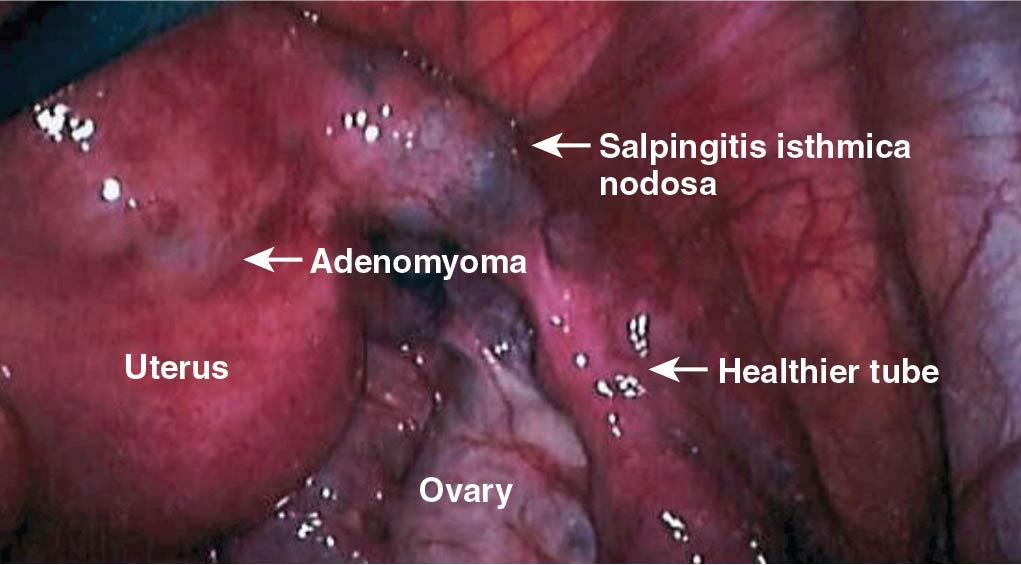
Salpingitis isthmica nodosa (SIN) is defined as the microscopic presence of tubal epithelium within the myosalpinx or beneath the tubal serosa ( Fig. 17.3 ). In two histopathologic studies of tubes removed from women with ectopic pregnancy, it was found that about half contained lesions of SIN compared with 5% in a control group. With serial sectioning, it has been determined that SIN is actually a diverticulum or intrauterine extension of the tubal lumen . Associated histologic evidence of chronic salpingitis was seen in only 6% of the tubes, suggesting that SIN was not necessarily the result of infection . The tubal pregnancy has been found to have usually implanted in a portion of the tube distal to the SIN, indicating that mechanical entrapment of the morula is not the mechanism whereby SIN causes tubal gestation. It is possible that SIN itself or the associated tubal anomalies may be responsible for dysfunction of the tubal transport mechanism without anatomic obstruction.
It is likely that adhesions between the tubal serosa and bowel or peritoneum may interfere with normal tubal motility and cause ectopic pregnancy because, as reported, 17% to 27% of women with ectopic pregnancy have had previous abdominal surgical procedures not involving the oviduct. On the other hand, neither endometriosis nor congenital anomalies of the tube have been associated with an increased incidence of ectopic pregnancy.
An operative procedure on the tube itself is a cause of ectopic pregnancy whether the tube is morphologically normal, as occurs with sterilization procedures, or abnormal, as occurs with post salpingitis reconstructive surgery. The incidence of ectopic pregnancy occurring after salpingoplasty or salpingostomy procedures to treat distal tubal disease ranges from 15% to 25%, probably because the damage to the endosalpinx remains. The rate of ectopic pregnancy after reversal of sterilization procedures is lower, about 4%, because the tubes have not been damaged by infection. The rate of ectopic pregnancy after sterilization is discussed later in this chapter.
Women who have had a prior ectopic pregnancy, even if treated medically or by unilateral salpingectomy, are at increased risk for having a subsequent ectopic pregnancy. The odds of a recurrent ectopic pregnancy among women with history of ectopic pregnancy compared with other pregnant women is almost threefold greater (adjusted odds ratio [AOR], 2.72; 95% CI 1.66 to 2.8) ( ). Of women who conceive after having one ectopic pregnancy, about 25% of subsequent pregnancies are ectopic . The rates of recurrent ectopic pregnancy after single-dose methotrexate treatment, salpingectomy, and linear salpingostomy are 8%, 9.8%, and 15.4%, respectively, among women who conceive ( ).
Although it is less commonly encountered today, the incidence of ectopic gestation is significantly greater (four to five times) in women who have been exposed to diethylstilbestrol (DES) in utero and has been reported at the rate of 4% to 5%. This is likely because of abnormal tubal morphology and impaired function of the fimbriae. In women exposed to DES whose hysterosalpingograms demonstrated abnormalities in the uterine cavity, the ectopic pregnancy rate was as high as 13%.
For several decades, sterilization has been the most popular method of contraception used by couples in the United States. Since the development of laparoscopic surgery, female tubal sterilization is performed about twice as often as vasectomy. In an analysis of the long-term risk of pregnancy after tubal sterilization reported by Peterson and coworkers, it was found that within 10 years after the procedure, the cumulative life table probability of pregnancy was 1.85% . The 10-year failure rate after bipolar electrosurgical sterilization of the tubes was 2.48%, which rose to 5.43% if the sterilization procedure was performed when the woman was younger than 28 years. These investigators reported that for all 143 pregnancies occurring after tubal sterilization, 43 (30.1%) were ectopic pregnancies ( ).
Several investigators have reported that if pregnancy occurred after tubal sterilization with electrosurgical devices (monopolar or bipolar instruments), the ectopic pregnancy rate was as high as 50%. It has been hypothesized that fistulas may develop, allowing sperm to pass into the distal segment of the oviduct and fertilize the egg ( Fig. 17.4 ) ( ). Such fistulas can be demonstrated radiographically in about 11% of women after laparoscopic electrosurgical sterilization. Peterson and colleagues reported that within 10 years after the sterilization procedure, women sterilized with bipolar devices had twice as many ectopic pregnancies compared with those sterilized with metal clips or silicone bands. The overall ectopic pregnancy rate after bipolar sterilization was 1.7%.
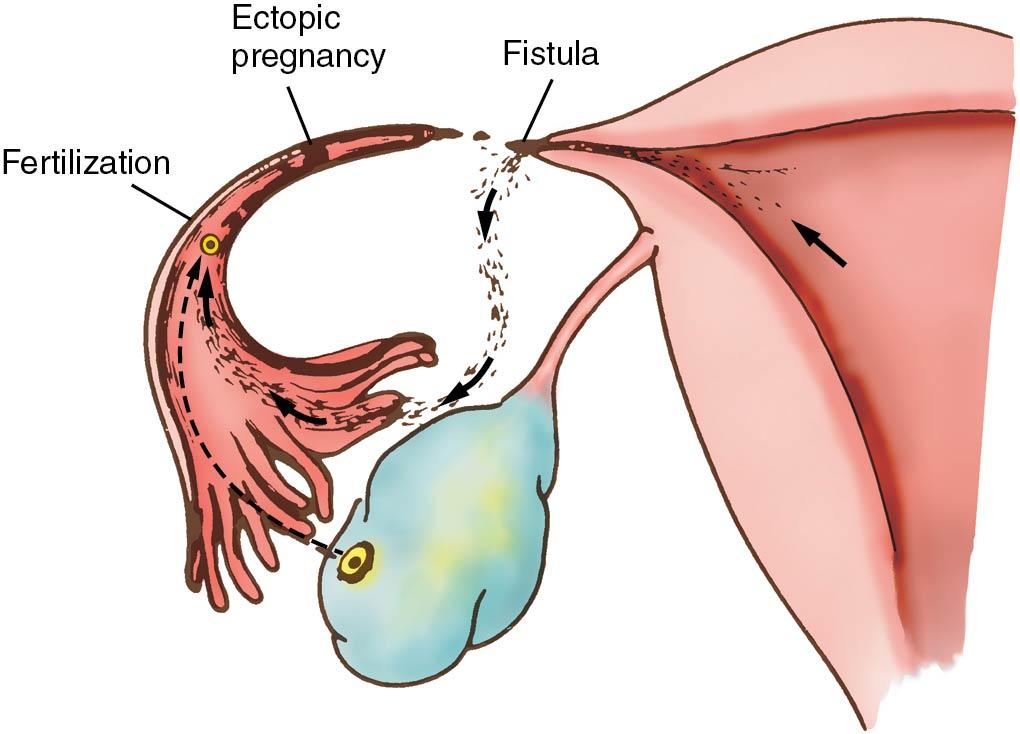
Because about one-third of pregnancies that occur after all tubal sterilizations are ectopic, women should be counseled that if they do not experience the expected menses at any time after tubal sterilization before menopause, a test to detect human chorionic gonadotropin (HCG) should be performed rapidly, and if they are pregnant, a diagnostic evaluation to exclude the presence of ectopic pregnancy is necessary. In women who have an ectopic pregnancy after sterilization with the use of electrosurgery, because the site of the fistula usually cannot be determined clinically, salpingectomies should be carried out.
More often tubal sterilizations are now completed with bilateral salpingectomies. Compared with bipolar electrosurgical sterilization, in which a portion of the tube is desiccated, bilateral salpingectomies offer complete removal of the fallopian tube. This offers several advantages, including reduced risk of posttubal fistula formation, diminished risk of tubal stump ectopic pregnancy, decreased risk of poststerilization hydrosalpinx. and opportunistic salpingectomies, which decrease one’s lifetime risk of ovarian cancer ( ).
In general, individuals using contraception have a lower incidence of ectopic pregnancy compared with those not using contraception because the likelihood of conceiving is lower. Among contraceptive failures, women using diaphragms or combination oral contraceptives do not have an increased risk of ectopic pregnancy, whereas contraceptive failures with the IUD lead to an increased risk of ectopic pregnancy. Among IUD contraceptive failures, the risk of ectopic pregnancy is approximately 6% for the copper IUD versus 50% for the levonorgestrel IUD ( ) . This is because the progestogen-releasing IUD inhibits tubal contractions, resulting in a higher ectopic rate than the copper IUD. Women who use this method of contraception have about twice the risk of ectopic pregnancy (7.5 per 1000 woman-years) if they conceive compared with women who use no method of contraception (3.5 per 1000 woman-years). Women using IUDs who elect to have their pregnancies terminated should have a histologic examination of the tissue removed from the uterine cavity to be certain the pregnancy was intrauterine.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here